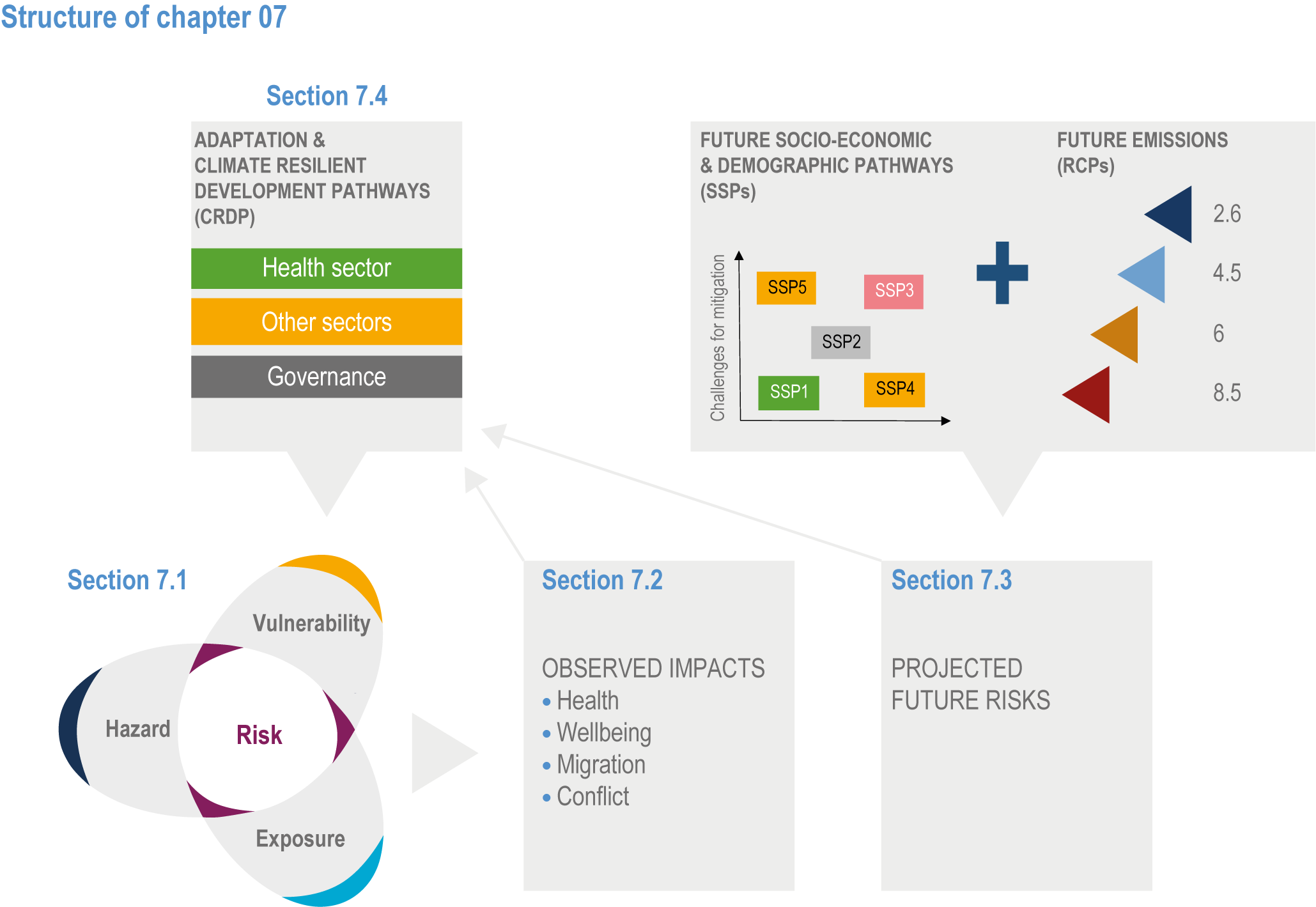
Chapter 7: Health, Wellbeing and the Changing Structure of Communities
Executive Summary
Climate-related illnesses, premature deaths, malnutrition in all its forms, and threats to mental health and well-being are increasing (very high confidence1 ). Climate hazards are a growing driver of involuntary migration and displacement (high confidence) and are a contributing factor to violent conflict (high confidence). These impacts are often inter-connected, are unevenly distributed across and within societies, and will continue to be experienced inequitably due to differences in exposure and vulnerability (very high confidence). Cascading and compounding risks affecting health due to extreme weather events have been observed in all inhabited regions, and risks are expected to increase with further warming (very high confidence) {7.1.3, 7.1.4; Cross-Chapter Box COVID in Chapter 7; 7.2.1, 7.2.2, 7.2.3, 7.2.4, 7.3.1, 7.3.2, 7.3.3, 7.4.1, 7.4.4; Cross-Chapter Box HEALTH in Chapter 7; Cross-Chapter Box ILLNESS in Chapter 2}.
Since AR5, new evidence and awareness of current impacts and projected risks of climate change on health, well-being, migration and conflict have emerged, including greater evidence of the detrimental impacts of climate change on mental health (very high confidence). New international agreements were reached on climate change (Paris Agreement), disaster risk reduction (DRR) (Sendai Agreement), sustainable development (the Sustainable Development Goals (SDGs)), urbanisation (The New Urban Agenda), migration (Global Compact for Safe, Orderly and Regular Migration) and refugees (Global Compact on Refugees) that, if achieved, would reduce the impacts of climate change on health, well-being, migration and conflict (very high confidence). However, the challenges with implementing these agreements are highlighted by the coronavirus disease 2019 (COVID-19) pandemic, which exposed systemic weaknesses at community, national and international levels in the ability of societies to anticipate and respond to global risks (high confidence). Incremental changes in policies and strategies have proven insufficient to reduce climate-related risks to health, well-being, migration and conflict, highlighting the value of more integrated approaches and frameworks for solutions across systems and sectors that are embodied in these new international agreements (high confidence) {7.1.3, 7.2.1, 7.4.1, 7.4.2, 7.4.3, 7.4.6; Cross-Chapter Box COVID in Chapter 7}.
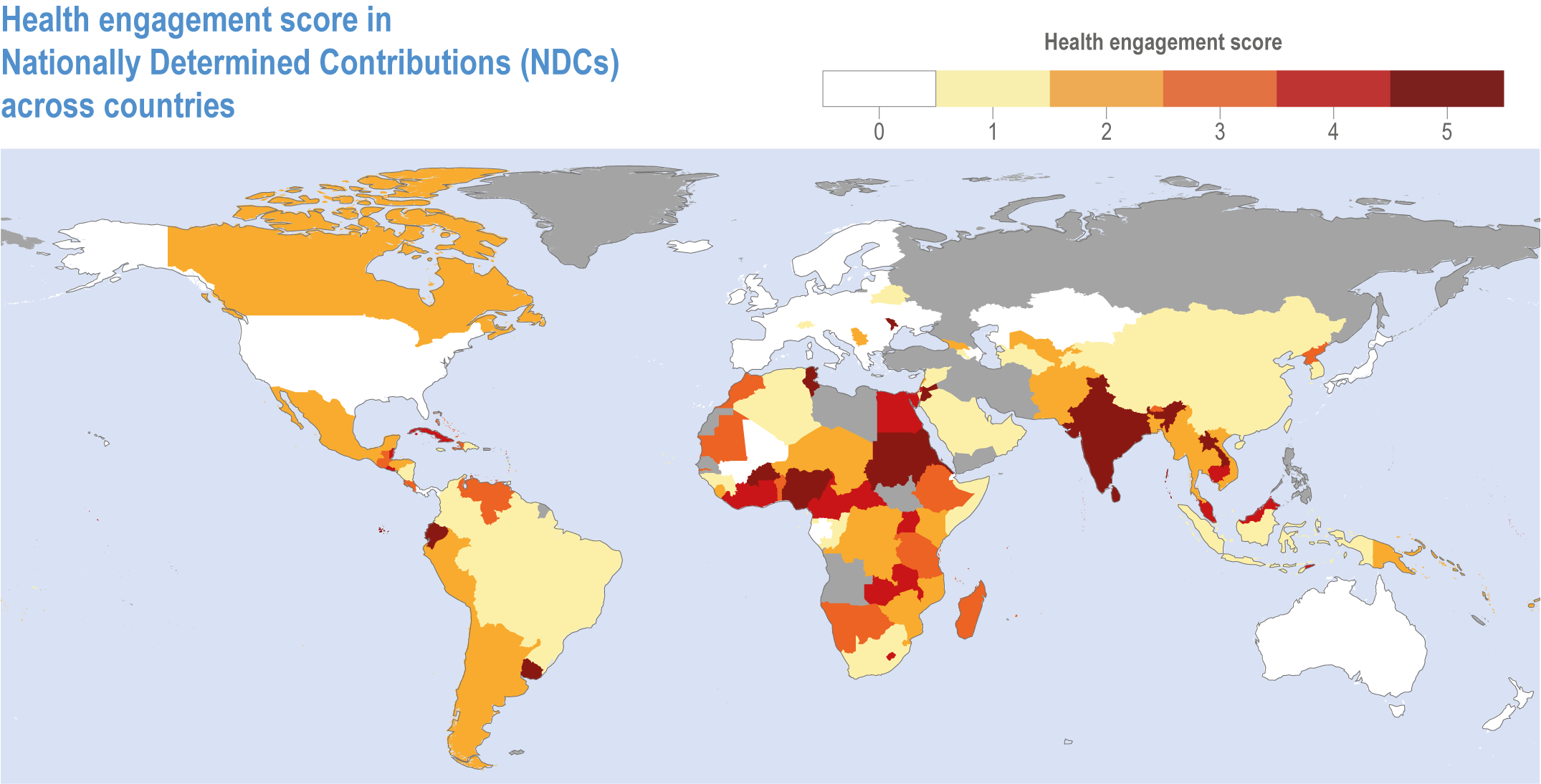
With proactive, timely and effective adaptation, many risks for human health and well-being could be reduced and some potentially avoided (very high confidence). A significant adaptation gap exists for human health and well-being and for responses to disaster risks (very high confidence). Nationally Determined Contributions (NDCs) to the Paris Agreement from low- and middle-income countries identify health as a priority concern. National planning on health and climate change is advancing, but the comprehensiveness of strategies and plans need to be strengthened, and implementing action on key health and climate change priorities remains challenging (high confidence). Multi-sectoral collaboration on health and climate change policy is evident, with uneven progress, and financial support for health adaptation is only 0.5% of dispersed multi-lateral climate finance projects (high confidence). This level of investment is insufficient to protect population health and health systems from most climate-sensitive health risks (very high confidence) {7.4.1, 7.4.2, 7.4.3}.
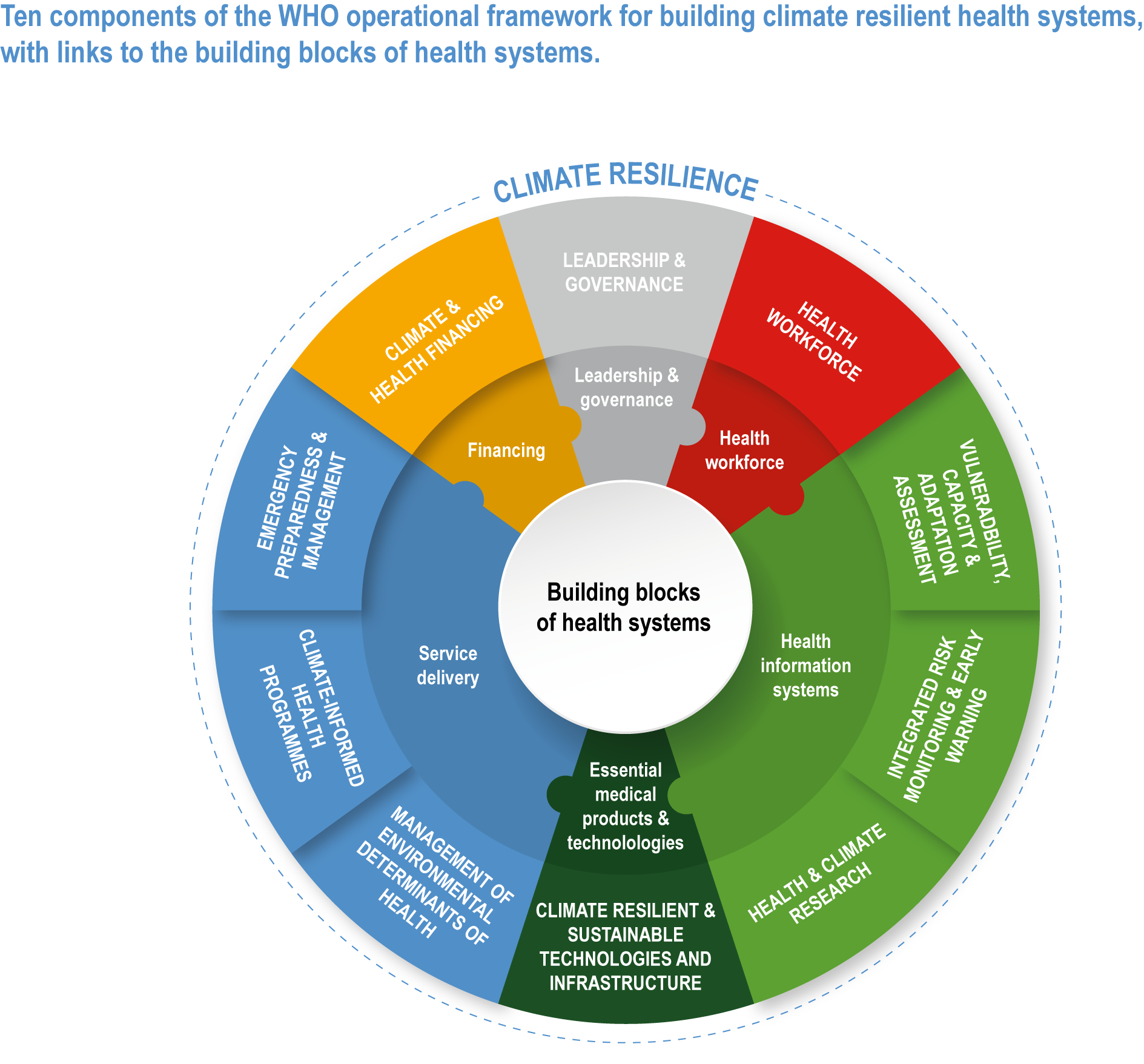
Climate resilient development has a strong potential to generate substantial co-benefits for health and well-being and to reduce risks of involuntary displacement and conflict (very high confidence). Sustainable and climate resilient development that decreases exposure, vulnerability and societal inequity and that increases timely and effective adaptation and mitigation more broadly, has the potential to reduce but not necessarily eliminate climate change impacts on health, well-being, involuntary migration and conflict (high confidence). This development includes greenhouse gas (GHG) emission reductions through clean energy and transport; climate-resilient urban planning; sustainable food systems that lead to healthier diets; universal access to healthcare and social protection systems; wide-scale, proactive adaptive capacity building for climate change; and achievement of the SDGs (very high confidence). Meeting the objectives of the Global Compact for Safe, Orderly, and Regular Migration and building inclusive and integrative approaches to climate-resilient peace would help prevent health risks related to migration and conflict (high agreement, medium evidence). The net global financial gains from these co-benefits to health and well-being, including avoided hospitalisations, morbidity and premature deaths, exceed the financial costs of mitigation (high confidence). As an example of co-benefits, the financial value of health benefits from improved air quality alone is projected to be greater than the costs of meeting the goals of the Paris Agreement (high confidence). All pathways to climate resilient development, including those for the health and healthcare systems, involve balancing complex synergies and trade-offs between development pathways and the options that underpin climate mitigation and adaptation pathways (very high confidence) {7.4.6; Cross-Chapter Box HEALTH in Chapter 7; Cross-Chapter Box MIGRATE in Chapter 7}.
Key transformations are needed to facilitate climate resilient development pathways (CRDPs) for health, well-being, migration and conflict avoidance (high confidence). The transformational changes will be more effective if they are responsive to regional, local and Indigenous knowledge and consider the many dimensions of vulnerability, including those that are gender- and age-specific (high confidence) . A key pathway towards climate resilience in the health sector is universal access to primary healthcare, including mental healthcare (high confidence). Investments in other sectors and systems that improve upon the social determinants of health have the potential to reduce vulnerability to climate-related health risks (high confidence). Links between climate risks, adaptation, migration and labour markets highlight the value of providing better mobility options as part of transformative change (medium confidence). Strong governance and gender-sensitive approaches to natural resource management can reduce the risk of inter-group conflict in climate-disrupted areas (medium confidence) {7.4.6; Cross-Chapter Box COVID in Chapter 7; Cross-Chapter Box HEALTH in Chapter 7; Cross-Chapter Box GENDER in Chapter 18; Cross-Chapter Box INDIG in Chapter 18; Cross-Chapter Box MIGRATE in Chapter 7}.
Observed Impacts
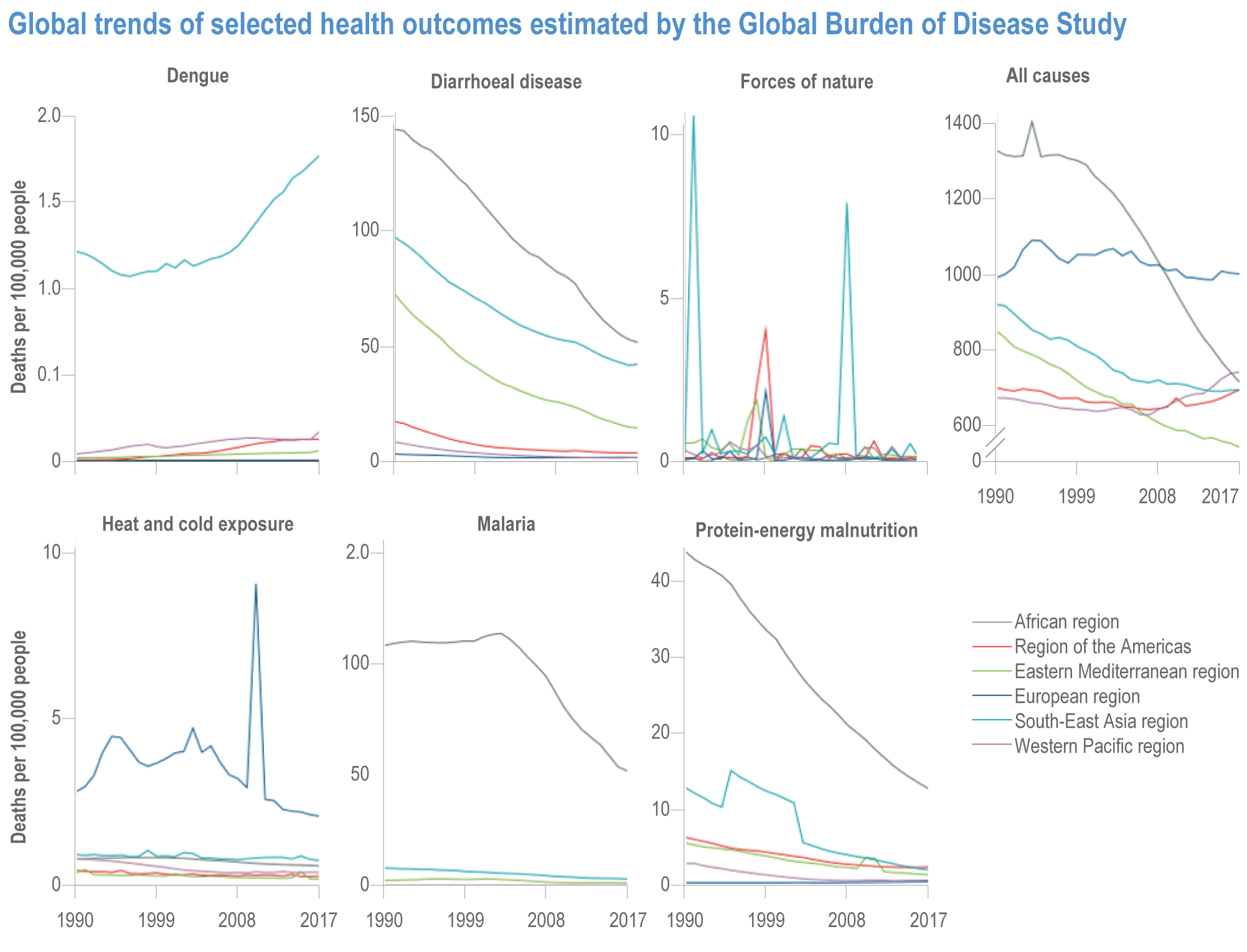
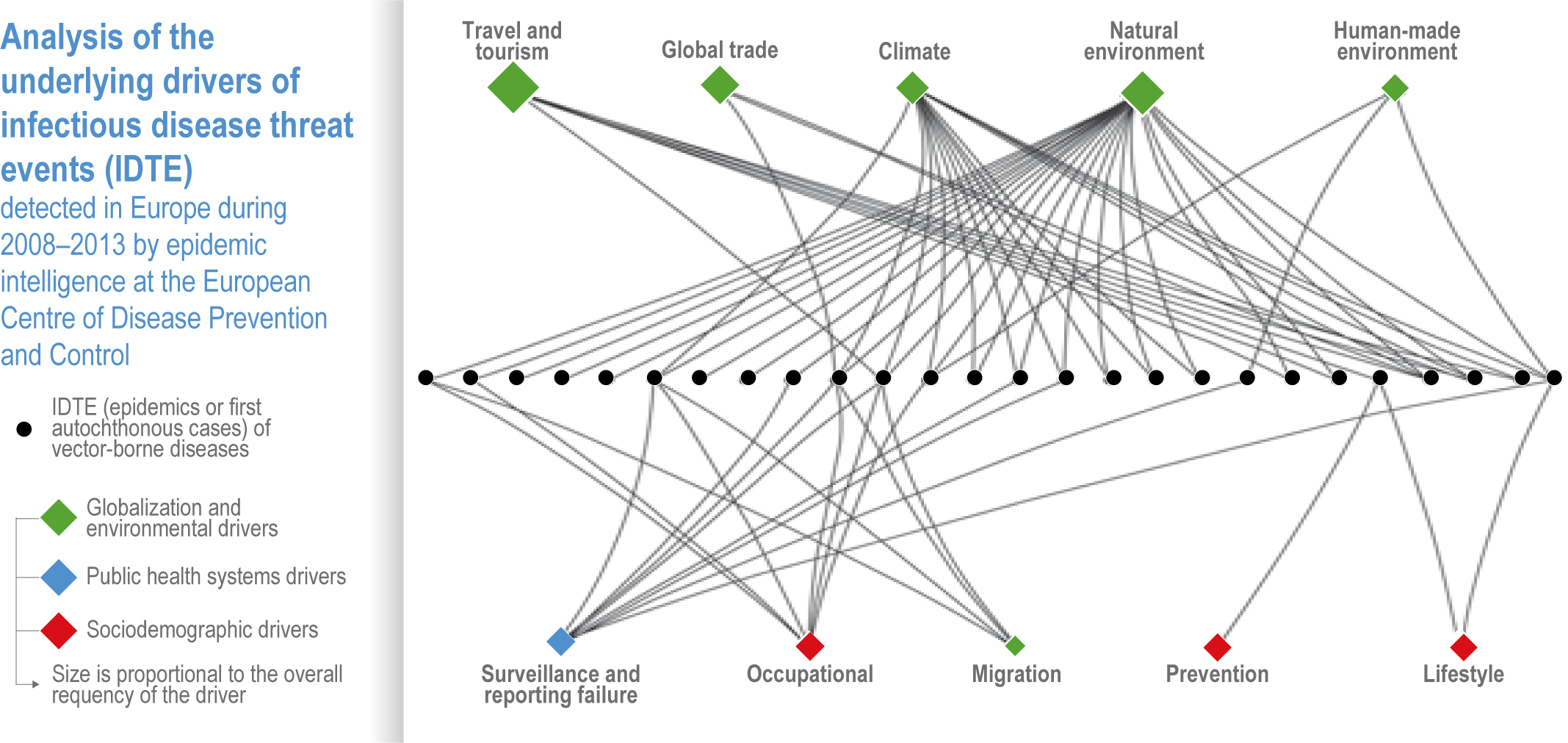
Climate hazards are increasingly contributing to a growing number of adverse health outcomes (including communicable and non-communicable diseases (NCDs)) in multiple geographical areas (very high confidence) . The net impacts are largely negative at all scales (very high confidence), and there are very few examples of beneficial outcomes from climate change at any scale (high confidence). While malaria incidence has declined globally due to non-climatic socioeconomic factors and health system responses, a shift to higher altitudes has been observed as the climate warms (very high confidence). Climate variability and change (including temperature, relative humidity and rainfall) and population mobility are significantly and positively associated with observed increases in dengue globally; chikungunya virus in Asia, Latin America, North America and Europe (high confidence) ; Lyme disease vector Ixodes scapularis in North America (high confidence) ; and Lyme disease and tick-borne encephalitis vector Ixodes ricinus in Europe (medium confidence). Higher temperatures (very high confidence), heavy rainfall events (high confidence) and flooding (medium confidence) are associated with an increase of diarrhoeal diseases in affected regions, including cholera (very high confidence) , other gastrointestinal infections (high confidence) and food-borne diseases due to Salmonella and Campylobacter (medium confidence). Floods have led to increases in vector- and waterborne diseases and to disturbances of public health services (high confidence). Climate extremes increase the risks of several types of respiratory tract infections (high confidence). Climate-related extreme events such as wildfires, storms and floods are followed by increased rates of mental illness in exposed populations (very high confidence) {7.2.1, 7.2.2, 7.2.3, 7.2.4, 7.2.5, 7.2.6}.
Several chronic, non-communicable respiratory diseases are climate-sensitive based on their exposure pathways (e.g., heat, cold, dust, small particulates, ozone, fire smoke and allergens) (high confidence), although climate change is not the dominant driver in all cases. Worldwide, rates of adverse health impacts associated with small particulate matter (PM) exposure have decreased steadily due to decreasing primary emissions (very high confidence) , while rates of adverse health impacts from ozone air pollution exposure have increased (very high confidence). Exposure to wildland fires and associated smoke has increased in several regions (very high confidence). Spring pollen season start dates in northern mid-latitudes are occurring earlier due to climate change, increasing the risks of allergic respiratory diseases (high confidence) {7.2.3.2}.
Heat is a growing health risk due to burgeoning urbanisation, an increase in high temperature extremes and demographic changes in countries with aging populations (very high confidence). Potential hours of work lost due to heat has increased significantly over the past two decades (high confidence). Some regions are already experiencing heat stress conditions at or approaching the upper limits of labour productivity (high confidence). A significant proportion of warm-season heat-related mortality in temperate regions is linked to observed anthropogenic climate change (medium confidence) but greater evidence is required for tropical regions. For some heatwave events over the last two decades, associated health impacts can be at least partially attributed to observed climate change (high confidence). Extreme heat has negative impacts on mental health, well-being, life satisfaction, happiness, cognitive performance and aggression (medium confidence) {7.2.4.1, 7.2.4.5}.
Climate variability and change contribute to food insecurity, which can lead to malnutrition, including undernutrition, overweight and obesity, and to disease susceptibility in low- and middle-income countries (high confidence). Populations exposed to extreme weather and climate events may consume inadequate or insufficient food, leading to malnutrition and increasing the risk of disease (high confidence). Children and pregnant women experience disproportionately greater adverse nutrition and health impacts (high confidence). Climatic influences on nutrition are strongly mediated by socioeconomic factors (very high confidence) {7.2.4.4, 7.3.1}.
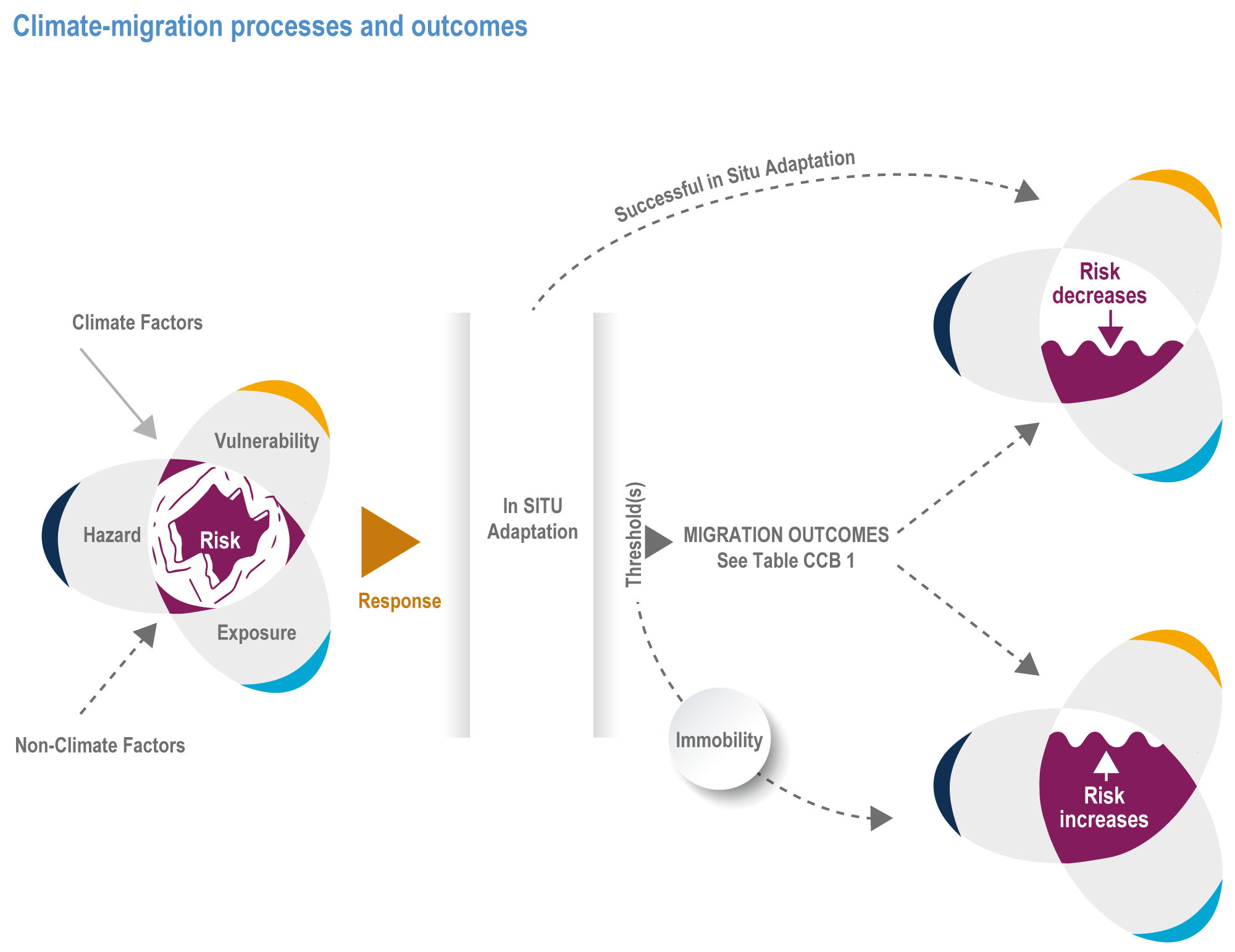
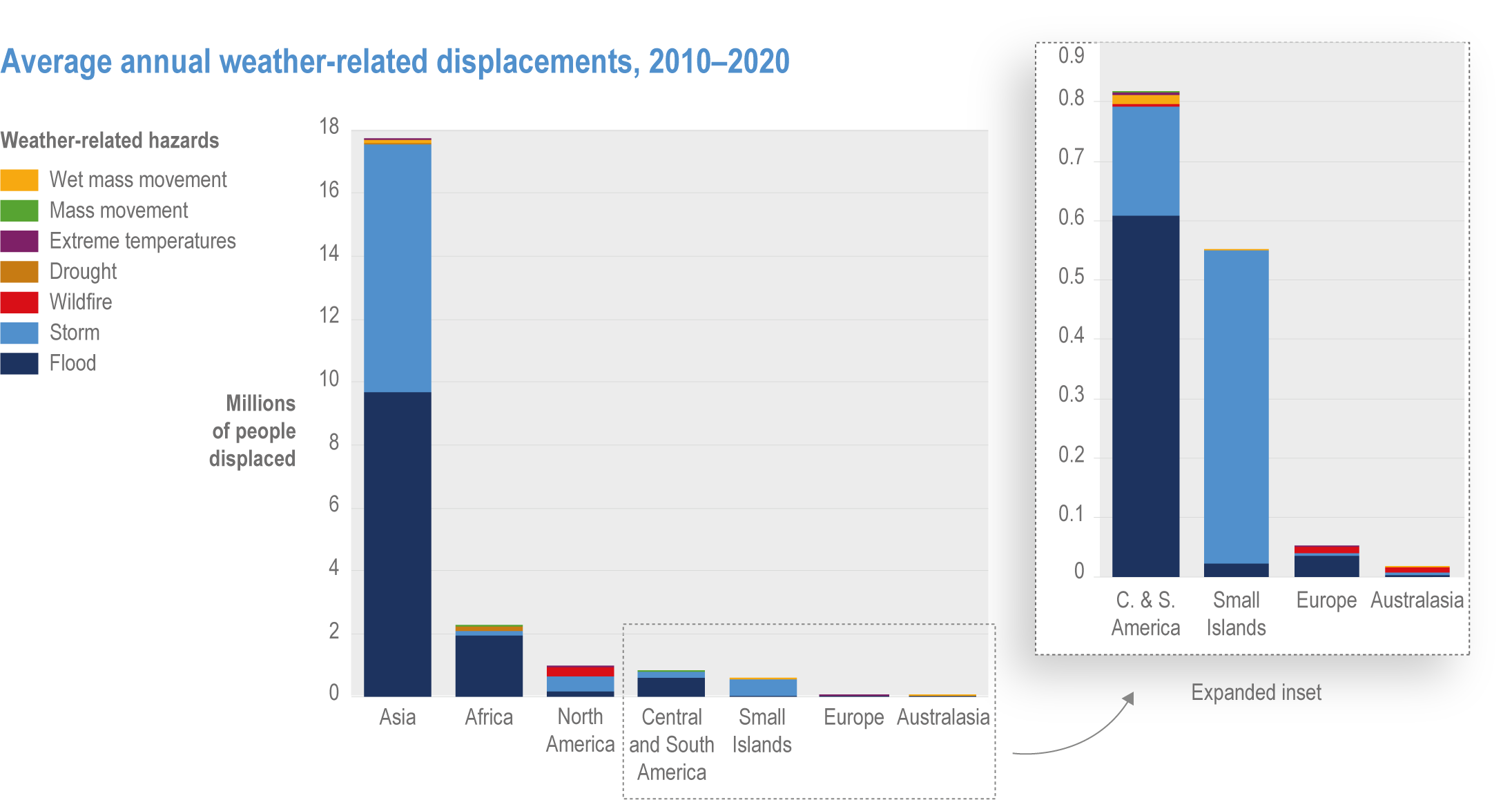
Extreme climate events act as both direct drivers (e.g., destruction of homes by tropical cyclones) and as indirect drivers (e.g., rural income losses during prolonged droughts) of involuntary migration and displacement (very high confidence). Most documented examples of climate-related displacement occur within national boundaries, with international movements occurring primarily within regions, particularly between countries with contiguous borders (high confidence). Global statistics collected since 2008 by the Internal Displacement Monitoring Centre (IDMC) show an annual average of over 20 million people internally displaced by weather-related extreme events, with storms and floods the most common drivers (high confidence). The largest absolute number of people displaced by extreme weather each year occurs in Asia (South, Southeast and East), followed by sub-Saharan Africa, but small island states in the Caribbean and South Pacific are disproportionately affected relative to their small population size (high confidence). Immobility in the context of climate risks can reflect vulnerability and lack of agency but can also be a deliberate choice of people to maintain livelihoods, economic considerations and social and cultural attachments to place (high confidence) {7.2.6; Cross-Chapter Box MIGRATE in Chapter 7}.
Climate hazards have affected armed conflict within countries (medium confidence), but the influence of climate is small compared to socioeconomic, political and cultural factors (high confidence). Climate increases conflict risk by undermining food and water security, income and livelihoods in situations where there are large populations, weather-sensitive economic activities, weak institutions and high levels of poverty and inequality (high confidence). In urban areas, food and water insecurity and inequitable access to services has been associated with civil unrest where there are weak institutions (medium confidence). Climate hazards are associated with increased violence against women, girls and vulnerable groups, and the experience of armed conflict is gendered (medium confidence). Adaptation and mitigation projects implemented without consideration of local social dynamics have exacerbated non-violent conflict (medium confidence) {7.2.7}.
Projected Risks and Vulnerabilities
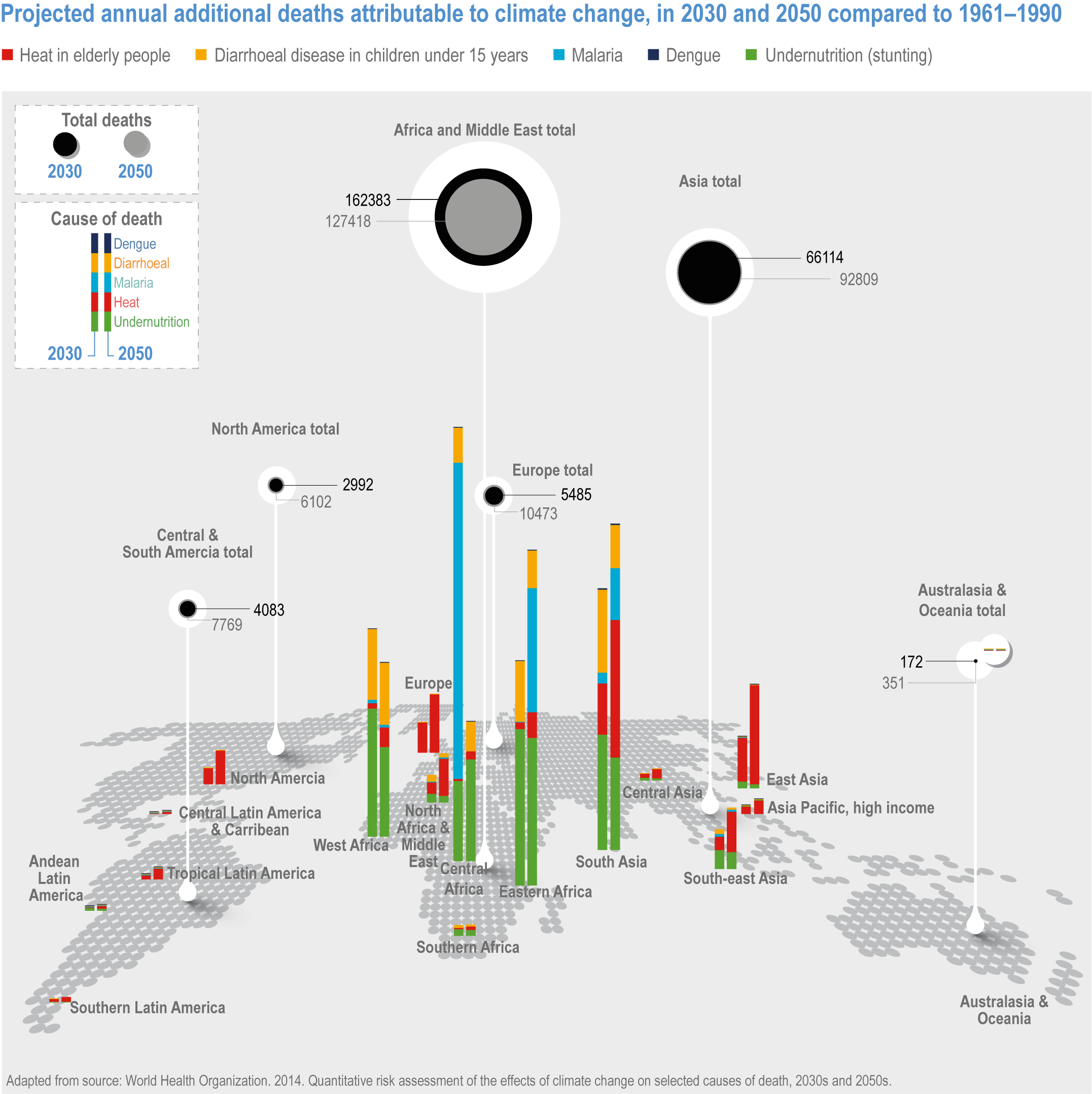
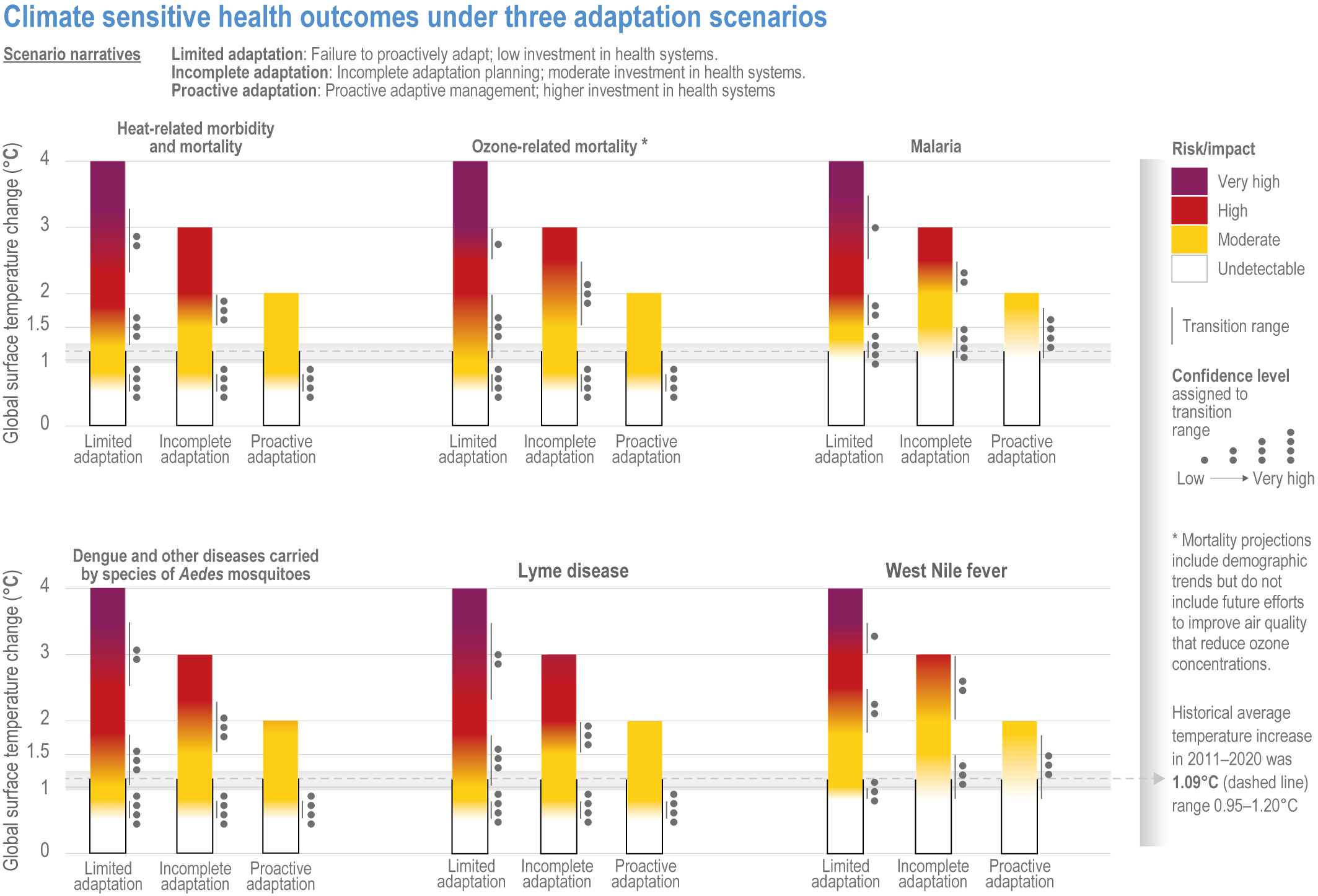
A significant increase in ill health and premature deaths from climate-sensitive diseases and conditions is projected due to climate change (high confidence) . An excess of 250,000 deaths yr –1 by 2050 attributable to climate change is projected due to heat, undernutrition, malaria and diarrhoeal disease, with more than half of this excess mortality projected for Africa (compared to a 1961–1991 baseline period for a mid-range emissions scenario) (high confidence). Risks for heat-related morbidity and mortality, ozone-related mortality, malaria, diseases carried by Aedes sp. mosquitoes, Lyme disease and West Nile fever, as well as the temperatures at which risk transitions occur (i.e. from moderate to high to very high), are contingent on future development pathways (high confidence) {7.3.1}.
Climate change is projected to significantly increase population exposure to heatwaves (very high confidence) and heat-related morbidity and mortality (high confidence). Models suggest exposure increases 16 times under Representative Concentration Pathway (RCP)4.5 and 36 times under RCP8.5, with the impact of warming amplified under development pathways that do not foster sustainable development . Globally, the impact of projected climate change on temperature-related mortality is expected to be a net increase under RCP4.5 to RCP8.5, even with adaptation (high confidence). Heat related cardiovascular disease mortality is projected to increase by the end of this century (high confidence). Strong geographical differences in heat-related mortality are projected to emerge later this century, mainly driven by population growth and aging in regions with tropical and subtropical climates (very high confidence) {7.3.1}.
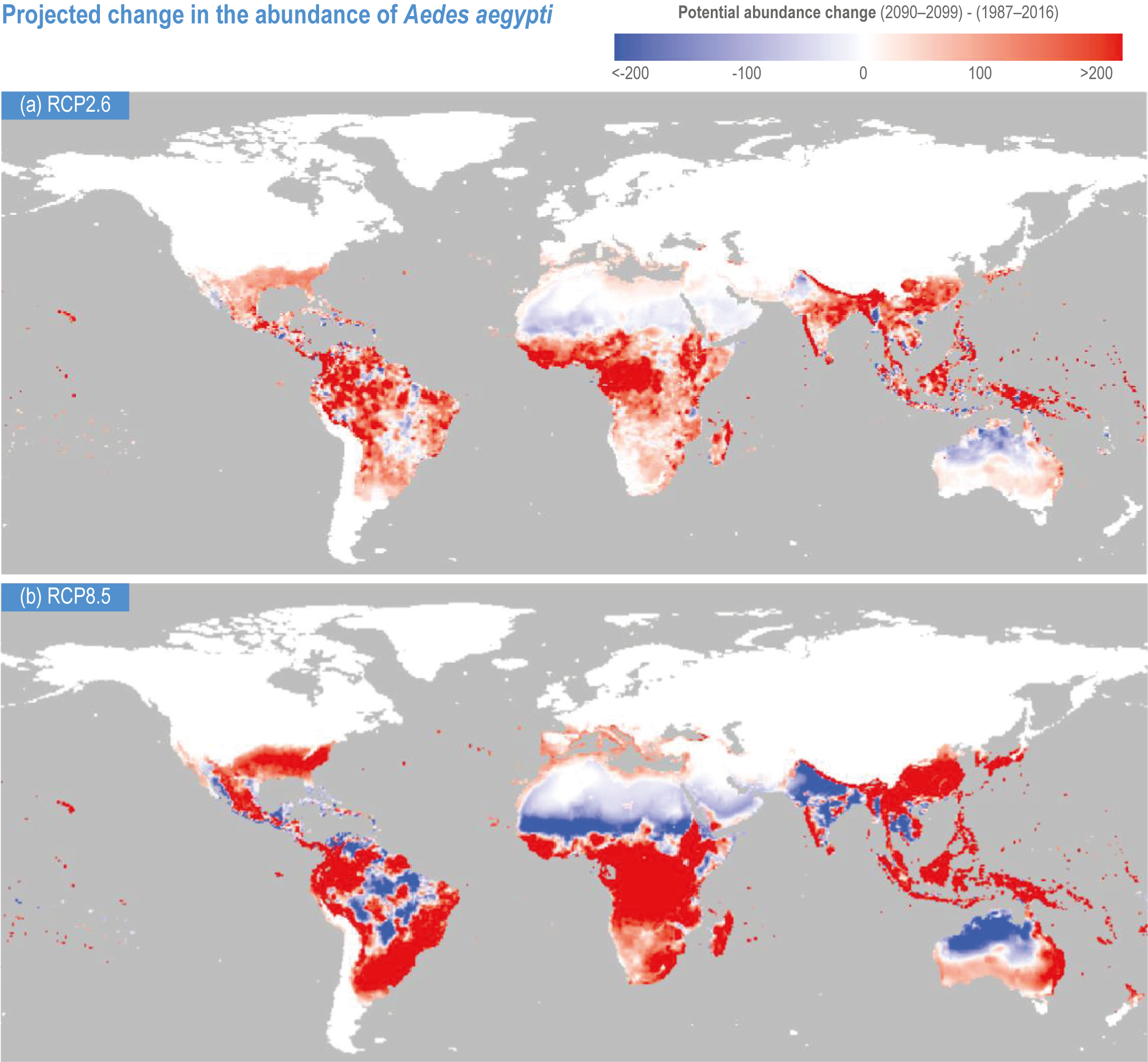
The burdens of several climate-sensitive food-borne, waterborne, and vector-borne diseases (VBDs) are projected to increase under climate change, assuming no additional adaptation (very high confidence). The distribution and intensity of transmission of malaria is expected to decrease in some areas and increase in others, with increases projected mainly along the current edges of its geographic distribution in endemic areas of sub-Saharan Africa, Asia and South America (high confidence). Dengue risk will increase, with a larger spatio-temporal distribution in Asia, Europe and sub-Saharan Africa under RCP6.0 and RCP8.5, potentially putting another 2.25 billion people at risk (high confidence). Higher incidence rates are projected for Lyme disease in the Northern Hemisphere (high confidence) and for transmission of Schistosoma mansoni in eastern Africa (high confidence) {7.3.1; Cross-Chapter Box ILLNESS in Chapter 2}.
Increasing atmospheric concentrations of carbon dioxide and climate change are projected to increase diet-related risk factors and related non-communicable diseasess globally and increase undernutrition, stunting and related childhood mortality particularly in Africa and Asia, with outcomes depending on the extent of mitigation and adaptation (high confidence) . These projected changes are expected to slow progress towards eradication of child undernutrition and malnutrition (high confidence). Higher atmospheric concentrations of carbon dioxide reduce the nutritional quality of wheat, rice and other major crops, potentially affecting millions of people at a doubling of carbon dioxide (very high confidence) {7.3.1}.
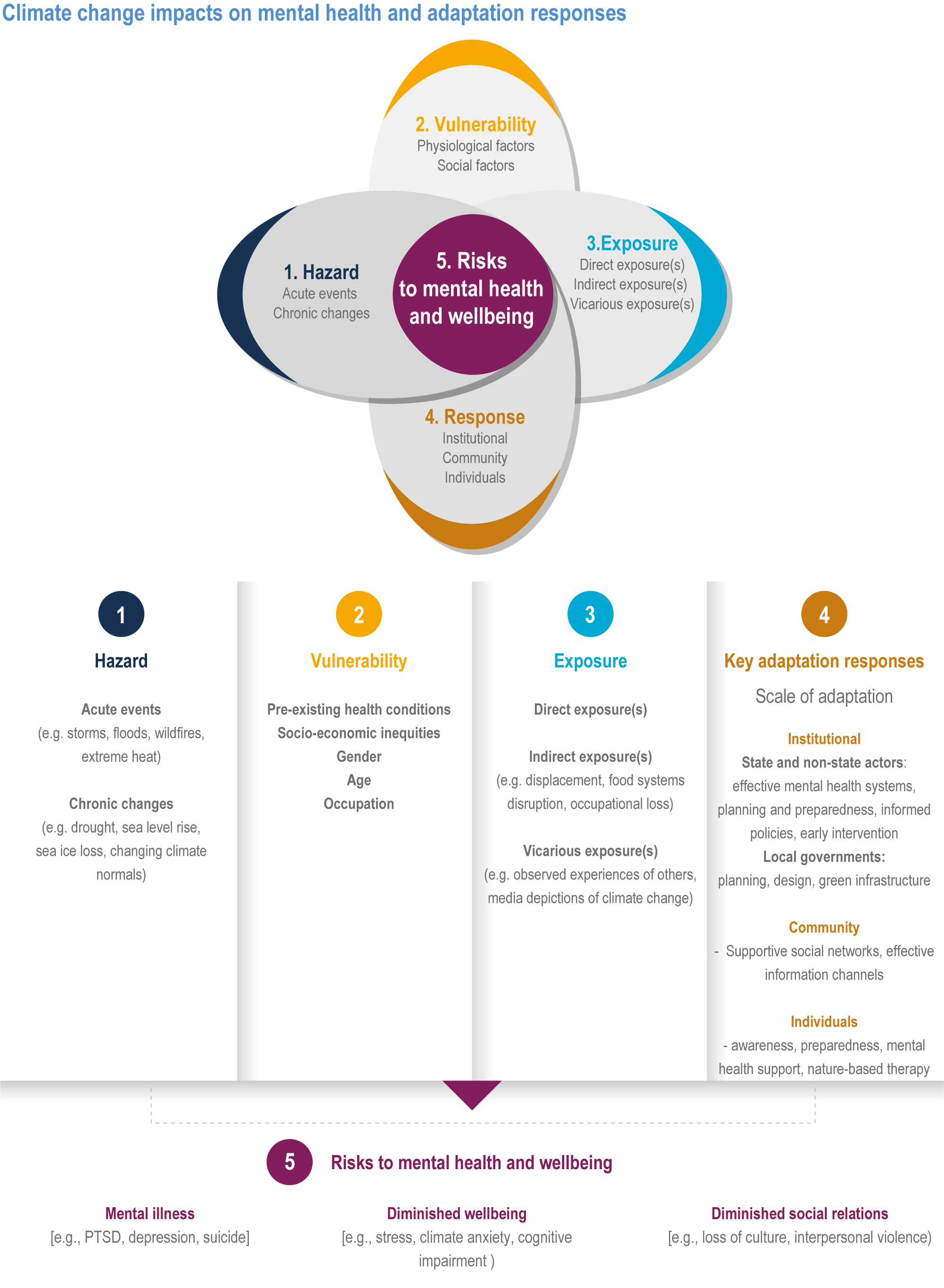
Climate change is expected to have adverse impacts on well-being and to further threaten mental health (very high confidence). Children and adolescents, particularly girls, elderly people, and people with existing mental, physical and medical challenges are particularly at risk. Mental health impacts are expected to arise from exposure to high temperatures, extreme weather events, displacement, malnutrition, conflict, climate-related economic and social losses, and anxiety and distress associated with worry about climate change (very high confidence) {7.3.1.11}.
Future climate-related migration is expected to vary by region and over time, according to future climatic drivers, patterns of population growth, adaptive capacity of exposed populations and international development and migration policies (high confidence). The wide range of potential outcomes is reflected in model projections of population displacements by 2050 in Latin America, sub-Saharan Africa and south Asia due to climate change, which vary from 31 million to 143 million people, depending on assumptions about future GHG emissions and socioeconomic development trajectories (high confidence). With every additional one degree Celsius of warming, the global risks of involuntary displacement due to flood events are projected to rise by approximately 50% (high confidence). High emissions/low development scenarios raise the potential for higher levels of migration and involuntary displacement (high confidence) and increase the need for planned relocations and support for people exposed to climate extremes but lacking the means to move (high confidence) {7.3.2; Cross-Chapter Box MIGRATE in Chapter 7}.
Climate change may increase susceptibility to violent conflict, primarily intra-state conflicts, by strengthening climate-sensitive drivers of conflict (medium confidence). Future violent conflict risk is highly mediated by socioeconomic development trajectories (high confidence) and so trajectories that prioritise economic growth, political rights and sustainability are associated with lower conflict risk (medium confidence). Future climate change may exceed adaptation limits and generate new causal pathways not observed under current climate variability (medium confidence). Economic shocks are not included in many models of conflict risks currently used, and some projections do not incorporate known socioeconomic predictors of conflict (medium confidence). As such, future increases in conflict-related deaths with climate change have been estimated, but results are inconclusive (medium confidence).
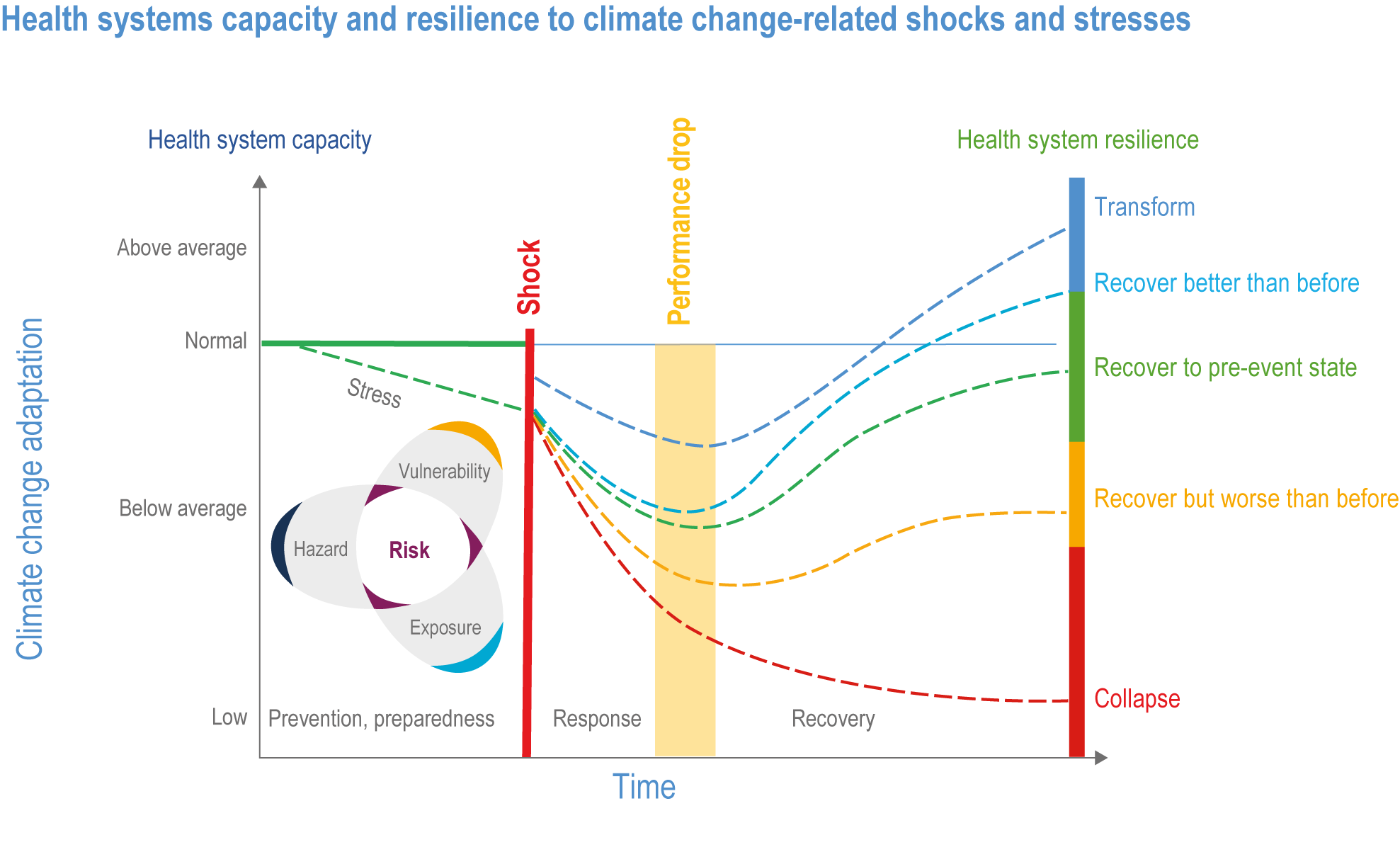
Solutions
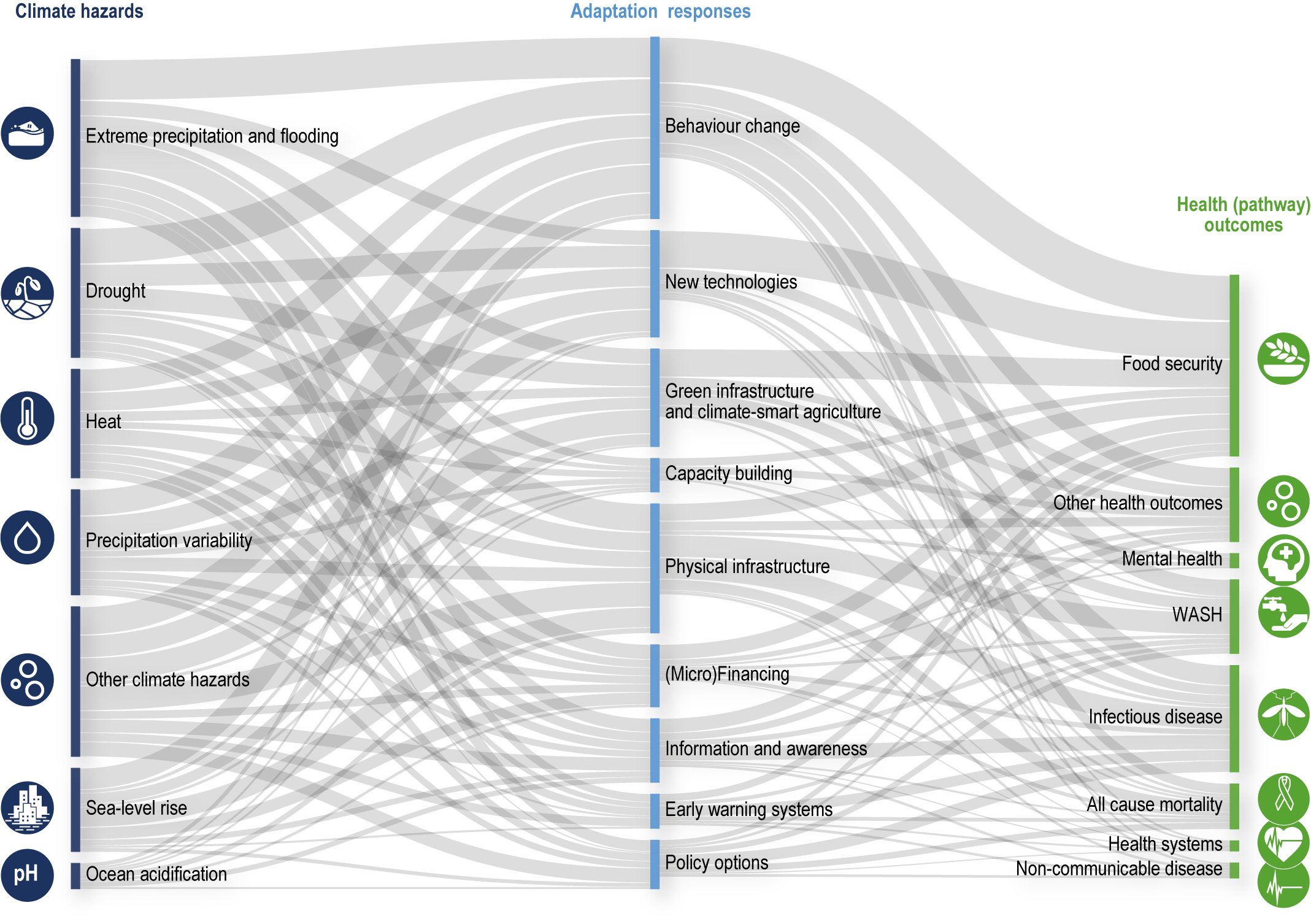
Since AR5, the value of cross-sectoral collaboration to advance sustainable development has been more widely recognised, but despite acknowledgement of the importance of health adaptation as a key component, action has been slow (high confidence). Building climate-resilient health systems will require multi-sectoral, multi-system and collaborative efforts at all governance scales (very high confidence) (Sections 7.4.1, 7.4.2). Globally, health systems are poorly resourced in general, and their capacity to respond to climate change is weak, with mental health support being particularly inadequate (very high confidence). The health sectors of some countries have focused on implementing incremental changes to policies and measures to fill the adaptation gap (very high confidence). As the likelihood of dangerous risks to human health continue to increase, there is greater need for transformational changes to health and other systems (very high confidence). This highlights an urgent and immediate need to address the wider interactions between environmental change, socioeconomic development and human health and well-being (high confidence) {7.4.1, 7.4.2, 7.4.3}.
Targeted investments in health and other systems, including multi-sectoral, integrated approaches to protect against key health risks can effectively increase resilience (high confidence). Increased investment in strengthening general health systems, along with targeted investments to enhance protection against specific climate-sensitive exposures (e.g., hazard early warning and response systems, and integrated vector control programmes for VBDs) will increase resilience if implemented to at least keep pace with climate change (high confidence).
- The future effects of climate change on VBDs can be significantly offset through enhanced commitment to and implementation of integrated vector control management approaches, disease surveillance, early warning systems and vaccine development (very high confidence) (Sections 7.4.1, 7.4.2).
- Adaptation options for future climate risks associated with waterborne and food-borne diseasess include improving access to potable water, reducing exposure of water and sanitation systems to flooding and extreme weather events, and improved (including expanded) early warning systems (very high confidence) (Sections 7.4.1, 7.4.2).
- Adaptation options for future extreme heat risks include heat action plans (HAPs) that incorporate early warning and response systems for urban and non-urban settings; tried, tested and iteratively updated response strategies targeting both the general population and vulnerable groups such as older adults or outside workers; and effective stakeholder communication plans (high confidence). These short-term responses can be complemented by longer-term urban planning and design, including nature-based solutions (NbS) that mitigate urban heat island (UHI) effects (high confidence) (Sections 7.4.1, 7.4.2, 7.4.3).
- Adaptation options to reduce the future risks of malnutrition include access to healthy, affordable, diverse diets from sustainable food systems (high confidence) ; health services including maternal, child and reproductive health (high confidence); nutrition services, nutrition and shock sensitive social protection (high confidence); water, sanitation and early warning systems (high confidence) ; and risk reduction schemes such as insurance (medium confidence) (Section 7.4.2.1.3).
The COVID-19 pandemic has demonstrated the value of coordinated and multi-sectoral planning, social protection systems, safety nets and other capacities in societies to cope with a range of shocks and stresses (high confidence) . The pandemic has posed a severe shock to many socioeconomic systems, resulting in substantial changes in vulnerability and exposure of people to climate risks (high confidence). The pandemic emphasises the inter-connected and compound nature of risks, vulnerabilities, and responses to emergencies that are simultaneously local and global (high confidence). Pathways to climate resilient development can be pursued simultaneously with recovering from the COVID-19 pandemic (high confidence). The COVID-19 pandemic has aggravated climate risks, demonstrated the global and local vulnerability to cascading shocks and illustrated the importance of integrated solutions that tackle ecosystem degradation and structural vulnerabilities in human societies (high confidence) {Cross-Chapter Box COVID in Chapter 7}.
Transitioning towards equitable, low-carbon societies has multiple benefits for health and well-being (very high confidence) . Benefits for health and well-being can be gained from wide-spread, equitable access to affordable renewable energy (high confidence); active transport (e.g., walking and cycling) (high confidence); green buildings and nature-based solutions, such as green and blue urban infrastructure (high confidence); and by transitioning to a low-carbon, well-being-oriented and equity-oriented economy consistent with the aims of the SDGs (high confidence). Plant-rich diets consistent with international recommendations for healthy diets could contribute to lower GHG emissions while also generating health co-benefits, such as reducing ill health related to over-consumption of animal-based products (high confidence) {7.4.2; Cross-Chapter Box HEALTH in Chapter 7; 7.4.4}.
Reducing future risks of involuntary migration and displacement due to climate change is possible through cooperative international efforts to enhance institutional adaptive capacity and sustainable development (high confidence). Institutional and cross-sectoral efforts to build adaptive capacity, coupled with policies aimed at ensuring safe and orderly movements of people within and between states, can form part of the CRDPs that reduce future risks of climate-related involuntary migration, displacement and immobility (medium confidence). In locations where permanent, government-assisted relocation becomes unavoidable, active involvement of local populations in planning and decision-making increases the likelihood of successful outcomes (medium confidence). People who live on small island states do not view relocation as an appropriate or desirable means of adapting to the impacts of climate change (high confidence) {7.4.3; Cross-Chapter Box MIGRATE in Chapter 7}.
Adaptation and sustainable development build peace in conflict-prone regions by addressing the drivers of grievances that lead to conflict and vulnerability to climate change (high confidence). Environmental peacebuilding (EP) through natural resource sharing, conflict-sensitive adaptation and climate-resilient peacebuilding offer promising avenues for addressing conflict risk, but their efficacy is still to be demonstrated through effective monitoring and evaluation (high confidence). Formal institutional arrangements for natural resource management contribute to wider cooperation and peacebuilding (high confidence) and gender-based approaches provide under-utilised pathways to achieving sustainable peace (medium confidence). Inclusion, cross-issue and cross-sectoral integration in policy and programming, and approaches that incorporate different geographical scales and work across national boundaries can support climate-resilient peace (high confidence) {7.4.5, 7.4.6}.
7.1 Introduction
This chapter assesses peer-reviewed and selected grey literature published since the IPCC’s Fifth Assessment Report (AR5) on the impacts and projected future risks of climate change for health, well-being, migration and conflict, taking into consideration determinants of vulnerability and the dynamic structure of human populations and communities. Particular attention is given to potential adaptation challenges and actions as well as potential co-benefits for health associated with mitigation actions. AR5 presented strong evidence-based statements regarding the likely 2 impacts of climate change on health, migration and conflict in two separate chapters on Human Health (Chapter 11) and Human Security (Chapter 12). The present chapter covers all topics found in AR5 Chapter 11 and Sections 12.4 (Migration and Mobility Dimensions of Human Security), 12.5 (Climate Change and Armed Conflict) and 12.6 (State Integrity and Geopolitical Rivalry) and provides an additional, expanded assessment of mental health impacts, gender dimensions of climate risks and solution pathways.
7.1.1 Major Health-Related Statements in AR5
AR5 stated with very high confidence that the health of human populations is sensitive to climate change (Smith et al., 2014). Specific observations of current impacts included the expansion of the geographical ranges of some diseases into previously unaffected areas and changes in the distributions of some food-, water- and vector-borne diseases (high confidence). Increasing future health risks were projected from injury, disease and death due to more intense heatwaves and fires (very high confidence) , undernutrition in poor regions (high confidence) , food- and waterborne diseases (very high confidence) and VBDs (medium confidence). AR5 found that climate change is a multiplier of existing health vulnerabilities, including food insecurity and limited access to safe water, improved sanitation, healthcare and education, and that the most effective measures to reduce vulnerability in the near term are programmes that implement and improve basic public health (very high confidence). Opportunities for co-benefits from mitigation actions were identified through such actions as reducing local emissions of short-lived climate pollutants from energy systems (very high confidence) and expanding transport systems that promote active travel (high confidence). The significant growth in peer-reviewed publications on links between climate change and human health and well-being since AR5 allowed for a more detailed and wider reaching assessment in the present chapter and stronger confidence statements for many climate-sensitive health outcomes.
7.1.2 Major Statements About Migration and Conflict in AR5
Key statements made in AR5 Chapter 12 (Human Security) about the impacts of climate change on migration were that climate change will have significant impacts on forms of migration that compromise human security and that mobility is a widely used strategy to maintain livelihoods in response to social and environmental changes (high agreement, medium evidence). Research on the influence of climate change and climate extremes on multiple forms of migration (including voluntary migration, involuntary displacement and immobility) has expanded significantly since AR5, which has allowed for a more robust assessment in this chapter, with migration also featuring in most other sectoral and regional chapters of this report. With respect to violent conflict, AR5 Chapter 12 found that people living in places affected by violent conflict are particularly vulnerable to climate change (medium evidence, high agreement ), that some of the factors increasing the risk of violent conflict within states are sensitive to climate change (medium evidence, medium agreement ) and that climate change will lead to new challenges to states and will increasingly shape both conditions of security and national security policies (medium evidence, medium agreement ). As with other subjects assessed in this chapter, there has been significant growth in the number of assessable studies, but there remain shortcomings with respect to the availability of evidence regarding the specific nature of causal linkages and the attributability of particular outcomes to climate events or conditions.
7.1.3 Important Developments Since AR5
7.1.3.1 International Agreements
Since AR5, several new international agreements have come into effect that have implications for international responses to the climate risks assessed in this chapter. The 2015 Paris Agreement, which explicitly mentions health in three separate sections, set new goals for adaptation and established a working group to study the effects of climate change on population displacement. The 17 United Nations (UN) SDGs for 2030, adopted in 2015, are all important for building adaptive capacity in general, with goals 13 (‘Take urgent action to combat climate change and its impacts’) and 3 (‘Ensure healthy lives and promote well-being for all at all ages’) being directly relevant to this chapter. Other SDGs contain specific targets that are also relevant for this chapter, including Target 10.7 (‘Well-managed migration policies’), Target 8.3 (‘Decent work for all’) and Target 5.4 (‘Promotion of peaceful and inclusive societies’) (Piper, 2017). The 2015 Sendai Framework for Disaster Risk Reduction puts an emphasis on health and well-being (Aitsi-Selmi and Murray, 2016) In 2018, UN member states negotiated Global Compacts for Safe, Orderly and Regular Migration and on Refugees that, taken together with the Paris Agreement, provide pathways for coordinated international responses to climate-related migration and displacement (Warner, 2018).
7.1.3.2 IPCC Special Reports
All three post-AR5 IPCC Special Reports considered some of the research that is assessed here in greater detail. The 2018 report on 1.5°C (SR1.5) included a review of climate change and health literature published since AR5 and called for further efforts for protecting health and well-being of vulnerable people and regions (Ebi et al., 2018b) and highlighted links between climate change hazards, poverty, food security, migration and conflict. The 2019 Special Report on Climate Change and Land (SRCCL) (IPCC, 2019b) emphasised the impacts of climate change on food security; highlighted links between reduced resilience of dryland populations, land degradation, migration and conflict; and raised concerns about the impacts of climate extremes. The 2019 Special Report on the Ocean and Cryosphere in a Changing Climate (IPCC, 2019a) detailed how changes in the cryosphere and ocean systems have impacted people and ecosystem services, particularly food security, water resources, water quality, livelihoods, health and well-being, infrastructure, transportation, tourism and recreation as well as the culture of human societies, particularly for Indigenous Peoples. It also noted the risks of future displacements due to rising sea levels and associated coastal hazards.
7.1.4 Interpretation of ‘Health and Well-Being’ Used in This Chapter
Assessing the links between human health, well-being and climate change is a new task for AR6, reflecting a broad perspective on health that increasingly acknowledges the importance of well-being and its interactions with individual and population health. The World Health Organization (WHO) defines health as ‘a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity’ (WHO, 1946). Although this chapter assesses physical health, mental health and general well-being separately, they are inter-connected; any type of health problem can reduce overall well-being and vice versa. For example, a child receiving inadequate nutrition may not be sick but is experiencing a clear threat to well-being that has implications for future physical and mental health.
There is no consensus definition of well-being, but it is generally agreed that it includes a predominance of positive emotions and moods (e.g., happiness) compared with extreme negative emotions (e.g., anxiety), satisfaction with life, a sense of meaning and positive functioning, including the capacity for unimpaired cognitive functioning and economic productivity (Diener and Tay, 2015; Piekałkiewicz, 2017). A capabilities approach (Sen, 2001) focuses on the opportunity for people to achieve their goals in life (Vik and Carlquist, 2018) or the ability to take part in society in a meaningful way, and is reflected in personal freedoms, human agency, self-efficacy, ability to self-actualise, dignity and relatedness to others (Markussen et al., 2018). An indigenous perspective on well-being is broad and typically incorporates a healthy relationship with the natural world (Sangha et al., 2018); emotional and mental health have also been linked to a strong cultural identity (Butler et al., 2019; Dockery, 2020). ‘Health’ itself is sometimes described as including relationships between humans and nature as well as links to community and culture (Donatuto et al., 2020; Dudgeon et al., 2017).
Subjective well-being is consistently associated with personal indicators such as higher income, greater economic productivity, better physical health (Diener and Tay, 2015; Delhey and Dragolov, 2016; De Neve et al., 2013) and environmental health, and it is reflected in societal indicators such as social cohesion and equality (Delhey and Dragolov, 2016). In a global survey of over 1 million people taken between 2004 and 2008 via the Gallup World Poll, annual income and access to food were strong predictors of subjective well-being and a healthy environment. In particular, access to clean water was important even when household income was controlled (Diener and Tay, 2015). Access to green spaces was also closely associated with well-being (high confidence) (Lovell et al., 2018; Yuan et al., 2018).
7.1.5 Towards Socioecological Perspectives on Health, Well-Being, and Loss and Damage
Since AR5, more comprehensive frameworks for framing and studying global health issues, including planetary health, ‘One Health’ and eco-health, have gained traction. These frameworks share an ecological perspective, emphasise the role of complex systems and highlight the need for inter-disciplinary approaches related to human health research and practice (Lerner and Berg, 2015; Zinsstag et al., 2018; Whitmee et al., 2015; Steffen et al., 2015). These frameworks increasingly shape the evidence related to climate change health impacts and response options, highlight the dynamics of complex systems in risk management and direct risk management efforts in new directions.
Building on these frameworks and perspectives, there is increasing overlap in the literature on global health, climate change impacts and estimates of loss and damage. The Global Burden of Disease study for 2019 for the first time included non-optimal temperature as a risk factor (Murray et al., 2020). Work by social scientists continues to explore how climate change indirectly affects resource availability, productivity, migration and conflict (Burke et al., 2015a; Carleton and Hsiang, 2016; Hsiang et al., 2017), bringing multiple lines of inquiry together to study the associations between global environmental changes, socioeconomic dynamics and impacts on health and well-being. Morbidity associated with migration and displacement, especially in the context of small island states, has been identified as a non-material form of loss and damage (Thomas and Benjamin, 2020; McNamara et al., 2021). Social costs of carbon estimates have been updated to include excess mortality associated with climate change, increasing estimates substantially (Dressler, 2021).
7.1.6 Developments Relevant to Tracking and Assessing Climate Change Impacts on Health
Since AR5, there has been a steady increase in standardised, globally scoped, data-driven health impact assessments, such as the ongoing Global Burden of Disease study (James et al., 2018) that now includes scenario-based projections (Foreman et al., 2018), that make linkages with other global priorities, including the SDGs (Fullman et al., 2017). Attention has turned from prioritising specific diseases like HIV/AIDS, malaria and tuberculosis, to strengthening health systems and providing universal health coverage (Chang et al., 2019), with an ongoing emphasis on the social determinants of health. Several climate-sensitive health outcomes are now tracked in the annual Lancet Countdown reports (Watts et al., 2015; Watts et al., 2017; Watts et al., 2018b; Watts et al., 2019; Watts et al., 2021). The Global Burden of Disease study is beginning to examine climate-sensitive disease burdens, incorporate temperature as a risk factor (Murray et al., 2020) and project future cause-specific disease burdens in a warming world (Burkart et al., 2021). Although not assessed in this chapter, there are numerous ongoing assessments of climate change impacts on health and well-being being undertaken by national and local health authorities that continue to generate insights into climate-related health impacts and suggest response options relevant for decision makers.
While the knowledge base regarding global health has increased, a comprehensive framework is not in place that fully integrates health, well-being and environmental impacts from climate change allowing for the cumulative assessment of their impact. Moreover, significant cracks in the foundation of global health governance that affect preparedness and adaptive capacity for climate change, among other threats, have been identified (Phelan et al., 2020; Defor and Oheneba-Dornyo, 2020; Ostergard et al., 2020; Shaffie, 2021). While attention to climate change and health has increased and there is evidence of increasing adaptation activity in the health sector (Watts et al., 2019), there is also continued evidence of substantial adaptation gaps (UNEP, 2018; UNEP, 2021) including gaps in humanitarian response capacity for climate-related disasters (Watts et al., 2021) that appear to be widening as adverse climate change impacts on health and well-being accrue.
7.1.7 Hazards, Exposure and Vulnerability in the Context of Human Health, Well-Being and the Changing Structure of Communities
7.1.7.1 Possible Climate Futures and Hazards
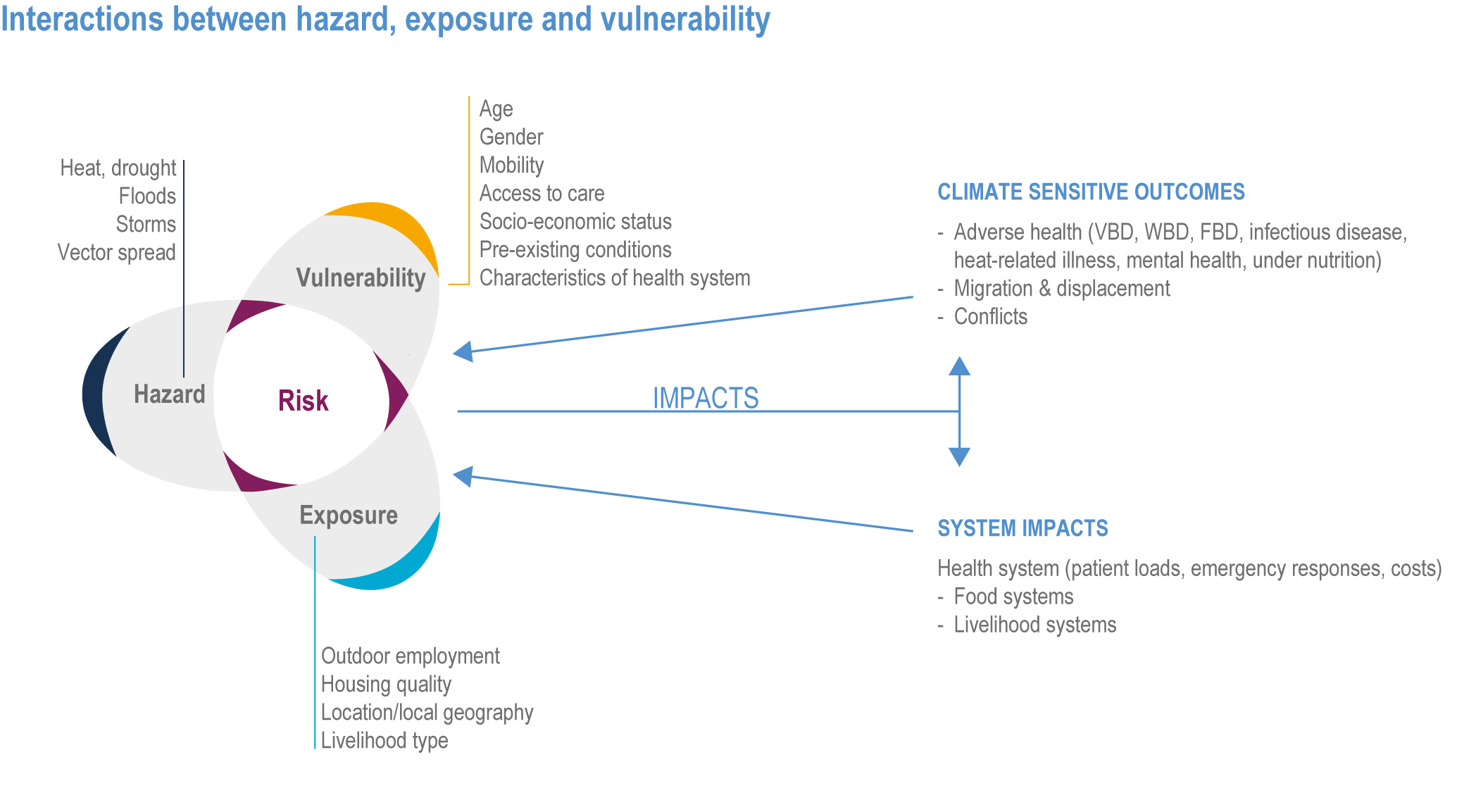
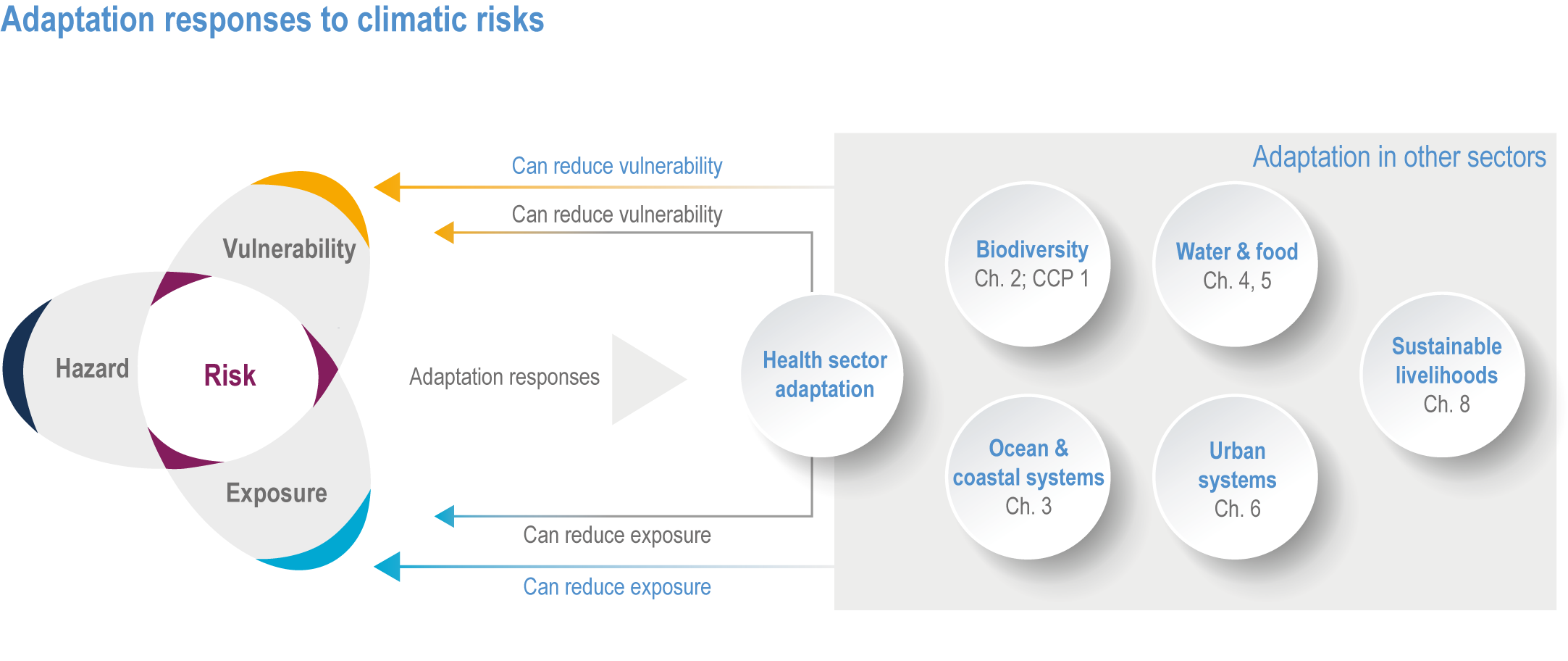
This chapter uses the conceptual framing described in Chapter 1, in which risks emerging from climate change are described in terms of hazard, exposure and vulnerability, with adaptation and climate resilient development being responses that have the potential to reduce or modify risk. The observed and projected future risks to health well-being, involuntary population displacements and conflict identified in this chapter are associated with a range of hazards that are manifested at a variety of geographical and temporal scales. These include observed and projected changes in climate normals; changes in the frequency, duration, and/or severity of extreme events; and hazards such as rising sea levels and extreme temperatures where the impacts have only begun to be widely experienced. The 2021 report of IPCC WGI (IPCC, 2021) provides an assessment of observed and projected changes in these hazards and is the backdrop against which assessments of future risks and adaptation options identified in the present chapter should be considered.
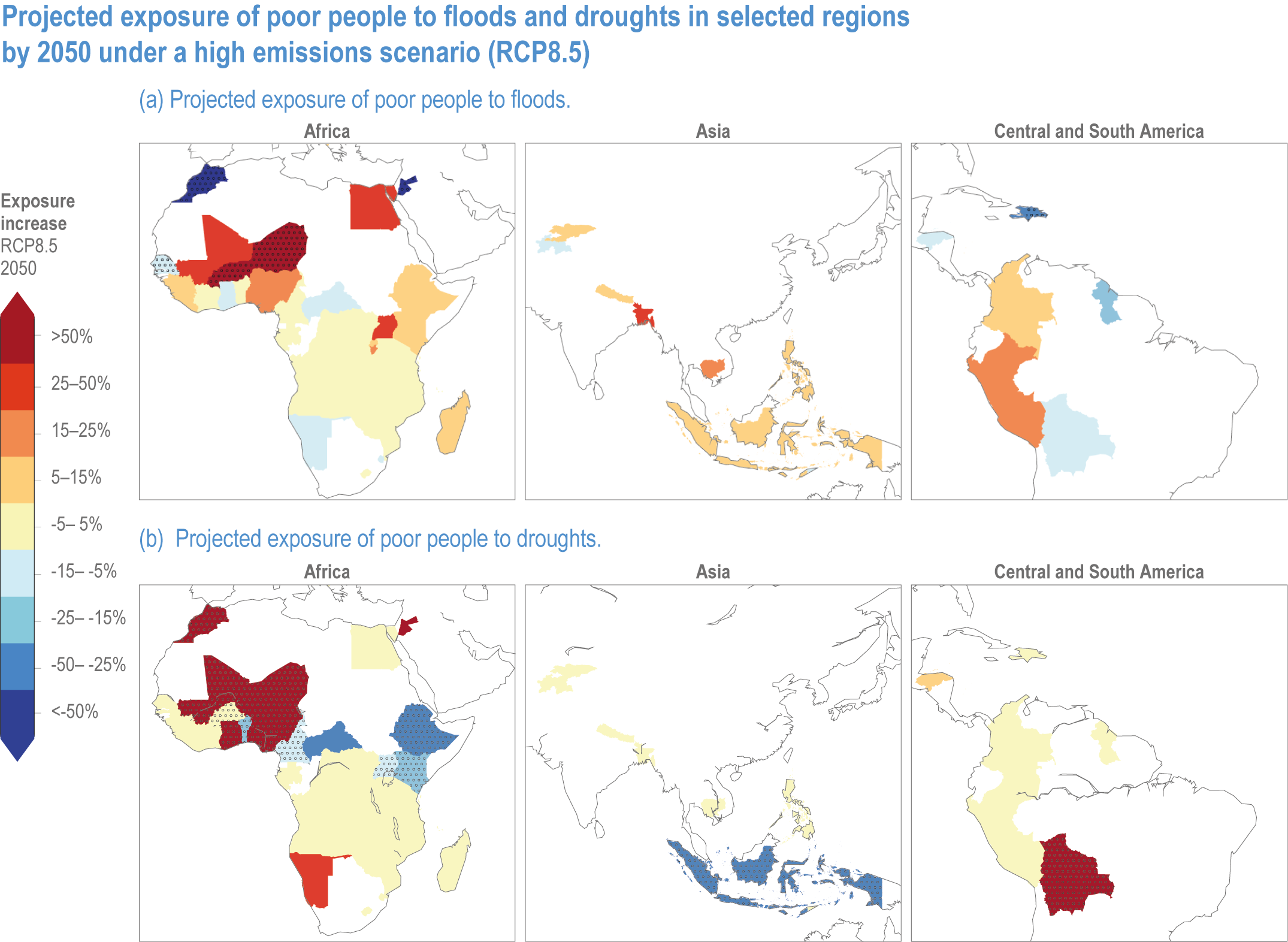
The exposure to hazards of populations, infrastructure, ecosystem capital, socioeconomic systems and cultural assets critical to health and well-being varies considerably across and within regions (high confidence). Exposure is also projected to vary across and within regions over time, depending on future GHG emissions pathways, development trajectories and differential vulnerability, particularly for exposure to extreme events and conditions, such as floods and droughts (Figures 7.1a, 7.1b) (Winsemius et al. 2018). For this reason, region-specific assessments of climate-related risks for health, displacement and conflict are found in each of the regional chapters of this report in addition to the general assessment that appears in this chapter.
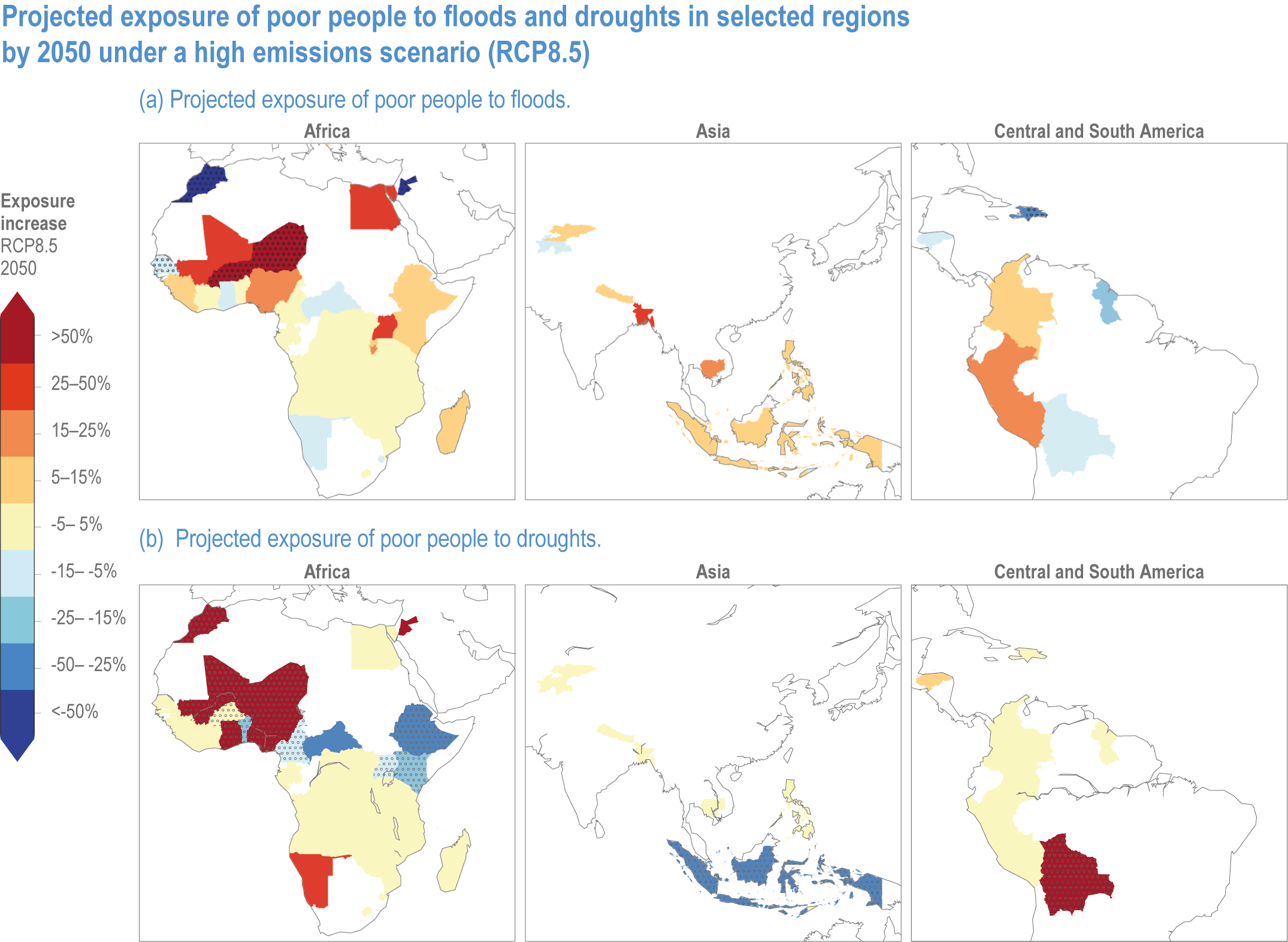
Figure 7.1 | Projected exposure of poor people toa) floods respectivelyb) droughts in selected regions by 2050 under a high emissions scenario (RCP8. 5) (adapted from Winsemius et al., 2018).
7.1.7.2 Differential Vulnerability and Cascading Effects
Vulnerability to climate change varies across time and location, across communities, and among individuals within communities; it reflects variations and changes in macro-scale non-climatic factors (such as changes in population, economic development, education, infrastructure, behaviour, technology and ecosystems) and individual- or household-specific characteristics, such as age, socioeconomic status, access to livelihood assets, pre-existing health conditions and ability (US Global Change Research Program, 2016; Chapter 1).
Many direct and indirect effects of climate change pose multiple threats to human health and well-being and can occur simultaneously, resulting in compounding or cascading impacts for vulnerable populations. For example, many of the long-term impacts of climate change on NCDs and injury described in Sections 7.2 and 7.3 are associated with future increases in air temperature and levels of air pollution; in many regions, and especially in large urban centres in Asia and Africa, these particular hazards are already causing substantial increases in morbidity and mortality due to respiratory illnesses (Tong et al., 2016). Climate change can therefore be expected to magnify such health risks over the long term.
At the same time, urban populations will also be experiencing indirect risks through climate change impacts on food and potable water systems, variations in the distribution and seasonality of infectious diseases and growing demand for shelter due to increased in-migration. The accumulation of these risks over time can be expected to generate accelerating declines in community resilience and health, with future vulnerability potentially expanding in a nonlinear fashion (Dilling et al., 2017; Liang and Gong, 2017; El-Zein and Tonmoy, 2017; see also Chapter 6). Further, although each individual risk in isolation may be transitory or temporary for the individuals or groups exposed, taken cumulatively, the impacts could create conditions of chronic lack of well-being, and early life experiences with specific illnesses and conditions could have lifelong consequences (Watts et al., 2015; Otto et al., 2017; WHO, 2018a). In this context, there is a distinct need for greater longitudinal research on vulnerability to multiple climatic and non-climatic health and well-being hazards over time (Fawcett et al., 2017). There is also need for more research to identify critical thresholds in social vulnerability to climate change (Otto et al., 2017); these include rapid, stepwise changes in vulnerability that emerge from changes in exposure (for example, air temperatures above which mortality rates or impacts on pre-natal health accelerate (Arroyo et al., 2016; Ngo and Horton, 2016; Abiona, 2017; Auger et al., 2017; Molina and Saldarriaga, 2017; Zhang et al., 2017b)) and thresholds in adaptation processes (such as when rural out-migration rates grow due to climate-related crop failures (McLeman, 2017)).
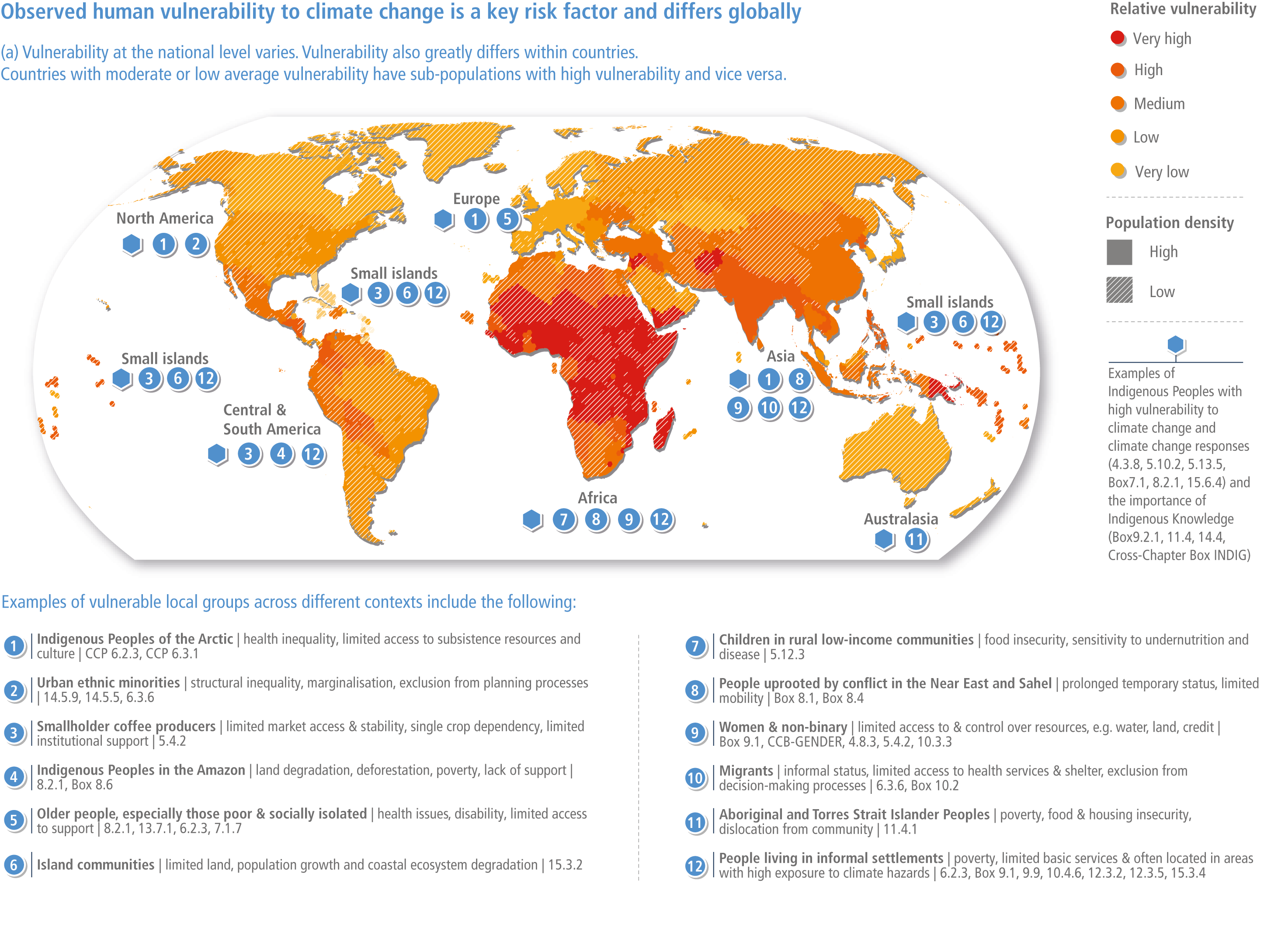
In virtually all of the research identifying particular climate-related risks to health, well-being, migration and conflict, specific types of individuals are identified as having higher levels of vulnerability and exposure to climate-related health hazards: people who are impoverished, undernourished, struggle with chronic or repeated illnesses, live in insecure housing in polluted or heavily degraded environments, work in unsafe conditions, are disabled, have limited education and/or have poor access to health and social infrastructure (WHO, 2018a). Their disproportionate exposure to ongoing climate hazards and their inability to recover from extreme events increase not only their own vulnerability but also that of the wider communities in which they live (US Global Change Research Program, 2016). Highly vulnerable populations are not evenly distributed across regions (Figure 7.2) nor within countries. Yet, even those fortunate enough to live in better neighbourhoods with greater financial means, higher-paying jobs and good access to resources and services, may experience adverse climate-related outcomes through community-level interactions and linkages (Haines and Ebi, 2019). Increased inequity itself threatens well-being and an effective response to climate change should not only avoid increased inequity but identify ways in which to reduce existing inequity.
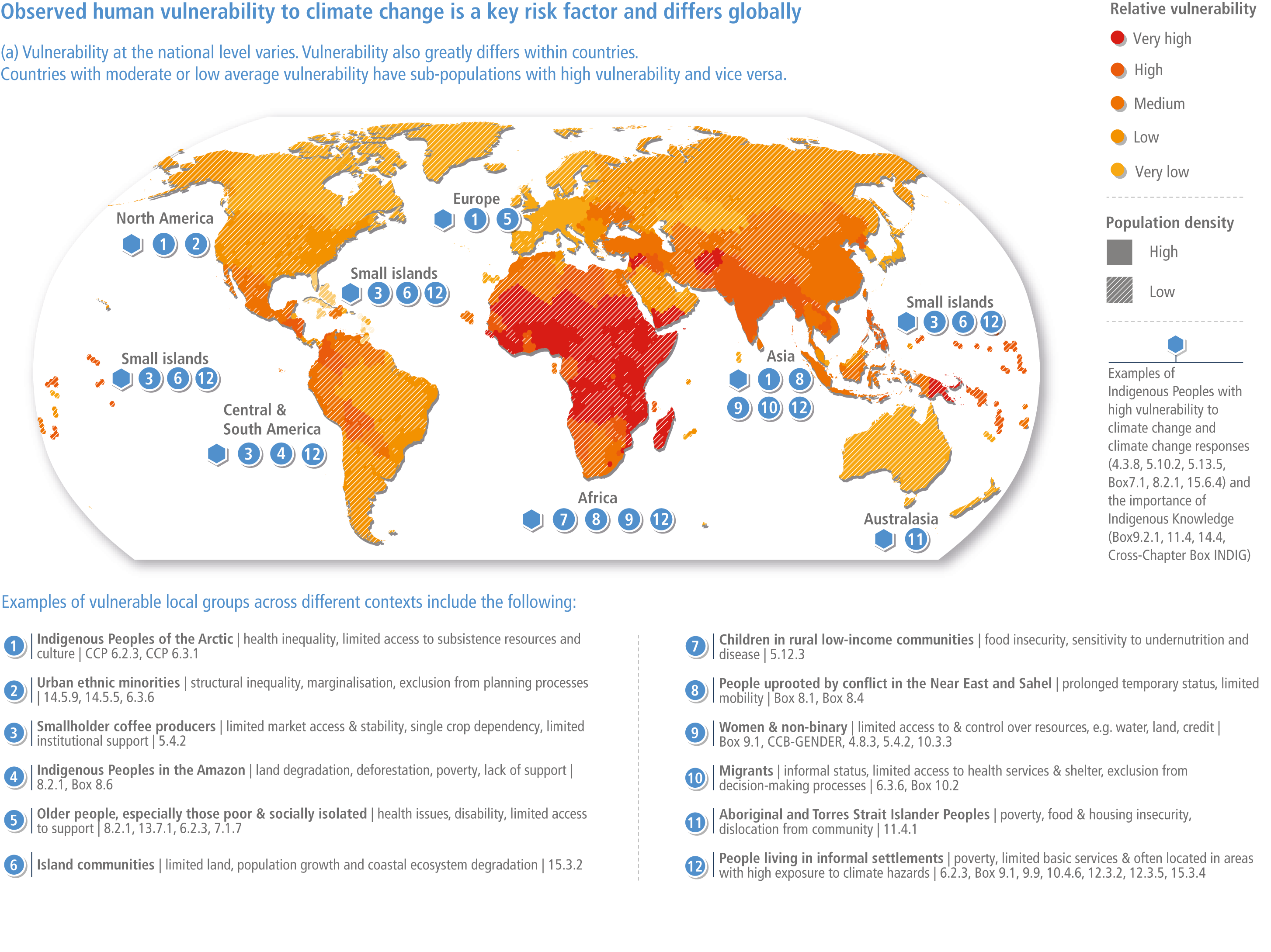
Figure 7.2 | Global distribution of vulnerable people from two indices, with examples (see also Technical Summary, this report).
7.1.7.3 Heightened Vulnerability to Climate-Related Impacts on Health and Well-Being Experienced by Specific Groups and Through Specific Pathways
7.1.7.3.1 Women and Girls
Climate change poses distinct risks to women’s health. Vulnerability to climate-related impacts on health and well-being shows notable differentiations according to gender, beyond implications for pregnant women. In many societies, differential exposure to such risks relate to gendered livelihood practices and mobility options. Pregnancy and maternal status heighten vulnerability to heat, infectious diseases, food-borne infections and air pollution (Arroyo et al., 2016; Ngo and Horton, 2016; Zhang et al., 2017b). Extreme heat events, high ambient temperatures, high concentrations of airborne particulates, water-related illnesses and natural hazards are associated with higher rates of adverse pregnancy outcomes such as spontaneous abortion, stillbirth, low birth weight and pre-term birth (Arroyo et al., 2016; Ngo and Horton, 2016; Abiona, 2017; Auger et al., 2017; Molina and Saldarriaga, 2017; Zhang et al., 2017b). Women and girls are at greater risk of food insecurity (FAO, 2018; Alston and Akhter, 2016), which is particularly problematic in combination with the nutritional needs associated with pregnancy or breastfeeding. Women and girls are more likely to die in extreme weather events (Garcia and Sheehan, 2016; Yang et al., 2019). Women are also expected to face a greater mental health burden in a changing climate (Manning and Clayton, 2018). Further, climatic extremes and water scarcity are associated with increases in violence against girls and women (Anwar et al., 2019; Opondo et al., 2016; Le Masson et al., 2016; Udas et al., 2019).
7.1.7.3.2 Children
Children are particularly vulnerable to climate change impacts. Children often have unique pathways of exposure and sensitivity to climate hazards, given their immature physiology and metabolism and high intake of air, food and water relative to their body weight as compared with adults (US Global Change Research Group, 2016). Climate change is expected to increase childhood risks of malnutrition and infectious disease for children in low-income countries through its impacts on household food access, dietary diversity, nutrient quality, water and changes in maternal and childcare access and breastfeeding (Tirado, 2017; FAO et al., 2018; Perera, 2017). Children living in locations with poor sanitation are especially vulnerable to GI illnesses, with future rates of diarrhoeal diseases among children expected to rise under many climate change scenarios (Cissé et al., 2018; WHO, 2014). Outdoor recreational opportunities for children may be reduced by extreme weather events, heat and poor air quality (Evans, 2019). Children and adolescents are particularly vulnerable to post-traumatic stress after extreme weather events; the effects may even be long-lasting, with impacts on their adult functioning (Brown et al., 2017; UNICEF, 2021; Thiery et al., 2021)
7.1.7.3.3 Elderly
Population age structures and changes over time have a significant influence on vulnerability to the impacts of weather and climate. Older adults (generally defined as persons aged 65 and older) are disproportionately vulnerable to the health impacts associated with climate change and weather extremes, including a greater risk of succumbing to waterborne pathogens due to poorer functioning thermoregulatory mechanisms, greater sensitivity to dehydration, changes in their immune systems and greater likelihood of having pre-existing chronic illnesses such as diabetes or respiratory, cardiovascular and pulmonary illnesses (Benmarhnia et al., 2016; Diaz et al., 2015; Mayrhuber et al., 2018; Paavola, 2017). Older adults may be less prompt in seeking medical attention when suffering from GI illnesses, which can lead to dehydration (Haq and Gutman, 2014). Åström et al. (2017) anticipate heat-related mortality among the elderly in Europe to rise in the 2050s under RCP4.5 and RCP8.5 in the absence of significant preventative measures. In a study of the combined effects of warming temperatures and an aging population in Korea, Lee and Kim (2016) projected a four- to six-fold increase in heat-related mortality by the 2090s when accounting for temperature and age structure.
7.1.7.3.4 Socioeconomically Marginalised Populations and People with Disabilities
People living in poverty are more likely to be exposed to extreme heat and air pollution and have poorer access to clean water and sanitation, accentuating their exposure to climate change-associated health risks (UNEP, 2021; FAO et al., 2018). Poverty influences how people perceive the risks to which they are exposed, how they respond to evacuation orders and other emergency warnings and their ability to evacuate or relocate to a less risk-prone location (US Global Change Research Program, 2016). Poorer households, who often live in highly exposed locations, are more likely to be forced into low-agency migration as a means of adapting to climate risks and at the same time are the most likely to be immobile or trapped in deteriorating circumstances where migration would be a preferred response (Leichenko and Silva, 2014; Fazey et al., 2016; Sheller, 2018). Climate emergencies disproportionally affect people with disabilities because of their inherent vulnerabilities, which may impair their ability to take protective action; they are also frequently excluded from adaptation planning (Gaskin et al., 2017).
7.1.7.3.5 Urban Compared with Rural Populations
Rural and urban populations are often exposed to different types of climate-related health risks. For example, because of the UHI effect and high concentrations of air pollution from motor vehicles and industrial activity, people who live in urban areas may have higher rates of extreme heat stress and respiratory illnesses than their rural counterparts (Hondula et al., 2014; Heaviside et al., 2016; Macintyre et al., 2018; Schinasi et al., 2018). Conversely, rural populations, especially those dependent on resource-based livelihoods, may have a greater exposure to climate impacts on food production or natural hazard events, which have subsequent effects on household nutrition and food security (Springmann et al., 2016a; see also Chapters 5 and 6 of this report).
7.1.7.3.6 Indigenous Peoples
Indigenous Peoples, especially those who live in geographically isolated, resource-dependent and/or impoverished communities, are often at greater risk of health impacts of climate change (Ford et al., 2020) (US Global Change Research Program, 2016). The close inter-connection of land-based livelihoods and cultural identity of many indigenous groups exposes them to multiple health- and nutrition-related hazards (Durkalec et al., 2015; Sioui, 2019) with potential implications for community social relations and individual mental health (Cunsolo Willox et al., 2013; Cunsolo Willox et al., 2015). Climate change risk exposures may be complicated by changes in lifestyle, diet and morbidity driven by socioeconomic processes, further increasing health risks for Indigenous Peoples (Jaakkola et al., 2018). Environmental consequences of climate change can also affect social ties and spiritual well-being, in part because land is often an integral part of their culture and spiritual identity.
7.1.7.3.7 Vulnerability Experienced through Food Systems
Stresses and shocks associated with climate change are drivers of food insecurity, particularly in sub-Saharan Africa, Asia and Latin America (Betts et al., 2018). The most vulnerable groups include smallholder farmers, pastoralists, agricultural laborers, poorer households, refugees, indigenous groups, women, children, the elderly and those who are socioeconomically marginalised (FAO et al., 2018; IPCC, 2019b) (high confidence). Men, women, children, the elderly and the chronically ill have different nutritional needs and these vulnerabilities may be amplified by gendered norms and differential access to resources, information and power (IPCC, 2019b). Extreme climate events have immediate and long-term impacts on food insecurity and malnutrition in poor and vulnerable communities, including when women and girls need to undertake additional duties as laborers and caregivers (FAO et al., 2018).
7.1.7.3.8 Health Vulnerability Experienced through Water and Sanitation Systems
Water and sanitation systems are particularly vulnerable to extreme weather events, and damage to such systems can lead to contamination of drinking water and subsequent adverse health impacts (Howard et al., 2016; Khan et al., 2015; Sherpa et al., 2014). In areas with only very simple traditional excreta disposal facilities (e.g., latrines) and traditional sources of water (e.g., unprotected wells), the repeated occurrence of floods and other extreme events can negatively affect water quality at household and community levels and increase the burden of food- and waterborne diseases (Cissé et al., 2016; Khan et al., 2015; Kostyla et al., 2015).
Box 7.1 | Indigenous Peoples’ Health and Well-Being in a Changing Climate
Contributing authors: Hannah Tait Neufeld (Canada), Lena Maria Nilsson (Sweden), Rhys Griffith Jones (New Zealand)
The indigenous population worldwide is estimated at 476 million people spread across all geographic regions of the world (FAO et al., 2021). Indigenous Peoples globally represent a large heterogeneity of people in terms of living conditions and social determinants of health. There is no simple definition of who is indigenous. In this text, we refer to Indigenous Peoples as people self-identified and organised as indigenous, according to the principles of the International Work Group for Indigenous Affairs (IWGIA), an international non-governmental organisation (NGO) with observer status at the United Nations (UN). Indigenous Peoples are described as ‘distinct social and cultural groups that share collective ancestral ties to the lands and natural resources where they live, occupy or from which they have been displaced’ (World Bank, 2021). A common experience among Indigenous Peoples are historical traumas related to overseas and/or settler/industrial colonisation.
Studies on climate change as it affects the health of Indigenous Peoples generally focus on non-displaced indigenous groups; that is, Indigenous Peoples maintaining culturally important elements of a land-based traditional lifestyle. Here we use an eco-medicine perspective in which the impacts of climate change on health are divided into primary, secondary and tertiary effects, as discussed below (Butler and Harley, 2010). Many analyses of indigenous health in relation to climate change use the One Health concept (Mackenzie and Jeggo, 2019; see Section 7.1.5).
Current Impacts of Climate Change on Health and Well-Being of Indigenous Peoples
Primary health effects of climate change include the immediate physical effects on human health, such as health hazards due to high temperatures, extreme weather events or accidents from exposure to climate-related hazards. For example, in arid and semiarid areas, an increased frequency of severe droughts is associated with immediate health problems related to overheating and lack of water for drinking, sanitation and livestock (Hall and Crosby, 2020; Mamo, 2020; Rankoana, 2021). In many cases, the possibilities for Indigenous Peoples to apply traditional strategies to mitigate droughts by migration are limited by competing land use, environmental protection and national borders, with many examples across Africa (Mamo, 2020). In the Jordan River Valley, the second most water stressed area in the world, water resources are not equally distributed to Indigenous Bedouin people, amplifying their immediate health threat during predictable as well as unpredictable droughts (Mamo, 2020).
In Arctic and sub-Arctic areas, higher temperatures with increased numbers of freeze–thaw cycles during the winter means increased occurrences of transport-related accidents in indigenous communities due to weaker ice on travel routes that cross lakes, rivers and the sea, along with changes in the snow cover and increased risk of avalanches (Durkalec et al., 2015; Jaakkola et al., 2018). Impeded access to healthcare during extreme weather conditions is a primary health risk for Indigenous Peoples living in remote areas (Amstislavski et al., 2013; Hall and Crosby, 2020; Mamo, 2020).
Pastoralists in many regions may experience changes in livestock behaviour due to climate change, leading to increased mobility-related health hazards (Jaakkola et al., 2018; Mamo, 2020). Indigenous Peoples living in low-lying coastal areas and small island states face long-term risk of flooding and the stresses of resettlement (Maldonado et al., 2021; McMichael and Powell, 2021).
Extreme rainfall, flooding, storms, heatwaves and wildfires lead to individual health hazards that may include injuries and thermal and respiratory traumas (Mamo, 2020) There are many examples when emergency responses to extreme events have ignored the needs of displaced Indigenous Peoples (Mendez et al., 2020; Maldonado et al., 2021). Population-based quantitative studies documenting the direct effects of these events on Indigenous Peoples are rare. In Mexico, respiratory diseases are almost twice as common among Indigenous Peoples compared to non-Indigenous Peoples (de Leon-Martinez et al., 2020). In Alaska and northern Canada, alarming levels of respiratory stress and disease have been reported among Inuit and First Nation communities in relation to wildfires (Howard et al., 2021), as well as increased mould in houses due to flooding resulting from increased precipitation (Furgal and Seguin, 2006; Harper et al., 2015; Norton-Smith et al., 2016 ). Climate- and housing-related respiratory stress is also a risk factor for severe COVID-19 infection, which has been highlighted in recent literature from an indigenous health perspective (de Leon-Martinez et al., 2020).
Secondary effects relate to ecosystem changes, for example, the increased risk of the acute spread of air-, soil-, vector-, food-, and waterborne infectious diseases (Hueffer et al., 2019). Higher proportions of climate-related infectious diseases are reported among indigenous groups compared to their non-indigenous neighbours, with examples from Torres Strait, Australia, showing a greater proportion of tuberculosis, dengue, Ross River virus, melioidosis, and non-tuberculous mycobacterial infections (Hall et al., 2021) and in the Republic of Sakha, Russia, high levels of zoonoses (Huber et al., 2020a). Increasing levels of livestock and canine diseases are also reported (Mamo, 2020; Bogdanova et al., 2021; Hillier et al., 2021). Another secondary health effect is an increase in human–animal conflicts, for example human–elephant conflicts in Namibia due to plant food scarcity (Mamo, 2020), human–bear conflicts in Arctic regions within Canada (Wilder et al., 2017), human–tiger conflicts in Bangladesh (Haque et al., 2015) and increased predatory pressure on Indigenous Peoples’ livestock and game worldwide (Haque et al., 2015; Jaakkola et al., 2018; Mukeka et al., 2019; Mamo, 2020; Terekhina et al., 2021). Undernutrition and metabolic disturbances associated with overnutrition and obesity due to the decreased availability or safety of local and traditional foods and increased dependency on imported substitutes affect many Indigenous Peoples worldwide (Amstislavski et al., 2013; Zavaleta et al., 2018; Houde et al., 2020; Jones et al., 2020; Akande et al., 2021; Bogdanova et al., 2021; Bryson et al., 2021) and are especially severe for pregnant women and small children (Mamo, 2020; Olson and Metz, 2020; Bryson et al., 2021); these are amplified by the combination of warming and the COVID-19 situation (Zavaleta-Cortijo et al., 2020). Decreased access to wild plants and animals as food sources and medicine due to climate change is another threat to the health and wellness of indigenous communities (Greenwood and Lindsay, 2019; Mamo, 2020; CIAT and and, 2021; Rankoana, 2021; Teixidor-Toneu et al., 2021).
Tertiary effects relate to culture-wide changes, for example, all forms of malnutrition due to climate-driven changes in food systems and anxiety, mental illness and suicidal thoughts related to cultural and spiritual losses. A wide range of tertiary, culture-related effects of climate change have been documented for Indigenous Peoples. These include anxiety, distress and other mental health impacts due to direct and indirect processes of dispossession of land and culture related to the combination of climate change and other factors (Richmond and Ross, 2009; Bowles, 2015; Norton-Smith et al., 2016 ; Jaakkola et al., 2018; Fuentes et al., 2020; Mamo, 2020; Middleton et al., 2020b; Middleton et al., 2020a; Olson and Metz, 2020; Timlin et al., 2021). Increased risks of conflict and abuse, including violence and homicide against females, and/or conflicts resulting from environmental activism, are other tertiary health threats for Indigenous Peoples (Mamo, 2020). Between 2017 and 2019, close to 500 indigenous people were killed for activism in 19 different countries (Mamo, 2020). In Uganda, climate change drives indigenous men to increase their distance and time from home and their families in search of water and food, leading to an increase in sexual violence against indigenous women and girls in their communities (Mamo, 2020).
Gender inequities amplify the tertiary health effects of climate change (Williams, 2018; Garnier et al., 2020). In an Inuit community, for instance, women reported a higher level of mental stress related to climate change than men (Harper et al., 2015). Adverse pregnancy outcomes and altered developmental trajectories have also been associated with climate change (Hall et al., 2021). Indigenous Batwa women in Uganda reported experiencing more severe circumstances of food insecurity during pregnancy due to drought and unpredictable seasons negatively impacting agricultural practices (de Leon-Martinez et al., 2020). More studies with a gender perspective on climate change as a determinant of Indigenous Peoples’ health are needed, along with the perspectives of indigenous children and youth, displaced individuals and communities in urban settings (Kowalczewski and Klein, 2018).
Box 7.1
Because cultural continuity is a recognised health factor (Lemelin et al., 2010; de Leon-Martinez et al., 2020; Middleton et al., 2020b), displaced Indigenous Peoples may suffer from climate change by worrying about impacts on non-displaced relatives and family and from traditional food staples turning into expensive commodified products. This is a knowledge gap with lasting implications not only on physical environments (Guo et al., 2018). Social connections and knowledge pathways are disrupted, leading to a decreased ability to share locally harvested and cultivated foods (King and Furgal, 2014; Neufeld et al., 2020).
Tertiary effects of climate change on Indigenous Peoples’ health are primarily described in smaller case studies and not designed in a way allowing for systematic international comparisons, which represents an important and significant gap in our understanding of these often-complex associations and impacts (Middleton et al., 2020b).
Future Risks for Indigenous People’s Health and Well-Being in a Changing Climate
Future risks for Indigenous Peoples’ health and well-being in a changing climate will result foremost from exacerbations of observed impacts. Primary and secondary health risks are expected to increase as the frequency and/or severity of climate hazards grow in many regions. As one example, melting permafrost in the Siberian Arctic is projected to lead to more outbreaks of anthrax (Bogdanova et al., 2021). Tertiary health threats are expected to persist even with strong global initiatives to mitigate greenhouse gases (GHGs) (Butler and Harley, 2010). Climate change is expected to compound non-climatic processes that lead to social exclusion and land dispossession that underlay health inequalities experienced by Indigenous Peoples (Huber et al., 2020a).
Options and Opportunities for Reducing Future Risks and Building Capacity/Resilience for Indigenous Peoples’ Health and Well-Being
Indigenous organisations worldwide stress the importance of applying a rights-based approach in responding to climate change (Mamo, 2020). Although Indigenous Peoples are often identified as being vulnerable to climate change, this framing does not always reflect the diverse responses and adaptations of Indigenous Peoples to these ongoing challenges (Nursey-Bray et al., 2020). An emerging body of research is focusing on the strength and resilience of indigenous communities globally as they adapt to these complex changes (Whyte, 2018; FAO et al., 2021).
During droughts and water shortages, for example, indigenous pastoralists may face additional challenges if water supply assistance provides only for human needs and neglects water requirements of livestock (Mamo, 2020). Indigenous knowledge on how to adapt to drought through storing and sharing strategies, for example, is valuable (Fatehpanah et al., 2020; Mamo, 2020).
Indigenous Peoples have been adapting to changes in their environments since time immemorial by developing new practices and techniques (FAO et al, 2021). Their beliefs, value systems and principles include core elements and common values such as reciprocity, solidarity, co-responsibility and community that are expressed in the dynamism of their knowledge systems (Lewis et al., 2020; Schramm et al., 2020b). The relevance of these knowledge systems, which are holistic and tied to relationships between all living things, cannot be ignored at this critical time (Garnier et al., 2020).
The health and equity impacts of climate change for Indigenous Peoples make mitigation efforts critical (Jones et al., 2020), including policies and actions that consider the effects of colonisation. Colonisation constrains the design and diversity of potential climate and health responses through its historic and ongoing suppression of Indigenous knowledge systems that are critical in supporting community-led actions to reduce future risks (Billiot et al., 2019; Reid et al., 2019; Nursey-Bray et al., 2020).
Four Brief Case Studies to Illustrate the Innovativeness of Indigenous Peoples’ Adaptation to Climate Risks
Bedouin Pastoralists’ Grazing Practices Decrease the Risk of Wildfires in Israel and Increase Food Sovereignty
Wildfires are a main cause of deforestation in Israel, and in recent years climate stress has decreased the forest resilience to fires (Klein et al., 2019). The original landscape, a shrubland or maquis consisting mostly of oak and Pistacia, has been used since time immemorial as grazing land for goats, sheep and camels belonging to Indigenous Bedouin people (Degen and El-Meccawi, 2009). Competing land use has reshaped the landscape with pine monocultures and cattle farming, reducing the availability of land suitable for herding goats the indigenous way (Perevolotsky and Sheffer, 2011). In addition, since 1950, plant protection legislation has decreased Bedouin forest pastoralism in Israel by defining indigenous black goats as an environmental threat (FAOLEX, 2021). In nature reserves where no human interference has been allowed, these areas have regenerated into herbaceous shrublands susceptible to wildfires (Turco et al., 2017). Meanwhile, urbanised Bedouin exist on lower incomes and experience higher levels of unemployment compared to other citizens, and some keep non-pastoralised livestock in cities as a strategy for food sovereignty (Degen and El-Meccawi, 2009). In 2019, many severe wildfires occurred in Israel due to extreme heatwaves and, in response, plant protection legislation was repealed, allowing Bedouin pastoralists to graze their goats in areas from which they had been excluded. The amount of combustible undergrowth subsequently decreased, reducing the risk for wildfire and their related impacts, while simultaneously facilitating indigenous food sovereignty among the Bedouin (Mamo, 2020).
Box 7.1
Gardening in the Ashes of Wildfires in the Pacific Northwest as a Strategy to Decrease Food Insecurity and Increase Connections With the Land
In the central interior of what is now known as British Columbia (BC), 2017 was an especially severe wildfire season, with over 1.3 million hectares of land burned and 65,000 people displaced (Timler and Sandy, 2020). The unceded and ancestral lands of the Tsilhqot’in, Dakelh and Secwépemc were impacted by two of the largest fires (Verhaeghe et al., 2017). Communities affected by the BC wildfires subsequently started indigenous gardens closer to home, to protect medicine and food plants and thereby sustaining relationships with these plants, the land and the community (Timler and Sandy, 2020). As there are cultural teachings for fire to cleanse the territory and the land, community members and plants previously isolated became better connected because of the wildfires. The regrowth of plants is part of the healing relationship between plants, people and other animals (Timler and Sandy, 2020). The wildfires were seen as events to catalyse action and emphasise the importance of relationships to support foodways and gardening as responsibility.
Widening our understanding of gardening in the face of climate change and colonialism can support health and healing for Indigenous and non-Indigenous Peoples. Gardening as a means of indigenous food sovereignty has long been utilised by a variety of indigenous groups within Canada and elsewhere to address circumstances of chronic food insecurity and support health and wellness (Johnson-Jennings et al., 2020; Timler and Sandy, 2020). The concept of gardening as both a Euro-Western agricultural practice and indigenous practice encourages an increased reverence and connection with the land and wider engagement with the natural world (Whyte, 2018). Much of this is because Indigenous knowledge and land management practices encompass processes that are known to be synergistic and sustainable (Ottenhoff, 2021). Indigenous worldviews offer a different perspective on social resilience to environmental change, one that is based on moral relationships of responsibility that connect humans to animals, plants and habitats (Grey and Patel, 2015). These responsible practices not only ensure ecosystems are maintained for future generations; they centre the moral qualities necessary to carry out the responsibilities of consent, reciprocity and trust. Moral qualities of responsibility are the foundation for relying on each other when facing environmental challenges (Whyte, 2018; Miltenburg et al., 2021).
To restore these sustainable relationships, a resurgence is needed of community roles and responsibilities (Cidro et al., 2015) as well as a reconsideration of the concept of food security and the role of gardening within diverse indigenous contexts. Offering individual or community gardening as a solution to ‘food insecurity’, a Eurocentric measure of health, ignores colonial contexts and sovereignty (Borrows, 2019; Timler and Sandy, 2020). Indigenous communities have historic, ongoing and evolving gardening and food gathering practices, including a wide variety of land-based and aquatic foods (Turner and Turner, 2008; Mt. Pleasant, 2016). Euro-Western science is beginning to recognise these longstanding relationships (Kamal et al., 2015; Hatfield et al., 2018; Timler and Sandy, 2020). For many indigenous communities, reconnecting with ancestral foodways holds the potential not only to address food security but to provide the community cohesion, self-esteem and wellness (Gordon et al., 2018).
Box 7.1
A New Food Composition Database in Uganda to Guide Local Policy in Healthy Eating Based on Indigenous Foods
In sub-Saharan Africa, climate change is an emerging risk factor for undernutrition, particularly in countries that rely on subsistence agriculture (Sorgho et al., 2020). In Uganda, negative health effects associated with climate change are being observed, including increased rates of food insecurity, with the highest rates recorded among the Batwa of Kanungu District, where 97% of households are severely food insecure (Patterson et al., 2017). For many Indigenous Peoples, food security in a changing climate is a growing concern (Guyot et al., 2006; Patterson et al., 2017). Locally harvested indigenous foods have been adversely impacted by climate change, while connection to land is being disrupted by the processes of colonisation, discrimination and lack of representation in decision-making groups, thereby restricting adaptive capacity for indigenous communities (Bryson et al., 2021). In Uganda, the Indigenous Batwa have experienced significant disparities resulting from the forced eviction from their territory, dispossessing them of their land and the ability to provide indigenous foods to their families (Patterson et al., 2017; Scarpa et al., 2021).
Nutrient-specific knowledge of indigenous foods is limited among many communities in Africa . A new food composition database in Uganda was constructed in dialogue with knowledge keepers from the Batwa and Bakiga Peoples to assess the nutrient density of these locally harvested foods (Scarpa et al., 2021). As in other lower resource settings, no food composition tables are available for southwestern Uganda. The only existing food database was designed for central and eastern Uganda; it does not include common recipes and local foods consumed by Batwa and Bakiga communities (Scarpa et al., 2021). Using a community-based approach and collaboration with local nutritionists, a list of foods was collected through focus group discussions, an individual dietary survey and market assessments. Including these locally familiar foods ultimately supports a focus on indigenous justice and the importance of valuing indigenous food systems and practices, which in many contexts have been found to have superior nutritional and environmental benefits for communities (Kuhnlein et al., 2013; Scarpa et al., 2021). This new and unique database including indigenous foods will not only guide local nutrition and health initiatives, but also contribute towards policies related to indigenous food sovereignty and resilience to climate change.
Decreased Fragmentation of Winter Grazing Increases Mental and Spiritual Well-Being in Reindeer Herding Sámi and Decreases their Dependency on Fossil Fuels
Sami are the Indigenous Peoples of northernmost Scandinavia and the Kola Peninsula of Russia, whose livelihoods have been traditionally sustained by reindeer herding, hunting, fishing and small-scale farming (Nilsson et al., 2011). Climate change is threatening core conditions for reindeer herding, with Sami pastoralists describing the situation as ‘facing the limit of resilience’ (Furberg et al., 2011). Sami pastoralists stress that an ability to continue reindeer herding is a prerequisite for their mental and spiritual health (Jaakkola et al., 2018).
In a pilot project for climate adaptation of reindeer herding run by the Swedish Sami Parliament, reindeer herding management plans (in Swedish, renbruksplaner) were used as a tool to develop strategies for climate adaptation (Walkepää, 2019). Four Sami reindeer herding cooperatives participated in the pilot study. They all agreed that climate change means that grazing patterns need to change. Traditionally, mountain reindeer graze in the Scandinavian mountains close to Norway in summer and in the coastal areas close to the Gulf of Bothnia in winter, representing a total migration route of up to 400 kilometres one-way. Rising temperatures are causing spring to occur earlier in the coastal winter grazing land before the calving areas in the summer land are suitable for grazing and free from snow. When the snow cover disappears, the herds are dispersed, so it is important to migrate while snow is still present (Walkepää, 2019). Migration routes are being destabilised by weaker ice cover on water and by hazardous weather events. Competing land use due to infrastructure, extractive industries, tourism, and energy production makes it difficult to find alternative grazing land. Supplementary feeding and increased use of trucks to transport reindeer is one result. Herds that are dispersed due to bad snow conditions have an increased exposure to predators (Walkepää, 2019; Uboni et al., 2020). By working strategically to secure adequate winter grazing and reduce fragmentation of grazing areas more generally represents win-win strategies for achieving decreased mental stress levels while reducing herders’ consumption of fossil fuels (Walkepää, 2019).
Box 7.1
7.1.8 Visual Guide to this Chapter
Figure 7.3 provides a visual guide to this chapter. Section 7.1 has briefly summarised major global frameworks and highlights groups that exhibit heightened vulnerability and exposure to the climatic risks assessed in this chapter. Section 7.2 assesses observed impacts on health and well-being, migration and conflicts that have emerged from interactions of climate and weather-related hazards, exposure to such hazards and vulnerability of communities and systems, while Section 7.3 assesses projected future risks. Section 7.4 assesses adaptation responses to climate risks, opportunities for transformative change, co-benefits and how solutions for reducing climate impacts on health, well-being, migration and conflicts may form part of the wider CRDPs.
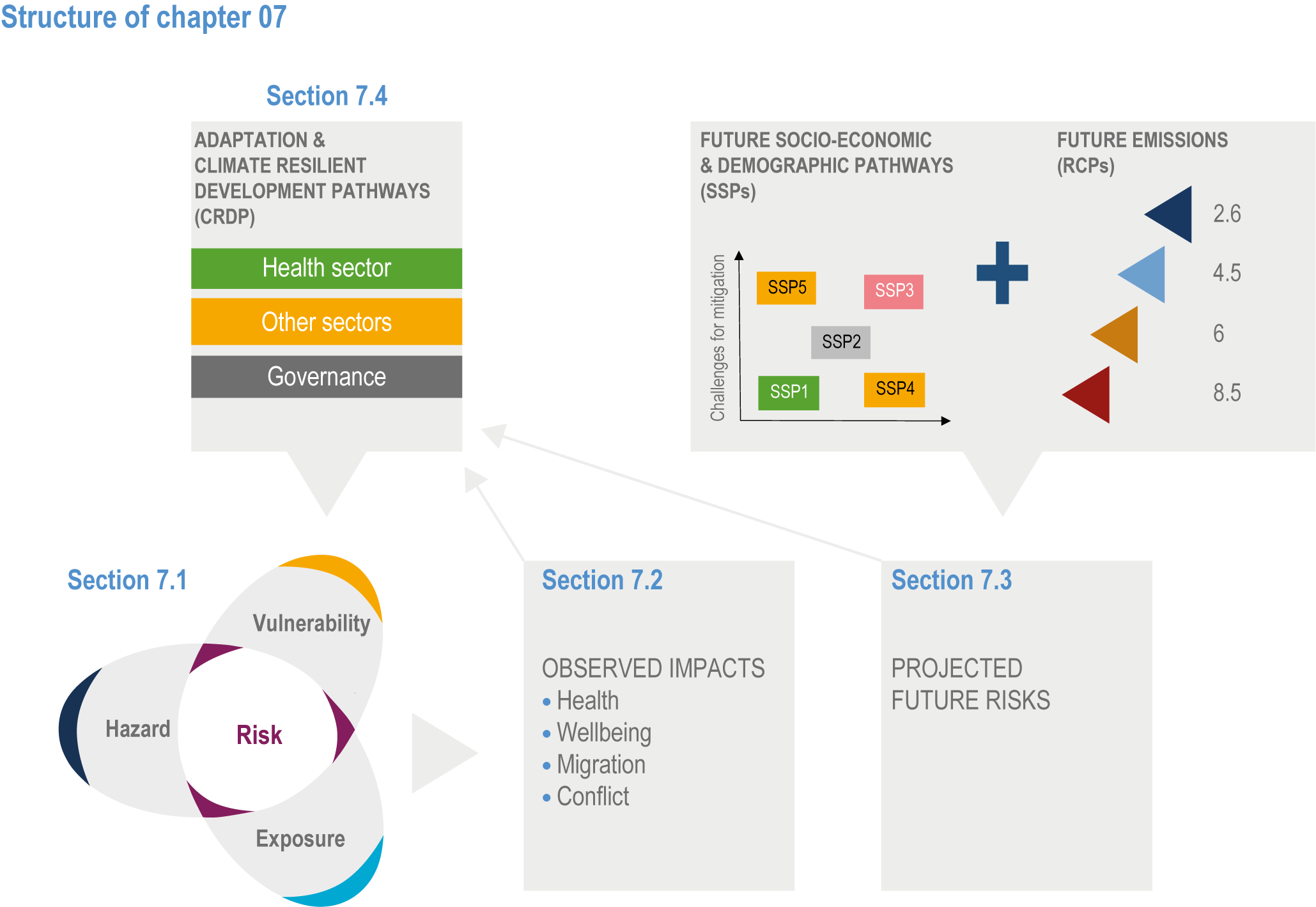
Figure 7.3 | Structure of the chapter following a pathway from hazard, exposure and vulnerability to the observed impacts, projected future risks, adaptation and climate resilient development pathways.
7.2. Observed Impacts of Climate Change on Health, Well-Being, Migration and Conflict
7.2.1 Observed Impacts on Health and Well-Being
Eleven categories of diseases and health outcomes have been identified in this assessment as being climate-sensitive through direct pathways (e.g., heat and floods) and indirect pathways mediated through natural and human systems and economic and social disruptions (e.g., disease vectors, allergens, air and water pollution, and food system disruption) (high confidence). A key challenge in quantifying the specific relationship between climate and health outcomes is distinguishing the extent to which observed changes in prevalence of a climate-sensitive disease or condition are attributable directly or indirectly to climatic factors as opposed to other non-climatic causal factors (Ebi et al., 2020). A subsequent challenge is then determining the extent to which those observed changes in health outcomes associated with climate are attributable to events or conditions associated with natural climate variability compared to persistent human induced shifts in the mean and/or the variability characteristics of climate (i.e., anthropogenic climate change). The context within which the impacts of climate change affect health outcomes and health systems is described in this chapter as being a function of risk, which is in turn a product of interactions between hazard, exposure and vulnerability (Chapter 1), with the impacts in turn having the potential to reinforce vulnerability and/or exposure to risk (Figure 7.4).
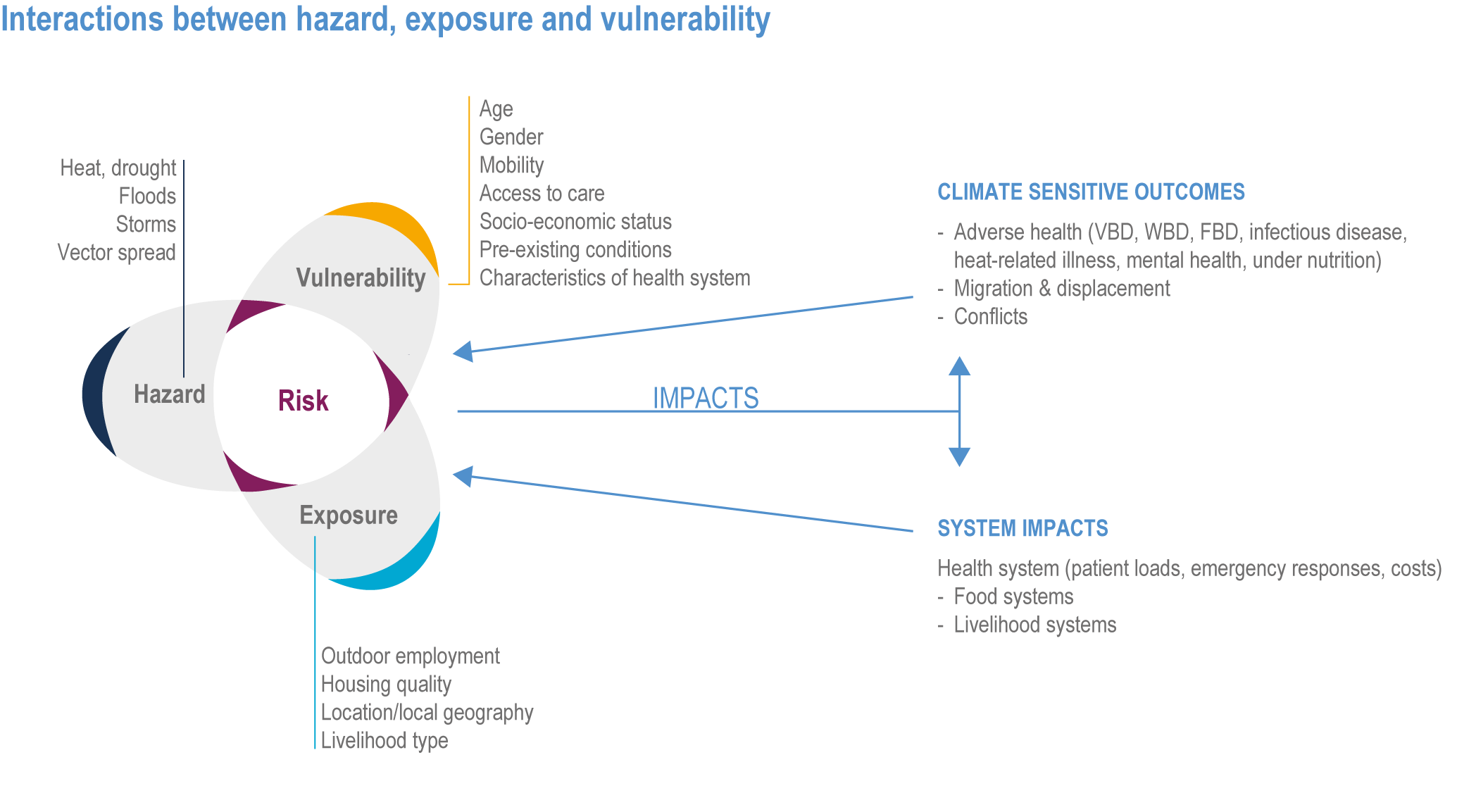
Figure 7.4 | Interactions between hazard, exposure and vulnerability that generate impacts on health systems and outcomes, with selected examples. WBD: waterborne disease, VBD: Vector-borne disease, and FBD: Food-borne disease.
Box 7.2 | The Global Burden of Climate-Sensitive Health Outcomes Assessed in this Chapter
Global statistics for death and loss of health are increasingly described in terms of burden, which describes gaps between a population’s actual health status and what its status would be if its members lived free of disease and disability to their collective life expectancy (Shaffer et al., 2019). Burden for each disease/health outcome is estimated by adding together the number of years of life lost (YLL) by a person because of early death and the number of years of life lived with disability (YLD) from the considered outcome. The resulting statistic, the disability-adjusted life year (DALY) represents the loss of one year of life lived in full health. The total global burden of disease (Vos et al., 2020), expressed in DALYs, is what the world’s health systems must manage and is reported annually in Global Burden of Disease Study (Vos et al., 2020). The estimated current global burden of climate-sensitive diseases and conditions described in this chapter, and the geographical regions most affected, are summarised in Table Box 7.2.1. As was observed in Chapter 11 (‘Human Health’) of AR5, the ‘background climate-related disease burden of a population is often the best single indicator of vulnerability to climate change – doubling of risk of disease in a low disease population has much less absolute impact than doubling of the disease when the background rate is high.’
The global magnitude of climate-sensitive diseases was estimated in 2019 to be 39,503,684 deaths (69.9% of total annual deaths) and 1,530,630,442 DALYs (Vos et al., 2020). Of these, cardiovascular diseases (CVDs) comprised the largest proportion of climate-sensitive diseases (32.8% of deaths and 15.5% DALYs). The next largest category consists of respiratory diseases – with chronic respiratory disease contributing to 7% of deaths and 4.1% of DALYs and respiratory infection and tuberculosis contributing to 6.5% of deaths and 6% of DALYs. The observed trend of climate-sensitive disease deaths since 1990 is marked by increasing cardiovascular mortality and decreasing mortality from respiratory infections, enteric diseases and other infectious diseases (Vos et al., 2020). Figure Box 7.2.1 illustrates specific global trends between 1990 and 2017 of selected health outcomes estimated by GBDs (Ahmad Kiadaliri et al. 2018).
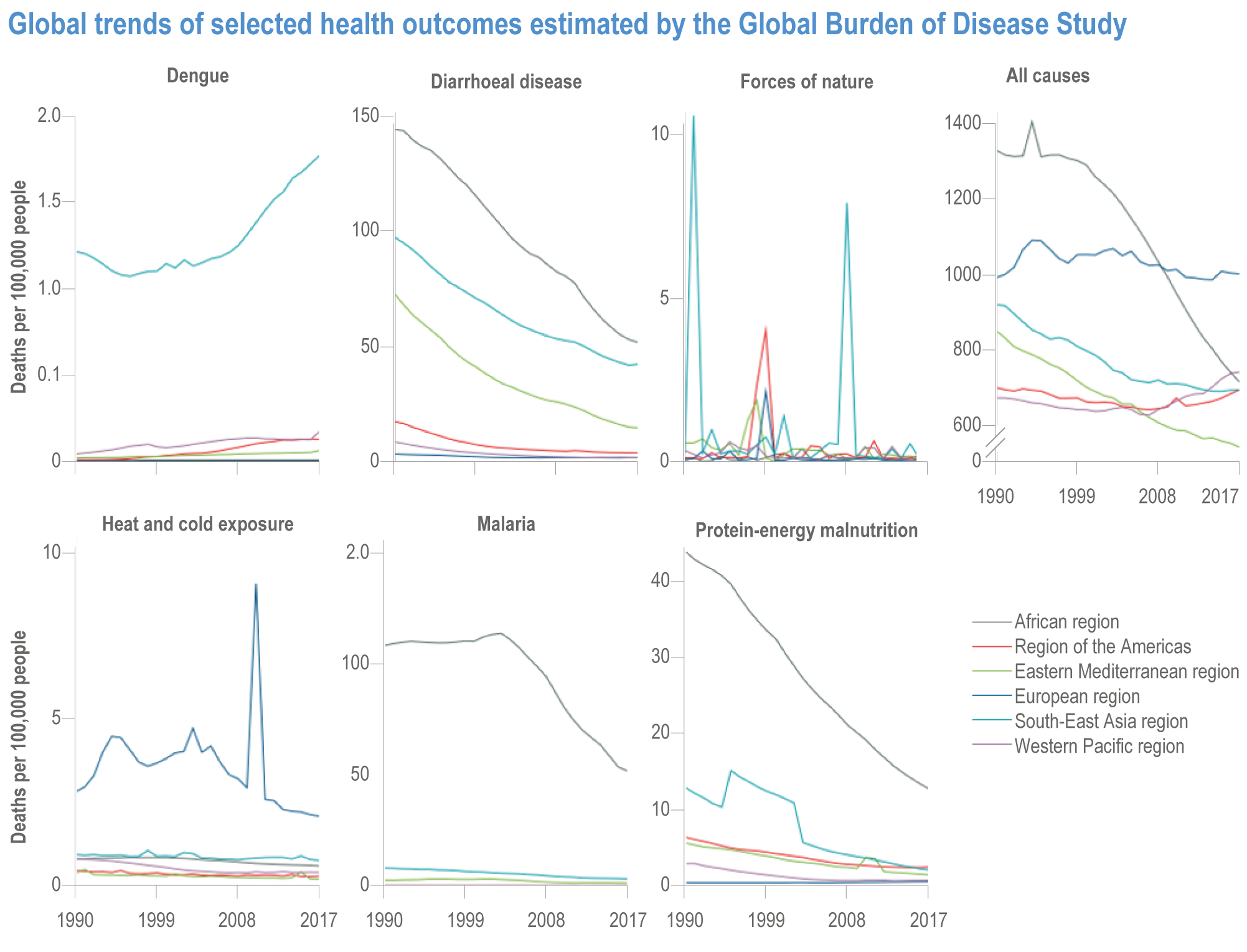
Figure Box 7.2.1 | Global trends of selected health outcomes estimated by GBDs. Source: Ahmad Kiadaliri et al. (2018a).
Table Box 7.2.1 | Global burden of climate-sensitive health risks assessed in this chapter (in order of assessment) (Vos et al., 2020) and synthesis of major observed and projected impacts in most affected regions. Blue represents an increase in positive health impacts, green represents an increase in negative health impacts and yellow represents an increase in both positive and negative impacts, but not necessarily in equal proportions. The confidence level refers to both the attributed observed and projected changes to climate change. No assessment means the evidence is insufficient for assessment.
Data from Global Burden of Disease 2019 (Vos et al. 2020) | Chapter 7 Assessment | ||||
Health outcome (disease/condition) | Global annual deaths | Regions most affected (deaths) | Climate change observed impacts | Climate change projected impacts in most affected regions | Selected key references of the Assessment |
Malaria | 643,381 | Africa (92%) | **** | *** | M’Bra et al. (2018); Caminade et al. (2019); Gibb et al. (2020); Tompkins and Caporaso (2016b); Ebi et al. (2021a) |
Dengue | 36,055 | Asia (96%) | *** | *** | Bhatt et al. (2013); Rocklöv & Dubrow (2020); Messina et al. (2019); Monaghan et al. (2018) |
Diarrhoeal diseases | 1,534,443 | Asia (56%) | *** | ** | Cissé (2019); Levy et al. (2018); Lo Iacono et al. (2017); Carlton et al. (2016) |
Salmonella | 79,046 | Africa (89%) | *** | ** | Cissé (2019); Smith and Fazil (2019); Lake (2017) |
RTIs | 2,493,200 | Asia (47%) | ** | Geier et al. (2018); Oluwole (2017) | |
Non-communicable respiratory illness | 3,741,705 | Asia (74%) | *** | ** | Schweitzer et al. (2018); Hansel et al. (2016); Collaco et al. (2018); D’Amato et al. (2020); Silva et al. (2017); Doherty et al. (2017); Beggs (2021) |
CVD | 18,562,510 | Asia (58%) | ** | *** | Stewart et al. (2017); Phung (2016); Sun (2018); Wang (2016); Tian (2019); Chen (2019); Zhang (2018) |
Death from malignant neoplasms | 10,079,637 | Asia (55%) | *** | Ahmed et al. (2014); Modenese et al. (2018); Prueksapanich et al. (2018) | |
Diabetes | 1,551,170 | Asia (56%) | ** | ** | Hajat et al. (2017); Xu et al. (2019b); Li et al. (2014);Yang et al. (2016); Velez-Valle et al. (2016); Quast and Feng (2019) |
Environmental heat and cold exposure | 47,461 | Asia (46%) | *** | **** | Zhang et al. (2019b); Green et al. (2019); Murray et al. (2020); Ma and Yuan (2021); Jones et al. (2018); Russo et al. (2019); Gosling et al. (2017) |
Nutritional deficiencies | 251,577 | Africa (43%) | *** | *** | Mbow et al. (2019); Lloyd (2018); Springmann et al. (2016b); Zhu et al. (2018); Weyant et al. (2018) |
Mental healtha | n.a. | n.a. | **** | **** | Cianconi et al. (2020); Charlson et al. (2021); Hayes and Poland (2018); Hrabok et al. (2020); Obradovich et al. (2018) |
Legend | |||||
Climate change impacts | Confidence | ||||
Positive health impacts | Very high | **** | |||
Negative health impacts | High | *** | |||
Positive and negative impacts | Medium | ** | |||
No assessment | Low | * | |||
Notes:
(a) Mental health data were not available (n.a.) due to lack of information in GBD 2019 related to annual deaths and the most affected regions.
7.2.2 Observed Impacts on Communicable Diseases
7.2.2.1 Observed Impacts on Vector-Borne Diseases
Climate-sensitive VBDs include mosquito-borne diseases, rodent-borne diseases and tick-borne diseases. Many infectious agents, vectors, non-human reservoir hosts, and pathogen replication rates can be sensitive to ambient climatic conditions. Elevated proliferation and reproduction rates at higher temperatures, longer transmission season, changes in ecology and climate-related migration of vectors, reservoir hosts or human populations contribute to this climate sensitivity (Rocklöv & Dubrow, 2020; Semenza and Paz, 2021). Age-standardised DALY rates for many VBDs have decreased over the last decade due to factors unrelated to climate. Vulnerability to VBD is strongly determined by sociodemographic factors (e.g., children, the elderly and pregnant women are at greater risk) with exposure to vectors being strongly influenced by various factors including socioeconomic status, housing quality, healthcare access, susceptibility, occupational setting, recreational activity, conflicts and displacement ( Rocklöv & Dubrow, 2020; Semenza and Paz, 2021). Figure 7.5 illustrates how climatic and non-climatic drivers and responses determine VBD outcomes.
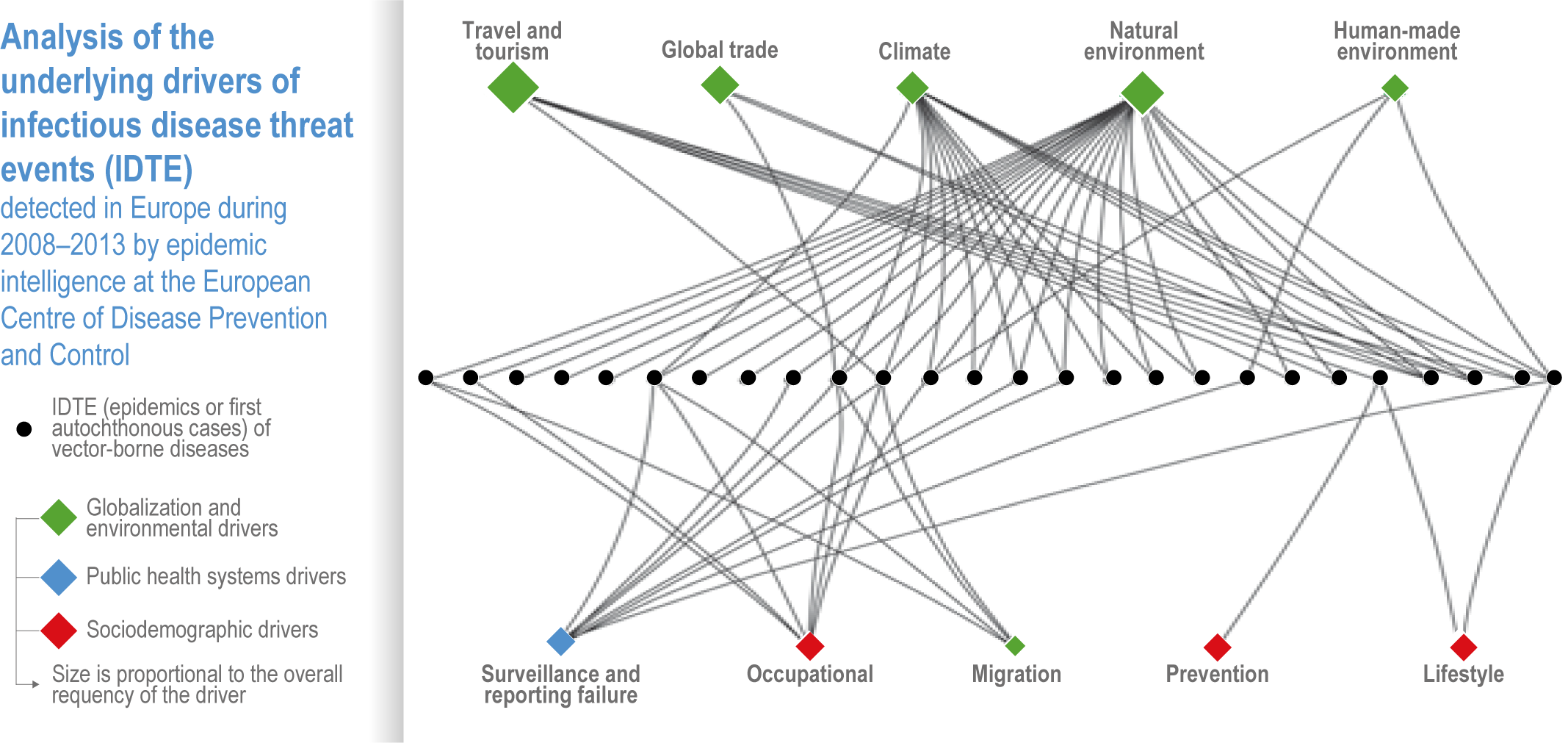
Figure 7.5 | Analysis of the underlying drivers of infectious disease threat events (IDTEs) detected in Europe from 2008 to 2013 by epidemic intelligence at the European Centre of Disease Prevention and Control. Seventeen drivers were identified and categorised into three groups: globalisation and environment (green), sociodemographic (red) and public health system (blue). The drivers are illustrated as diamond shapes and arranged in the top and bottom row; the sizes are proportional to the overall frequency of the driver. Here IDTEs (epidemics or first autochthonous cases) of VBDs are illustrated as a horizontal row of dots in the middle. These empirical data include the IDTEs of VBDs such as West Nile fever, malaria, dengue fever, chikungunya and Hantavirus infection. Source: Semenza et al. (2016).
Evidence has increased since AR5 that the vectorial capacity has increased for dengue fever, malaria and other mosquito-borne diseases and that higher global average temperatures are making wider geographic areas more suitable for transmission (very high confidence). Transmission rates of malaria are directly influenced by climatic and weather variables such as temperature, with non-climatic socioeconomic factors and health system responses counteracting the climatic drivers (very high confidence). The burden of malaria is greatest in Africa, where more than 90% of all malaria-related deaths occur (M’Bra et al., 2018; Caminade et al., 2019). Between 2007 and 2017, DALYs for malaria have decreased by 39% globally. Malaria is mainly caused by five distinct species of plasmodium parasite (Plasmodium falciparum, Plasmodium vivax, Plasmodium malariae, Plasmodium ovale and Plasmodium knowlesi) and is transmitted by Anopheline mosquitoes. Evidence suggests that in highland areas of Colombia and Ethiopia, malaria has shifted in warmer years towards higher altitudes, indicating that, without intervention, malaria will increase at higher elevations as the climate warms (Siraj et al., 2014; Midekisa et al., 2015). Each year, local outbreaks of malaria occur due to importation in areas from which it was once eradicated, such as Europe, but the risk of re-establishment is considered low.
The transmission of dengue fever is linked to climatic and weather variables such as temperature, relative humidity and rainfall (high confidence). The dengue virus is carried and spread by Aedes mosquitoes, primarily Aedes aegypti. Dengue has the second highest burden of VBDs, with the majority of deaths occurring in Asia (Bhatt et al., 2013). Since 1950, global dengue burden has grown and is attributable to a combination of climate-associated expansion in the geographic range of the vector species and non-climatic factors such as globalised air traffic, urbanisation and ineffective vector abatement measures. Temperature, relative humidity and rainfall variables are significantly and positively associated with increased dengue case incidence and/or transmission rates globally, including in Vietnam (Phung et al., 2015; Xuan le et al., 2014), Thailand (Xu et al., 2019a), India (Mutheneni et al., 2017; Rao et al., 2018; Mala and Jat, 2019), Indonesia (Kesetyaningsih et al., 2018), the Philippines (Carvajal et al., 2018), the USA (Lopez et al., 2018; Pena-Garcia et al., 2017; Duarte et al., 2019; Rivas et al., 2018; Silva et al., 2016a), Jordan (Obaidat and Roess, 2018) and Timor-Leste (Wangdi et al., 2018). Variation in winds, sea surface temperatures and rain over the tropical eastern Pacific Ocean (El Niño-Southern Oscillation; ENSO) have been linked to increased dengue incidence in Colombia (Quintero-Herrera et al., 2015; McGregor and Ebi, 2018; Pramanik et al., 2020) and its interannual variation successfully forecasted in Ecuador using ENSO indices as predictors (Petrova et al., 2019). The observed time lag between climate exposures and increased dengue incidence is approximately 1–2 months (Chuang et al., 2017; Lai, 2018; Chang et al., 2018).
Changing climatic patterns are facilitating the spread of CHIKV, Zika, Japanese encephalitis and Rift Valley Fever in Asia, Latin America, North America and Europe (high confidence). Climate change may have facilitated the emergence of CHIKV as a significant public health challenge in some Latin American and Caribbean countries (Yactayo et al., 2016; Pineda et al., 2016) and contributed to chikungunya outbreaks in Europe (Rocklöv et al., 2019; Mascarenhas et al., 2018; Morens and Fauci, 2014). The Zika virus outbreak in South America in 2016 was preceded by 2007 outbreaks on Pacific islands and followed a period of record high temperatures and severe drought conditions in 2015 (Paz and Semenza, 2016; Tesla et al., 2018). Increased use of household water storage containers during the drought is correlated with a range expansion of Aedes aegypti during this period, increasing household exposure to the vector (Paz and Semenza, 2016). Changing climate also appears to be a risk factor for the spread of Japanese encephalitis to higher altitudes in Nepal (Ghimire and Dhakal, 2015) and in southwest China (Zhao et al., 2014). In eastern Africa, climate change may be a risk factor in the spread of Rift Valley Fever (Taylor et al., 2016a).
Changes in temperature, precipitation, and relative humidity have been implicated as drivers of West Nile fever in southeastern Europe (medium confidence). The average temperature and precipitation prior to the exceptional 2018 West Nile outbreak in Europe was above the 1981–2010 period average, which may have contributed to an early upsurge of the vector population (Marini et al., 2020; Haussig et al., 2018; Semenza and Paz, 2021). In 2019 and 2020, West Nile fever was first detected in birds and subsequently in humans in Germany and the Netherlands (Ziegler et al., 2020; Vlaskamp et al., 2020).
Climate change has contributed to the spread of the Lyme disease vectorIxodes scapularis , a corresponding increase in cases of Lyme disease in North America (high confidence) and the spread of the Lyme disease and tick-borne encephalitis vectorIxodes ricinus in Europe (medium confidence). In Canada, there has been a geographic range expansion of the black-legged tick I. scapularis, the main vector of Borrelia burgdorferi, the agent of Lyme disease. Vector surveillance of I. scapularis has identified strong correlation between temperatures and the emergence of tick populations, their range and recent geographic spread, with recent climate warming coinciding with a rapid increase in human Lyme disease cases (Clow et al., 2017; Cheng et al., 2017; Gasmi et al., 2017; Ebi et al., 2017). Ixodes ricinus, the primary vector in Europe for both Lyme borreliosis and tick-borne encephalitis is sensitive to humidity and temperature (Daniel et al., 2018; Estrada-Peña and Fernández-Ruiz, 2020) (high confidence). There has been an observed range expansion to higher latitudes in Sweden and to higher elevations in Austria and the Czech Republic.
Rodent-borne disease outbreaks have been linked to weather and climate conditions in a small number of studies published since AR5, but more research is needed in this area . In Kenya, a positive association exists between precipitation patterns and Theileria-infected rodents, but for Anaplasma, Theileria and Hepatozoon, the association between rainfall and pathogen varies according to rural land use types (Young et al., 2017). Weather variability plays a significant role in transmission rates of haemorrhagic fever with renal syndrome (HFRS) (Hansen et al., 2015; Xiang et al., 2018; Liang et al., 2018; Fei et al., 2015; Xiao et al., 2014; Vratnica et al., 2017; Roda Gracia et al., 2015; Monchatre-Leroy et al., 2017; Bai et al., 2019). In Chongqing, HFRS incidence has been positively associated with rodent density and rainfall (Bai et al., 2015).
7.2.2.2 Observed Impacts on Waterborne Diseases
Important waterborne diseases (WBDs) include diarrhoeal diseases (such as cholera, shigella, cryptosporidiosis and typhoid), schistosomiasis, leptospirosis, hepatitis A and E and poliomyelitis (Cisse, 2019; Houéménou et al., 2021; Hassan et al., 2021; Archer et al., 2020; Mbereko et al., 2020; Fan et al., 2021). The number of cases of WBDs is considerable, and even in high-income countries WBDs continue to be a concern (Cissé et al., 2018; Kirtman et al., 2014; Levy et al., 2018; Murphy et al., 2014; Brubacher et al., 2020; Lee et al., 2021). Nevertheless, diarrhoea mortality has declined substantially since 1990, although there are variations by country, and the global burden of WBDs has decreased in line with vaccination coverage of some WBDs (such as polio and cholera), poverty reduction and improved sanitation and hygiene (Jacob and Kazaura, 2021; Mutono et al., 2020; Lee et al., 2019; Semenza and Paz, 2021; Jacob and Kazaura, 2021; Mutono et al., 2020).
Drinking water containing pathogenic microorganisms is the main driver of the burden of WBDs (Murphy et al., 2014; Lee et al., 2021; Chen et al., 2021b; Musacchio et al., 2021). WBD outbreaks, particularly intestinal diseases, are attributable to a combination of the presence of particular pathogens (bacteria, protozoa, viruses or parasites) and the characteristics of drinking water systems in a given location (Bless et al., 2016; Ligon and Bartram, 2016; Mutono et al., 2021; Ferreira et al., 2021).
Since AR5 there is a growing body of evidence that increases in temperature (very high confidence), heavy rainfall (high confidence), flooding (medium confidence) and drought (low confidence) are associated with an increase of diarrhoeal diseases. In the majority of studies there is a significant positive association observed between WBDs and elevated temperatures, especially in areas where water, sanitation and hygiene (WASH) deficiencies are significant (Levy et al., 2018; Carlton et al., 2016; Levy et al., 2018; Sherpa et al., 2014; Guzman Herrador et al., 2015; Levy et al., 2016; Lo Iacono et al., 2017). In Ethiopia, South Africa and Senegal, increases in temperatures are associated with increases in diarrhoea, while in Ethiopia, Senegal and Mozambique, increases in monthly rainfall are associated with an increase in cases of childhood diarrhoea (Azage et al., 2015; Thiam et al., 2017; Horn et al., 2018). Similar associations between weather and diarrhoea have been observed in Cambodia, China, Bangladesh, Pacific Island countries and the Philippines (McIver et al., 2016a; McIver et al., 2016b; Liu et al., 2018; Wu et al., 2014; Matsushita et al., 2018). Heavy precipitation events have been consistently associated with outbreaks of WBDs in Europe, USA, UK and Canada (Guzman Herrador et al., 2015; Levy et al., 2016; Lo Iacono et al., 2017; Curriero et al., 2001; Guzman Herrador et al., 2016; Levy et al., 2018; Semenza and Paz, 2021).
Impacts of floods include outbreaks of WBDs, with such events disproportionately affecting the young, elderly and immunocompromised (Suk et al., 2020; Guzman Herrador et al., 2015; Levy et al., 2016; Lo Iacono et al., 2017; Zhang et al., 2019a). Water shortage and drought have been found associated with diarrhoeal disease peaks (Epstein et al., 2020b; Subiros et al., 2019; Boithias et al., 2016), while some reviews found insufficient evidence of the effects of drought on diarrhoea (Levy et al, 2016 ; Asmall et al., 2021; Epstein et al., 2020b; Subiros et al., 2019; Boithias et al., 2016; Ramesh et al., 2016).
Heavy rainfall and higher than normal temperatures are associated with increased cholera risk in affected regions (very high confidence). Cholera is an acute diarrhoeal disease typically caused by the bacterium Vibrio cholerae that can result in severe morbidity and mortality. Maximum and minimum temperatures and precipitation have been negatively associated with cholera cases. Cholera outbreaks have occurred in several regions after natural disasters, including cholera incidence increasing three-fold in El Niño-sensitive regions of Africa (Mpandeli et al., 2018; Amegah et al., 2016; Escobar et al., 2015; Jutla et al., 2017; Asadgol et al., 2019; Moore et al., 2018; Moore et al., 2017; Camacho et al., 2018; IPCC, 2019a; Cross-Chapter Box ILLNESS in Chapter 2; Box 3.3).
Heavy rainfall, warmer weather and drought are linked to increased risks for other GI infections (high confidence). As temperature increases, bacterial causes of GI infection also appear to increase, and this association is variably influenced by humidity and rainfall (Ghazani et al., 2018; Levy, 2016). In New York it has been found that every 1°C increase in temperature was correlated with a 0.70–0.96% increase in daily hospitalisation for GI infections (Lin et al., 2016). In the Philippines, leptospirosis and typhoid fever showed an increase in incidence following heavy rainfall and flooding events (Matsushita et al., 2018).
7.2.2.3 Observed Impacts on Food-Borne Diseases
FBDs refer to any illness resulting from ingesting food that is spoiled or contaminated by pathogenic bacteria, viruses, parasites, toxins, pesticides and/or medicines (WHO, 2018b). FBD risks are present throughout the food chain, from production to consumption, and most often arise due to contamination at source and from improper food handling, preparation and/or storage (Smith and Fazil, 2019; Semenza and Paz, 2021). As with WBDs, FBD outbreaks can follow multiple causal pathways as climatic risk factors interact with food production and distribution systems, urbanisation and population growth, resource and energy scarcity, decreasing agricultural productivity, price volatility, modification of diet trends, new technologies and the emergence of antimicrobial resistance (Lake, 2018; Yeni and Alpas, 2017). The burden of FBDs is also linked to malnutrition as reduced immunity increases susceptibility to various food-borne pathogens and toxins (FAO, 2020).
A strong association exists between increases in FBDs and high air and water temperatures and longer summer seasons (very high confidence). The risks occur through complex transmission pathways throughout the food chain and the wide range of food-borne pathogens (Cisse, 2019; Hellberg and Chu, 2016; Lake and Barker, 2018; Park et al., 2018b; Smith and Fazil, 2019). The food-borne pathogens of most concern are those having low infective doses, a significant persistence in the environment and high stress tolerance to temperature change (e.g., enteric viruses, Campylobacter spp., Shiga toxin-producing E. coli strains, Mycobacterium avium, tuberculosis complexes, parasitic protozoa and Salmonella) (Lake, 2018; Lake, 2017; Lake and Barker, 2018; Smith and Fazil, 2019; European Food Safety Authority 2020; Semenza and Paz, 2021). Priority risks include marine biotoxins, mycotoxins, salmonellosis, vibriosis, transfer of contaminants due to extreme precipitation, floods, increased use of chemicals in the food chain (plant protection products, fertilizers, veterinary drugs) and potential residues in food (European Food Safety Authority 2020; World Health Organization 2018b).
There is a strong association observed between the increase in average ambient temperature and increases in Salmonella infections (high confidence). Most types of Salmonella infections lead to salmonellosis, while some other types (SalmonellaTyphi and SalmonellaParatyphi) can lead to typhoid fever or paratyphoid fever. The transmission to humans of the non-typhoidal Salmonella infection, one of the most widespread FBDs, usually occurs through eating foods contaminated with animal faeces. Studies conducted in Australia (Milazzo et al., 2016), New Zealand (Lal et al., 2016), the UK (Lake, 2017), South Korea (Park et al., 2018a; Park et al., 2018c; Park et al., 2018a), Singapore (Aik et al., 2018) and Hong Kong, SAR of China (Wang et al., 2018a; Wang et al., 2018b), have shown that Salmonella outbreaks are strongly associated with temperature increases.
Significant associations exist between FBDs due toCampylobacter , precipitation and temperature (medium confidence). The timing of heat-associated Campylobacteriosis events varies across countries, with infection rates in the UK appearing to decline immediately after periods of high rainfall (Djennad et al., 2019; Lake et al., 2019; Rosenberg et al., 2018; Yun et al., 2016; Weisent et al., 2014). This suggests the association with climate may be indirect and due to weather conditions that encourage outdoor food preparation and recreational activities (Lake, 2017; Semenza and Paz, 2021).
Outbreaks of human and animal Cryptococcus have been reported as being associated with a combination of climatic factors and shifts in host and vector populations (Chang and Chen, 2015 ; Rickerts, 2019). The prevalence of childhood cryptosporidiosis, which is the second leading cause of moderate to severe diarrhoea among infants in the tropics and subtropics, shows associations with population density and rainfall, with contamination due to Cryptosporidium spp. being 2.61 times higher during and after heavy rain (Lal et al., 2019; Young et al., 2015; Khalil et al., 2018). Studies from Ghana, Guinea Bissau, Tanzania, Kenya and Zambia show a higher prevalence of Cryptosporidium during high rainfall seasons, with some peaks observed before, at the onset or at the end of the rainy season (Squire and Ryan, 2017).
7.2.2.4 Respiratory Tract Infections
Climatic risk factors for respiratory tract infections (RTIs) due to multiple pathogens (bacteria, viruses and fungi) include temperature and humidity extremes, dust storms, extreme precipitation events and increased climate variability. Amongst a range of RTIs, pneumonia and influenza represent a significant disease burden (Ferreira-Coimbra et al., 2020; Lafond et al., 2021; McAllister et al., 2019; Wang et al., 2020 c). The drivers of pneumonia incidence are complex and include a range of possible non-climate as well as climate factors. For example, chronic diseases (e.g., lung disease, chronic obstructive pulmonary disease (COPD) and asthma), other comorbidities, a weak immune system, age, gender, community, passive smoking, air pollution and childhood immunisation may confound the climate pneumonia relationship (Miyayo et al., 2021).
In temperate regions, the incidence of pneumonia is higher in winter months, but the exact causes of this seasonality remain debated (Mirsaeidi et al., 2016). With regards to temperature, various J-shaped, U-shaped or V-shaped temperature–pneumonia relationships have been reported in the literature (Huang et al., 2018 ; Kim et al., 2016; Liu et al., 2014; Qiu et al., 2016; Sohn et al., 2019) with such relationships dependent on location. Humidity also appears important but, like temperature, its effect is not consistent across studies – low temperatures and low humidity (Davis et al., 2016), high temperatures and high humidity (Lam et al., 2020) and low temperatures and high humidity (Miyayo et al., 2021) have all been found to be associated with an increased incidence of pneumonia.
Day-to-day variations in temperature also appear important. For Australia, increases in emergency room visits for childhood pneumonia are associated with sharp temperature drops (Xu et al., 2014). Large inter-daily changes in temperature are important for respiratory disease incidence in Guangzhou, China (Lin et al., 2013) and Shanghai (Lei et al., 2021) while rapidly changing and extreme temperatures during pregnancy have been linked to childhood pneumonia (Miao et al., 2017; Zeng et al., 2017; Zheng et al., 2021). In tropical and subtropical areas of Africa and Asia, pneumonia incidence has been reported to be higher during the rainy season, pointing to a positive association between pneumonia patterns and temperature and precipitation (Chowdhury et al., 2018a; Lim and Siow, 2018; Paynter et al., 2010).
The degree to which the timing, duration and magnitude of local influenza virus epidemics is dependent on climate factors is poorly understood (Lam et al., 2020). Further, a host of non-climate confounders are likely to influence the incidence of seasonal influenza (Caini et al., 2018). This poses a number of challenges for making reliable climate-based epidemiological forecasts for influenza (Gandon et al., 2016). Although no association between anomalous climate conditions and influenza have been reported in some locations (Lam et al., 2020), generally, low winter temperatures and humidity in temperate regions and periods of high humidity and precipitation in the tropical and subtropical regions have been linked to outbreaks of influenza (Deyle et al., 2016; Soebiyanto et al., 2015; Tamerius et al., 2013). However, the climate sensitivity of influenza may be more complex than this, with both high and low humidity; the amount and intensity of precipitation; solar activity and/or sunshine; and latitude also being important (Axelsen et al., 2014; Chong et al., 2020b; Geier et al., 2018; Park et al., 2019; Qu, 2016; Smith et al., 2017; Wang et al., 2017 c; Zhao et al., 2018a). Moreover, the shape of the climate variable influenza relationship may be conditioned on influenza type (Chong et al., 2020a). Further, distinct periods of weather variability characterised by rapid inter-daily changes in temperature may act as precursors to influenza epidemics as has been demonstrated for the marked 2017–2018 influenza season and others across the USA (Liu et al., 2020a; Zhao et al., 2018a). For the eastern Mediterranean, such rapid weather changes are associated with the ‘Cyprus Low’, with the timing and magnitude of seasonal influenza related to the interannual frequency of this particular weather regime (Hochman et al., 2021). Potentially, large-scale modes of climatic variability such as ENSO and the Indian Ocean Dipole, which strongly moderate the frequency of weather regimes in some parts of the world, could affect influenza pandemic dynamics. However, studies conducted to date report inconsistent results. Some point to an increased (decreased) severity of seasonal influenza during El Niño (La Niña) (Oluwole, 2015; Oluwole, 2017), while others find influenza to be more severe and frequent when coinciding with La Niña events (Chun et al., 2019; Flahault et al., 2016; Shaman and Lipsitch, 2013). This raises the possibly of non-stationary associations between large-scale modes of climatic variability and influenza dynamics (Onozuka and Hagihara, 2015) as found for other diseases (Kreppel et al., 2014), something that might be expected given El Niño’s time-varying impact on global precipitation and temperature fields and associated impacts on health outcomes (McGregor and Ebi, 2018).
7.2.2.5 Other Water Shortage and Drought-Associated Diseases and Health Outcomes
Water shortage and drought are associated with skin diseases (Schachtel et al., 2021; Lundgren, 2018; Andersen and Davis, 2017; Kaffenberger et al., 2017; Andersen and Davis, 2017), trachoma (Ramesh et al., 2016) and violence (Epstein et al., 2020a); more research is warranted in these areas for future assessment.
Box 7.3 | Cascading Risk Pathways Linking Waterborne Disease to Climate Hazards
The causal linkages between climate variability and change and incidence of WBDs follow multiple direct and indirect pathways, often as part of a cascading series of risks (Semenza, 2020). For example, extreme precipitation can result in a cascading hazard or disease event with implications of greater magnitude than the initial hazard, especially if there are pre-existing vulnerabilities in critical infrastructure and human populations (Semenza and Paz, 2021). Intense or prolonged precipitation can flush pathogens in the environment from pastures and fields to groundwater, rivers and lakes, consequently infiltrating water treatment and distribution systems (Howard et al., 2016; Khan et al., 2015; Sherpa et al., 2014; Cissé et al., 2016; Kostyla et al., 2015; Chapter 4). Table Box 7.3.1 shows the variety and complexity of pathways between climate hazard and WBD outcomes (Semenza, 2020).
Table Box 7.3.1 | Pathways between climate hazard and waterborne disease (WBD) outcomes. Source: Semenza (2020).
Cascading risk pathways from heavy rain and flooding |
Storm runoff yields water turbidity, which compromises water treatment efficiency Storm runoff and floods mobilise and transport pathogens Overwhelmed or damaged infrastructure compromises water treatment efficiency Floods overwhelm containment system and discharge untreated wastewater Floods damage critical water supply and sanitation infrastructure Floods displace populations towards inadequate sanitation infrastructure |
Cascading risk pathways from drought |
Low water availability augments travel distance to alternate (contaminated) sources Intensified demand for and sharing (e.g., with livestock) of limited water resources decreases water availability and quality Intermittent drinking water supply results in cross-connections with sewer lines and water contamination Uncovered household water containers are a source of vector breeding Poor hygiene due to decreased volume of source water and increased concentration of pathogens Exposure to accumulated human excrements and animal manure |
Cascading risk pathways from increasing temperature |
Extended transmission season for opportunistic pathogens Permissive temperature for the replication of marine bacteria Enhanced pathogen load in animal reservoirs (e.g., chicken) Pathogen survival and proliferation outside of host Wildfires during heatwaves degrade water quality Exposure to contaminated water due to higher water consumption Behaviour change due to extended season (e.g., food spoilage during barbeque) |
Cascading risk pathways from sea level rise |
Population displacement due to powerful storm surges Disruption of drinking water supply and sanitation infrastructure due to inundation Decline in soil and water quality due to saline intrusion into coastal aquifers Seawater infiltration into drinking water distribution and sewage lines |
Notes:
Examples are purposely not exhaustive and should be considered illustrative.
Cross-Chapter Box COVID | COVID-19
Authors: Maarten van Aalst (Netherlands, Chapter 16), Guéladio Cissé (Mauritania/Switzerland/France, Chapter 7), Ayansina Ayanlade (Nigeria, Chapter 9), Lea Berrang-Ford (United Kingdom/Canada, Chapter 16), Rachel Bezner Kerr (Canada/USA, Chapter 5), Robbert Biesbroek (Netherlands, Chapter 13), Kathryn Bowen (Australia, Chapter 7), Martina Angela Caretta (Sweden, Chapter 4), So-Min Cheong (Republic of Korea, Chapter 17), Winston Chow (Singapore, Chapter 6), Mark John Costello (New Zealand/Norway/Ireland, Chapter 11, CCP1), Kristie Ebi (USA, Chapter 7), Elisabeth Gilmore (USA/Canada, Chapter 14), Bruce Glavovic (South Africa/New Zealand, Chapter 18, CCP2), Walter Leal (Germany, Chapter 8), Stefanie Langsdorf (Germany, TSU), Elena Lopez-Gunn (Spain/United Kingdom, Chapter 4), Ruth Morgan (Australia, Chapter 4), Aditi Mukherji (India, Chapter 4), Camille Parmesan (France/ United Kingdom /USA, 2), Mark Pelling (United Kingdom, Chapter 6), Elvira Poloczanska (United Kingdom, TSU), Marie-Fanny Racault (United Kingdom/France, Chapter 3), Diana Reckien (Germany/Netherlands, Chapter 17), Jan C. Semenza (Sweden, Chapter 7), Pramod Kumar Singh (India, Chapter 18), Stavana E. Strutz (USA), Maria Cristina Tirado von der Pahlen (Spain/USA, Chapter 7), Corinne Schuster-Wallace (Canada), Alistair Woodward (New Zealand, Chapter 11), Zinta Zommers (Latvia, Chapter 17)
Introduction
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which causes COVID-19, emerged in late 2019, halfway through the preparation of the IPCC WGII Sixth Assessment Report. This Cross-Chapter Box assesses how the massive shock of the pandemic and response measures interact with climate-related impacts and risks as well as its significant implications for risk management and climate resilient development.
COVID-19 and environmental connections
Infectious diseases may emerge and spread through multiple climate-related avenues, including direct effects of climatic conditions on disease reproduction and transmission and various indirect effects, often interlinked with ecosystem degradation (high confidence). Climate change is affecting the risk of emerging infectious diseases by contributing to factors that drive the movements of species, including vectors and reservoirs of diseases, into novel human populations and vice versa (high confidence) (Sections 2.4.2.7, 5.2.2.3; Cross-Chapter Box Illness in Chapter 2; IPCC, 2019b; IPBES 2020). The spillover of some emerging infectious diseases from wildlife into humans is associated with live animal–human markets, intensified livestock production and climate-related movements of humans and wild animals into new areas that alter human–animal interactions (Section 2.4.2.7; Chapter 3; Sections 5.2.2.3, 7.2; Cross-Chapter Box ILLNESS in Chapter 2; Cross-Chapter Box MOVING PLATE in Chapter 5).
Human-to-human transmission is the prominent driver in the spread of the COVID-19 pandemic, rather than climatic drivers (high confidence). There is emerging literature on the environmental determinants of COVID-19 transmission, incidence and mortality rates, with initial evidence suggesting that temperature, humidity and air pollution contribute to these patterns (Brunekreef et al., 2021; Xiong et al., 2020; Zhang et al., 2020b; AR6 WGI CCB 6.1: Implications of COVID-19 restrictions for emissions, air quality and climate). Climate change is altering environmental factors like temperature and seasonality that affect COVID-19 transmission (Choi et al., 2021).
The impact of COVID-19 containment measures resulted in a temporary reduction in greenhouse gas (GHG) emissions and reduced air pollution (high confidence) (IPCC WGI TS; Arias et al., 2021; AR6 WGI CCB 6.1: Implications of COVID-19 restrictions for emissions, air quality and climate). However, global and regional climate responses to the radiative effect were undetectable above internal climate variability due to the temporary nature of emission reductions. They therefore do not result in detectable changes in impacts or risks due to changes in climate hazards (Arias et al 2021; AR6 WGI CCB 6.1: Implications of COVID-19 restrictions for emissions, air quality and climate; Naik et al., 2021).
Cascading and compounding risks and impacts
The COVID-19 pandemic posed a severe shock to many socioeconomic systems, resulting in substantial changes in vulnerability and exposure of people to climate risks (high confidence). The disease and response measures significantly affected human health, economic activity, food production and availability, health services, poverty, social and gender inequality, education, supply chains, infrastructure maintenance and the environment. These COVID-19 impacts interact with many risks associated with climate change (IMF, 2020), often through a cascade of impacts across numerous sectors (van den Hurk et al., 2020). Beyond COVID-19-related mortality and long-term COVID, mortality from other diseases (some of which may also have a climate-related component), as well as maternal and neonatal mortality, increased because of disruption in health services (Barach et al., 2020; Maringe et al., 2020; Zadnik et al., 2020; Goyal et al., 2021). In addition, a rapid rise in poverty has disproportionately affected poorer countries and people (Ferreira et al., 2021), and thus increased their vulnerability. After many years of steady declines, extreme poverty increased by about 100 million people in 2020 (World Bank, 2021). The effects of the pandemic increased food insecurity and malnourishment, which increased by 1.5 percentage points to around 9.9% in 2020 after being virtually unchanged for the previous five years (FAO et al., 2021).
During the pandemic, extreme weather and climate events such as droughts, storms, floods, wildfires and heatwaves continued, resulting in disastrous compounding impacts (high confidence). Between March and September 2020, 92 extreme weather events coincided with the COVID-19 pandemic, affecting an estimated 51.6 million people; additionally, 431.7 million people were exposed to extreme heat, and 2.3 million people were affected by wildfires (Walton and van Aalst, 2020). The COVID-19 pandemic, in combination with extreme events, affected disaster preparedness, disaster response and safe evacuations, while physical distancing regulations reduced the capacity of temporary shelters (UN DRR Asia-Pacific, 2020; Tozier de la Poterie et al., 2020; Shumake-Guillemot, J, et al, 2020; Bose-O’Reilly et al., 2021). Complex humanitarian emergencies were aggravated, with vulnerable populations facing the combined risks of conflict, displacement, COVID-19 and climate impacts (FSIN, 2020). Compounding events are not only found in low-income countries but also in medium- and high-income countries, for instance in the case of COVID-19 and heatwaves (Shumake-Guillemot et al., 2020; Bose-O’Reilly et al., 2021).
Cross-Chapter Box COVID
Responses and implications for adaptation and climate resilient development
The pandemic emphasises the inter-connected and compound nature of risks, vulnerabilities and responses to emergencies that are simultaneously local and global (high confidence). COVID-19 is often considered a more ‘explosive’ risk than the more gradual anthropogenic climate change. However, many climate-related risks do already appear as severe shocks at smaller scales, and infrequent or unprecedented extreme weather-related events often warrant similar rapid responses (Dodds et al., 2020; Gebreslassie, 2020; Hynes et al., 2020; Phillips et al., 2020; Schipper, 2020; Semenza et al., 2021; illustrated in Figure COVID.1). Individuals, households, sub-national and national entities, and international organisations had generally delayed responses or denied the pandemic’s severity before responding at the scale and urgency required, a pattern that resembles the international action required on climate change (Polyakova et al., 2020; Shrestha et al., 2020).
Improved contingency and recovery planning, including disease mitigation measures, were crucial in responding to the pandemic in similar ways to those seen in the aftermath of climate-related disasters (Guo et al., 2020; Ebrahim et al., 2020; Baidya et al., 2020; Shultz et al., 2020; Mukherjee et al., 2020). The pandemic highlighted the lack of global and country-specific capacity to respond to an unexpected and unplanned event and the need to implement more flexible detection and response systems (Ebi et al., 2021b).
It also exposed underlying vulnerabilities, such as the lack of water access and healthcare in select low- and middle-income countries and among indigenous and marginalised groups in high-income countries (Section 4.4.3; Box 4.3; 5.12.1). Increased risks of COVID-19 transmission emerged in crowded areas such as urban settings, refugee camps, detention centres and some workplaces, including in rural settings (Brauer et al., 2020; Ramos et al., 2020; Staddon et al., 2020; Haddout et al., 2020). Public health responses to the COVID-19 pandemic, such as mandates for social distancing and advice for frequent handwashing, underlined the need for access to water and sanitation facilities and wastewater management. However, they also sometimes interfered with access, for example, in evacuation and shelter infrastructure during climate-related disasters (Armitage and Nellums, 2020; Adelodun et al., 2020; Poch et al., 2020; Hallema et al., 2020; Patel et al., 2020; Espejo et al., 2020).
The experience of COVID-19 demonstrates that many warnings about the risks of the emergence of zoonotic transmission (‘delay is costly’, ‘adapt early’ and ‘prevention pays’) did not result in sufficient political attention, funding and pandemic prevention. In some countries, there has been an increased awareness of the risks and the real or perceived trade-offs associated with risk management (e.g., economy compared with health and impacts compared with adaptation). Building trust and participatory processes and establishing stronger relationships with communities and other civic institutions may enable a recalibration of how the government responds to crises and society–government relationships more generally (Amat et al., 2020; Deslatte, 2020).
The management of the COVID-19 pandemic has highlighted the value of scientific (including medical and epidemiological) expertise and the importance of fast, accurate and comprehensive data to inform policy decisions and to anticipate and manage risk (high confidence). It emphasises the importance of effective communication of scientific knowledge (Semenza et al., 2021), decision-making under uncertainty and decision frameworks that navigate different values and priorities. Successful policy responses were based on the emerging data, medical advice and collaboration with a wider set of societal stakeholders beyond public health experts. For instance, experience in Aotearoa, New Zealand, highlights the importance of pandemic responses attuned to the needs of different sociocultural groups and Indigenous Peoples in particular. Their strengths-based COVID-19 response goes beyond identifying vulnerabilities to unlocking the resources, capabilities and potential that might otherwise be latent in communities (McMeeking and Savage, 2020). As far as the value of information for risk management is concerned, compared to the initial uncertainties regarding COVID-19, data about near- and longer-term climate-related hazards is generally very good; however, high-quality and dense meteorological data are often still lacking in lower income countries (Otto et al., 2020). Health data are particularly difficult to obtain in real time, as is the case for biodiversity data, which has a time lag of years before being made available and for which there is no coordinated monitoring, hampering effective risk management (Navarro et al., 2017). Therefore, both epidemiological and meteorological forecasts would benefit from more focus on (a) decision support, (b) conveying uncertainty and (c) capturing vulnerability (Coughlan de Perez et al., 2021).
There is a considerable evidence base of specific actions that have co-benefits for reducing pandemic and climate change risks while enhancing social justice and biodiversity conservation (high confidence). The pandemic highlighted aspects of risk management that have long been recognised but are often not reflected in national and international climate policy: the value of addressing structural vulnerability rather than taking specific measures to control single hazards and drivers of risk and the importance of decision-making capacities and transparency, the rule of law, accountability and addressing inequities (or social exclusion) (reviewed by Pelling et al. (2021); see also Figure COVID.1).
Cross-Chapter Box COVID
Comprehensive and integrated risk management strategies can enable countries to address both the current pandemic and increase resilience against climate change and other risks (Reckien, 2021; Semenza et al., 2021; Ebi et al., 2021b). In particular, given their immense scale, COVID-19 recovery investments may offer an opportunity to contribute to climate resilient development pathways (CRDPs) through a green, resilient, healthy and inclusive recovery (high confidence) (Sovacool et al., 2020; Rosenbloom and Markard, 2020; Lambert et al., 2020; Boyle et al., 2020; Bouman et al., 2020; UN DRR Asia-Pacific, 2020; Brosemer et al., 2020; Dodds et al., 2020; Hynes et al., 2020; Markard and Rosenbloom, 2020; Phillips et al., 2020; Schipper, 2020; Willi et al., 2020; Semenza et al., 2021; Pasini and Mazzocchi, 2020; Meige et al., 2020; Pelling et al., 2021). However, windows of opportunity to enable such transitions are only open for a limited period and need to be swiftly acted upon to effect change (high confidence) (Chapter 18; Weible et al., 2020; Reckien, 2021). Initial indications suggest that only USD 1.8 trillion of the greater than USD 17 trillion COVID-19-related stimulus financing by G20 countries and other major economies that was committed up until mid-2021 contributed to climate action and biodiversity objectives, with significant differences between countries and sectors (Vivideconomics, 2021). Moreover, responses to previous crises (e.g., the 2008–2011 global financial crisis) demonstrate that despite high ambitions during the response phase, opportunities for reform do not necessarily materialise (Bol et al., 2020; Boin et al., 2005). In addition, heightened societal and political attention to one crisis often comes at the cost of other policy priorities (high confidence) (Maor, 2018; Tosun et al., 2017), which could affect investments for climate resilient development (Hepburn et al., 2020; WHO, 2020a; Bateman et al., 2020; Meige et al., 2020; Semenza et al., 2021).
In summary, the emerging literature suggests that the COVID-19 pandemic has aggravated climate-related health risks, demonstrated the global and local vulnerability to cascading shocks and illustrated the importance of integrated solutions that tackle ecosystem degradation and structural vulnerabilities in human societies. This highlights the potential and urgency of interventions that reduce pandemic and climate change risks while enhancing compound resilience, social justice and biodiversity conservation (see Figure COVID.1).

Figure COVID.1 | Compound risk and compound resilience to pandemic and climate change. Source: Pelling et al. (2021).
7.2.3 Observed Impacts on Non-communicable Diseases
NCDs are those that are not directly transmitted from one person to another person; they impose the largest disease burden globally. NCDs constitute approximately 80% of the burden of disease in high-income countries; the NCD burden is lower in low- and middle-income countries but are expected to rise (Bollyky et al., 2017). NCDs constitute a large group of diseases driven principally by environmental, lifestyle and other factors; those identified as being climate sensitive include non-infectious respiratory disease, cardiovascular disease (CVD), cancer and endocrine diseases including diabetes. Additionally, there are potential interactions between multiple climate-sensitive NCDs and food security, nutrition and mental health. The literature on climate change and NCDs continues to develop. More recently, scientists have identified key gaps in the calculation of the global burden of disease due to environmental health factors (Shaffer et al., 2019).
7.2.3.1 Cardiovascular Diseases
CVDs are a group of disorders of the heart and blood vessels that include coronary heart disease, cerebrovascular disease, peripheral arterial disease, rheumatic heart disease, congenital heart disease, deep vein thrombosis and pulmonary embolism. CVDs are the leading cause of death globally and over three quarters of the world’s CVD deaths now occur in low- and middle-income countries (Roth et al., 2020).
Climate change affects the risk of CVD through high temperatures and extreme heat (assessed in Section 7.2.4.1) and through other mechanisms (medium confidence), though the degree to which non-temperature risks may increase remains unclear. For example, exposure to air pollutants including PM, ozone (via its precursors), black carbon, oxides of nitrogen, oxides of sulphur, hydrocarbons and metals can invoke pro-inflammatory and prothrombotic states, endothelial dysfunction and hypertensive responses (Giorgini et al., 2017; Stewart et al., 2017). Winter peaks in CVD events, associated with greater concentrations of air pollutants, have been reported in a range of countries and climates (Claeys et al., 2017; Stewart et al., 2017); however, the association between air pollution, weather and CVD events is complex and seems to differ between cold and warm months, particularly for gaseous pollutants such as ozone (Shi et al., 2020).
Climate change is projected to increase the number and severity of wildfires (Liu et al., 2015b; Youssouf et al., 2014) and the evidence for wildfire smoke-related CVD morbidity and mortality is suggestive of increased CVD morbidity and mortality risk (Chen et al., 2021a) including significant increases in certain cardiovascular outcomes (e.g., cardiac arrests) (Dennekamp et al., 2015). CVD risks to highly exposed populations, such as firefighters, are clearer (Navarro et al., 2019) and could increase with additional exposure driven by climate change.
Other climate-related mechanisms that may increase CVD risk include reductions in physical activity related to hot weather (Obradovich et al., 2017), sleep disturbance (Obradovich et al., 2017) and dehydration (Lim et al., 2015; Frumkin and Haines, 2019). There is little literature on how changes in winter weather may affect these risks. Saline intrusion of groundwater related to sea level rise (Taylor et al., 2012) may increase the salt intake of affected populations, a risk factor for hypertension that has been observed to increase blood pressure in exposed populations (Talukder et al., 2017; Al Nahian et al., 2018).
7.2.3.2 Non-communicable Respiratory Diseases
Lung diseases, including asthma, COPD and lung cancer, comprise the largest subsets of non-communicable pulmonary disease (Ferkol and Schraufnagel, 2014). Overall, the global burden of non-communicable lung disease including all chronic lung disease and lung cancer is substantial, being responsible for 10.6% of deaths and 5.9% of DALYs globally in 2019 (Vos et al., 2020).
Several non-communicable respiratory diseases are climate sensitive based on their exposure pathways (very high confidence). Multiple exposure pathways contribute to non-communicable respiratory disease (Deng et al., 2020), some of which are climate-related (Rice et al., 2014), including mobilisation and transport of dust (Schweitzer et al., 2018); changes in concentrations of air pollutants such as small particulates (PM2.5) and ozone formed by photochemical reactions sensitive to temperature (Hansel et al., 2016); increased wildland fires and related smoke exposure (Johnston et al., 2002; Reid et al., 2016); increased exposure to ambient heat driving reduced lung function and exacerbations of chronic lung disease (Collaco et al., 2018; Jehn et al., 2013; McCormack et al., 2016; Witt et al., 2015) and modification of aeroallergen production and duration of exposure (Ziska et al., 2019).
Burdens of allergic disease, particularly allergic rhinitis and allergic asthma may be changing in response to climate change (medium confidence) (D’Amato et al., 2020; Eguiluz-Gracia et al., 2020; Deng et al., 2020; Demain, 2018). This is supported by evidence showing an increase in the length of the North American pollen season attributable to climate change (Ziska et al., 2019), an association between timing of spring onset and higher asthma hospitalisations presumed to be due to higher pollen exposure (Sapkota et al., 2020) and other evidence linking aeroallergen exposure with a worsening burden of allergic disease (Demain, 2018; Poole et al., 2019).
7.2.3.3 Cancer
Climate change is likely to increase the risk of several malignancies (high confidence), though the degree to which risks may increase remains unclear. Cancers, also known as malignant neoplasms, include a heterogeneous collection of diseases with various causal pathways, many with environmental influences. Malignant neoplasms impose a substantial burden of disease globally and are responsible for slightly more than 10 million deaths and 251 million DALYs globally in 2019 (Vos et al., 2020). Climatic hazards affect exposure pathways for several different chemical hazards associated with carcinogenesis (Portier et al., 2010). Most relevant literature has focused on elaborating potential pathways and producing qualitative or quantitative estimates of effect, though there is limited literature on current and projected impacts.
The vast majority of elaborated pathways point to increased risk; for example, there is concern that climate change may alter the fate and transport of carcinogenic polyaromatic hydrocarbons (Domínguez-Morueco et al., 2019) and increase mobilisation of carcinogens such as bromide (Regli et al., 2015), persistent organic pollutants (POPs) including polychlorinated-biphenyls that have accumulated in areas contaminated by industrial runoff (Miner et al., 2018) and radioactive material (Evangeliou et al., 2014). Exposure to these known carcinogens can occur through multiple environmental media and can be increased by climate change, for example through increased flooding related to extreme precipitation events and mobilisation of sediment where carcinogens have accumulated (León et al., 2017; Santiago and Rivas, 2012). In addition, there is concern that changes in ultraviolet light exposure related to shifts in precipitation may increase the incidence of malignant melanoma, particularly for outdoor workers (Modenese et al., 2018). Other harmful pathways include migration of and increased exposure to liver flukes, which cause hepatobiliary cancer (Prueksapanich et al., 2018) and the introduction of infectious diseases such as schistosomiasis that increase cancer risk due to climate-related migration (Ahmed et al., 2014). Increased exposure to carcinogenic toxins via multiple pathways is also a concern. Aflatoxin exposure, for example, is expected to increase in Europe (Moretti et al., 2019), India (Shekhar et al., 2018), Africa (Gnonlonfin et al., 2013; Bandyopadhyay et al., 2016) and North America (Wu et al., 2011). Other carcinogenic toxins originate from cyanobacteria blooms (Lee et al., 2017a), which are projected to increase in frequency and distribution with climate change (Wells et al., 2015; Paerl et al., 2016; Chapra et al., 2017).
7.2.3.4 Diabetes
Individuals suffering from diabetes are at higher risk of heat-related illness and death (medium confidence). Extreme weather events and rising temperatures have been found to increase morbidity and mortality in patients living with diabetes, especially in those with cardiovascular complications (Méndez-Lázaro et al., 2018; Zilbermint, 2020; Hajat et al., 2017). Evidence suggests that the local heat loss response of skin blood flow is affected by diabetes-related impairments, resulting in lower elevations in skin blood flow in response to a heat or pharmacological stimulus. Thermoregulatory sweating may also be diminished by type-2 diabetes, impairing the body’s ability to transfer heat from its core to the environment (Xu et al., 2019b). Higher rates of doctor consultations by patients with type-2 diabetes and diabetics with cardiovascular comorbidities have been observed during hot days, but without evidence of heightened risk of renal failure or neuropathy comorbidities (Xu et al., 2019b).
People with chronic illnesses are at particular risk during and after extreme weather events due to treatment interruptions and lack of access to medication (medium confidence). The impacts of extreme weather events on the health of chronically ill people are due to a range of factors including disruption of transport, weakened health systems including drug supply chains, loss of power and evacuations of populations (Ryan et al., 2015a). Evacuations also pose specific health risks to older adults (especially those who are frail, medically incapacitated or residing in nursing or assisted living facilities) and may be complicated by the need for concurrent transfer of medical records, medications and medical equipment (Becquart et al., 2018; Quast and Feng, 2019; US Global Change Research Program, 2016). Emergency room visits after Hurricane Sandy rose among individuals with type-2 diabetes (Velez-Valle et al., 2016).
7.2.4 Observed Impacts on Other Climate-Sensitive Health Outcomes
7.2.4.1 Heat- and Cold-Related Mortality and Morbidity
Extreme heat events and extreme temperature have well-documented, observed impacts on health, mortality (very high confidence) and morbidity (high confidence). AR5 described the thermoregulatory mechanisms and responses, including acclimatisation, linking heat, cold and health, and these have been further confirmed by recent studies and reviews (e.g., Giorgini et al., 2017; Ikaheimo, 2018; McGregor et al., 2015; Stewart et al., 2017; Schuster et al., 2017; Zhang et al., 2018b). The health impacts of heat manifest clearly in periods of extreme heat often codified as heatwaves. For example, heatwaves across Europe (2003), Russia (2010), India (2015) and Japan (2018) resulted in significant death tolls and hospitalisations (McGregor et al., 2017; Hayashida et al., 2019). Heat continues to pose a significant health risk due to increases in exposure, changes in the size and spatial distribution of the human population, mounting vulnerability and an increase in extreme heat events (high confidence) (Harrington et al., 2017; Liu et al., 2017; Mishra et al., 2017; Rohat et al., 2019a; Rohat et al., 2019b; Rohat et al., 2019c; Watts et al., 2019). Some regions are already experiencing heat stress conditions approaching the upper limits of labour productivity and human survivability (high confidence). These include the Persian Gulf and adjacent land areas, parts of the Indus River Valley, eastern coastal India, Pakistan, northwestern India, the shores of the Red Sea, the Gulf of California, the southern Gulf of Mexico and coastal Venezuela and Guyana (Krakauer et al., 2020; Li et al., 2020; Raymond et al., 2020; Saeed et al., 2021; Xu et al., 2020).
Under a variety of methods, estimates of the world’s population exposed to extreme heat indicate very large and growing numbers and an increase since pre-industrial times. For example, Li et al. (2020) estimate that globally, 1.28 billion people each year experience heatwave conditions similar to that of the lethal Chicago 1995 event, compared with 0.99 billion people that would be similarly exposed under a pre-industrial climate. Further, for the 150 most populated cities of the world, a 500% increase in the exposure to extreme heat events occurred over the 1980–2017 period (Li et al., 2021), while for the 1986–2005 period, the total exposure to dangerous heat in Africa’s 173 largest cities was 4.2 billion person-days yr –1 (Rohat et al., 2019a). Globally the present exposure to heatwave events is estimated to be 14.8 billion person-days yr –1, with the greatest cumulative exposures measured in person-days occurring across southern Asia (7.19 billion), sub-Saharan Africa (1.43 billion), and north Africa and the Middle East (1.33 billion) (Jones et al., 2018).
The country level percentage of mortality attributable to non-optimum temperature (heat and cold) has been found to range from 3.4 to 11% (Gasparrini et al., 2015; Zhang et al., 2019b). Heat as a health risk factor has largely been overlooked in low- and middle-income countries (Campbell et al., 2018; Green et al., 2019; Dimitrova et al., 2021). For 2019, the GBD report estimates the burden of DALYs attributable to low temperature was 2.2 times greater than the burden attributable to high temperature. However, this global figure obscures important regional variations. Countries with a high sociodemographic index—mainly mid-latitude high-income temperate to cool climate countries— were found to have a cold-related burden 15.4 times greater than the heat-related burden, while for warm lower-income regions, such as south Asia and sub-Saharan Africa, the heat-related burden was estimated to be 1.7 times and 3.6 times greater, respectively (Murray et al., 2020). For countries where data availability permits, there is evidence that extreme heat (and extreme cold) leads to higher rates of premature deaths (Armstrong et al., 2017; Cheng et al., 2018; Costa et al., 2017).
Rapid changes and variability in temperatures are observed to increase heat-related health and mortality risks, the outcomes varying across temperate and tropical regions (Guo et al., 2016; Cheng et al., 2019; Kim et al., 2019a; Tian et al., 2019; Zhang et al., 2018b; Zhao et al., 2019).
Several lines of evidence point to a possible decrease in population sensitivity to heat, albeit mainly for high-income countries (high confidence), arising from the implementation of heat warning systems, increased awareness and improved quality of life. (Sheridan and Allen, 2018). Evidence suggests a general decrease in the impact of heat on daily mortality (Diaz et al., 2018; Kinney, 2018; Miron et al., 2015), a decline in the relative risk attributable to heat (Åström et al., 2018; Barreca et al., 2016; Petkova et al., 2014) and an increase in the minimum mortality temperature (MMT) (Åström et al., 2018; Folkerts et al., 2020; Follos et al., 2021; Chung et al., 2018; Todd and Valleron, 2015; Yin et al., 2019). It is difficult to draw conclusions regarding trends in heat sensitivity for low- to middle-income countries and specific vulnerable groups as these are under-represented in the literature (Sheridan and Allen, 2018). Trends in heat sensitivity are generally believed to be scale and situation dependent, but there is considerable variability in changes in heat sensitivity as measured by trends in heat-related mortality or MMT (Follos et al., 2021; Kim et al., 2019a; Lee et al., 2021), with notable variability across different population groups (Lu et al., 2021).
Temperature interacts with heat-sensitive physiological mechanisms via multiple pathways to affect health. In the worst cases, these lead to organ failure and death (Mora et al., 2017a; Mora et al., 2017b). Excess deaths during extreme heat events occur predominantly in older individuals and are overwhelmingly cardiovascular in origin (very high confidence). A higher occurrence of CVD mortality in association with prolonged period of low temperatures has been well documented globally (Giorgini et al., 2017; Stewart et al., 2017); however, there is growing evidence that cardiovascular deaths are more related to heat events than cold spells (Chen et al., 2019; Liu et al., 2015a; Bunker et al., 2016). While there is strong association between ambient temperature and cardiovascular events globally, there are complex interactions and modulators of individual response (Wang et al., 2017 b). Further, some CVD morbidity sub-groups such as myocardial infarction (MI) and stroke hospitalisation display temperature sensitivity while others do not (Bao et al., 2019; Sun et al., 2018; Wang et al., 2016). Although older adults have inherent sensitivities to temperature-related health impacts (Bunker et al., 2016; Phung et al., 2016), children can also be affected by extreme heat (Xu et al., 2014). Cardiovascular capacity or health is also a critical determinant of individual health outcomes (Schuster et al., 2017). Medications to treat CVDs, such as diuretics and beta-blockers, may impair resilience to heat stress (Stewart et al., 2017). Other mediating factors in the causal pathway range from alcohol consumption (Cusack et al., 2011; Epstein and Yanovich, 2019) and obesity (Speakman, 2018) to pre-existing conditions, such as diabetes and hyperlipidaemia, and urban characteristics (Chen et al., 2019; Sera et al., 2019).
Under extreme heat conditions, increases in hospitalisations have been observed for fluid disorders, renal failure, urinary tract infections, septicaemia, general heat stroke as well as unintentional injuries (Borg et al., 2017; Phung et al., 2017; Goggins and Chan, 2017; Hayashida et al., 2019; Hopp et al., 2018; Ito et al., 2018; Kampe et al., 2016; McTavish et al., 2018; Ponjoan et al., 2017; van Loenhout et al., 2018). Hospitalisations and mortality due to respiratory disorders also occur during heat events with the interactive role of air quality being important for some locations but not others (Krug et al., 2019; Pascal et al., 2021; Patel et al., 2019). Increased levels of heat-related hospitalisation also manifest in elevated levels of emergency service calls (Cheng et al., 2016; Guo, 2017; Papadakis et al., 2018; Williams et al., 2020).
Heat- and cold-related health outcomes vary by location (Dialesandro et al., 2021; Hu et al., 2019; Phung et al., 2016), suggesting outcomes are highly moderated by socioeconomic, occupational and other non-climatic determinants of individual health and socioeconomic vulnerability (Åström et al., 2020; McGregor et al., 2017; McGregor et al., 2017; Schuster et al., 2017; Benmarhnia et al., 2015; Watts et al., 2019) (high confidence). For example, access to air conditioning is an important determinant of heat-related health outcomes for some locations (Guirguis et al., 2018; Ostro et al., 2010). Although there is a paucity of global level studies of the effectiveness of air conditioning for reducing heat-related mortality, a recent assessment indicates increases in air conditioning explains only part of the observed reduction in heat-related excess deaths, amounting to 16.7% in Canada, 20.0% in Japan, 14.3% in Spain and 16.7% in the US (Sera et al., 2020).
Significant effects of heat exposure are evident in sport and work settings with exertional heat illness leading to death and injury (Adams and Jardine, 2020). Although most studies of heat-related sports injuries refer to high-income countries, these point to an increasing number of heat injuries with widening participation in sport and an increasing frequency of extreme heat events. The highest rates of exertional heat illness are reported for endurance type events (running, cycling and adventure races), American football and athletics (Gamage et al., 2020; Grundstein et al., 2017; Kerr et al., 2020; McMahon et al., 2021; Yeargin et al., 2019). The health, safety and productivity consequences of working in extreme heat are widespread (Ma et al., 2019; Morabito et al., 2021; Kjellstrom et al., 2019; Orlov et al., 2020; Smith et al., 2021; Vanos et al., 2019; Varghese et al., 2020; Williams et al., 2020). Occupational heat strain in outdoor workers manifests as dehydration, mild reduction in kidney function, fatigue, dizziness, confusion, reduced brain function, loss of concentration and discomfort (Al-Bouwarthan et al., 2020; Boonruksa et al., 2020; Habibi et al., 2021; Levi et al., 2018; Venugopal et al., 2021; Xiang et al., 2014). In the case of armed forces, a global review of the available literature points to a slightly higher incidence of heat stroke in men compared to women but a higher proportion of heat intolerance and greater risk of exertional heat illness amongst women (Alele et al., 2020). There is also some evidence that for healthcare workers, the risk of occupational heat stress grew during the COVID-19 pandemic due to the need to wear personal protective equipment (Foster et al., 2020; Lee et al., 2020; Messeri et al., 2021). Based on a systematic review of the literature, one study estimates global costs from heat-related lost work time were USD 280 billion in 1995 and USD 311 billion in 2010, with low- and middle-income countries and countries with warmer climates experiencing greater losses as a proportion of gross domestic project (GDP) (Borg et al., 2021). Other global level assessments note an increase in the potential hours of work lost due to heat over the 2000–2018 period; in 2018, 133.6 billion potential work hours were lost, amounting to 45 billion hours more than in 2000 (Watts et al., 2019). For China, heat-related productivity losses have been estimated at 9.9 billion hours in 2019, equivalent to 0.5% of the total national work hours for that year, with Guangdong province, one of the warmest regions in China, accounting for almost a quarter of the losses (Cai et al., 2021).
Wide ranging knowledge regarding the specific detection of heat- and cold-related mortality/morbidity and its attribution to observed climate change is lacking . Although there has been an observed increase in winter-season temperatures for a number of regions, to date there is variable evidence for a consequential reduction in winter mortality and susceptibility to cold over time due to milder winters; some countries demonstrate decreasing trends, while other countries show stable or even increasing trends in cold-attributable mortality fractions over time (e.g., Arbuthnott et al. (2020); Åström et al. (2013); Diaz et al. (2019); Hajat (2017); Hanigan et al. (2021); Lee et al. (2018b)). While there is a burgeoning literature on the attribution of extreme heat events to climate change (e.g., Vautard et al. (2020)), the number of studies that assess the extent to which observed changes in heat-related mortality may be attributable to climate change is small (Ebi et al., 2020). During the 2003 European heatwave, anthropogenic climate change increased the risk of heat-related mortality by approximately 70% and 20% for London and Paris, respectively (Mitchell et al., 2016). For the severe heat event across Egypt in 2015, the impact on human discomfort was 69% (±17%) more likely due to anthropogenic climate change (Mitchell, 2016), and for Stockholm, Sweden, it has been estimated that mortality due to temperature extremes for 1980 to 2009 was double what would have occurred without climate change (Åström et al., 2013). To date there has only been one multi-country attempt to quantify the heat-related human health impacts that have already occurred due to climate change. Based on an analysis of 732 locations spanning 43 countries for the 1991–2018 period, the study found that on average 37.0% (inter-quartile range 20.5–76.3%) of warm-season heat-related deaths can be attributed to anthropogenic climate change, equivalent to an average mortality rate of 2.2/100,000 (median: 1.67/100,000; interquartile range: 1.08–2.34/100,000). Regions with a high attributed percentage (> 50%) include southern and western Asia (Iran and Kuwait), Southeast Asia (Philippines and Thailand) and several countries in Central and South America. Those with lower values (< 35%) include Western Europe (the Netherlands, Germany and Switzerland), eastern Europe (Moldova, the Czech Republic and Romania), southern Europe (Greece, Italy, Portugal and Spain), North America (USA) and eastern Asia (China, Japan and South Korea) (Vicedo-Cabrera et al., 2021). Due to data restrictions, some of the poorest and most susceptible regions to climate change and increases in heat exposure, such as west and east Africa (Asefi-Najafabady et al., 2018; Sylla et al., 2018) and south Asia, could not be included in the analysis (Mitchell, 2021).
7.2.4.2 Injuries Arising from Extreme Weather Events Other than Heat and Cold
Injuries comprise a substantial portion of the global burden of disease. In 2019, injuries comprised 9.82% of total global DALYs and 7.61% of deaths (Vos et al., 2020). The causal pathways for many injuries, particularly those from heat and extreme weather events, flooding and fires, exhibit clear climate sensitivity (Roberts and Arnold, 2007; Roberts and Hillman, 2005), as do some injuries occurring in occupational settings (Marinaccio et al., 2019; Sheng et al., 2018), but a comprehensive assessment of climate sensitivity in injury causal pathways has not been done. Certain groups, including Indigenous Peoples, children and the elderly (Ahmed et al., 2020) are at greater risk for a wide range of injuries. Extreme events impose substantial disease burden directly as a result of traumatic injuries, drowning and burns and large mental health burdens associated with displacement (Fullilove, 1996), depression and post-traumatic stress disorder (PTSD), but the overall injury burden associated with extreme weather is not known. It is known that the Asia-Pacific region has experienced the highest relative burden of injuries from extreme weather in recent decades (Hashim and Hashim, 2016).
Extreme weather imposes a substantial morbidity and mortality burden that is quite variable by location and hazard. The proportion of this burden related specifically to injuries is not established. From 1998 to 2017 there were 526,000 deaths from 11,500 extreme weather events, and the average annual attributable all-cause mortality incidence in the ten most affected countries was 3.5 per 100,000 population (Eckstein et al., 2017). Rates can be much higher; mortality incidence in Puerto Rico and Dominica from extreme weather were 90.2 and 43.7 per 100,000 population in 2017, respectively (Eckstein et al., 2017). Not all of these deaths are from injuries, and the proportion of mortality and morbidity associated with injuries varies by location and hazard. One review found that one-year post-event prevalence rates for injuries associated with extreme events (floods, droughts, heatwaves and storms) in developing countries ranged from 1.4% to 37.9% (Rataj et al., 2016). Other literature has documented an increase in the risk of motor vehicle accidents in association with extreme precipitation (Liu et al., 2017; Stevens et al., 2019), temperature (Leard and Roth, 2019) and sandstorms (Islam et al., 2019) and an increased risk of traumatic occupational injuries associated with temperature extremes, particularly extreme heat, likely from fatigue and decreased psychomotor performance (Varghese et al., 2019).
There is clear evidence of climate sensitivity for multiple injuries from floods, fires and storms, but there is a need for additional evidence regarding the current injury burden attributable to climate change. It is as likely as not that climate change has increased the current burden of disease from injuries related to extreme weather, particularly in low-income settings (low confidence). Approximately 120 million people are exposed to coastal flooding annually (Nicholls et al., 2007), causing an estimated 12,000 deaths (Shultz et al., 2005), and there is significant concern for worsening flooding associated with climate change (Shultz et al., 2018a; Shultz et al., 2018b; Woodward and Samet, 2018) but very limited quantification of attributable burden. A range of adverse health outcomes has been identified in a study of fires in sub-zero temperatures that are thought to be increasing in frequency due to climate change (Metallinou and Log, 2017).
7.2.4.3 Observed Impacts on Maternal, Foetal and Neonatal Health
Maternal and neonatal disorders accounted for 3.7% of total global deaths and 7.8% of global DALYs in 2019 (Vos et al., 2020). Children and pregnant women have potentially higher rates of vulnerability and/or exposure to climatic hazards, extreme weather events and undernutrition (Garcia and Sheehan, 2016; Sorensen et al., 2018; Chersich et al., 2018). Available evidence suggests that heat is associated with higher rates of pre-term birth (Wang et al., 2020), low birthweight, stillbirth, neonatal stress (Cil and Cameron, 2017; Kuehn and McCormick, 2017) and adverse child health (Kuehn and McCormick, 2017). Extreme weather events are associated with reduced access to prenatal care, unattended deliveries (Abdullah et al., 2019) and decreased paediatric healthcare access (Haque et al., 2019).
7.2.4.4 Observed Impacts on Malnutrition
Climate variability and change contribute to food insecurity that can lead to malnutrition, including undernutrition, overweight and obesity, and to disease susceptibility, particularly in low- and middle-income countries (high confidence). Since AR5, analyses of the links between climate change and food expanded beyond undernutrition to include the impacts of climate change on a wider set of diet- and weight-related risk factors and their impacts on NCDs, along with the role of dietary choices for GHG emissions (IPCC, 2019b) including dietary inadequacy (deficiencies, excesses or imbalances in energy, protein and micronutrients), infections and sociocultural factors (Global Nutrition Report 2020). Undernutrition exists when a combination of insufficient food intake, health, and care conditions results in one or more of the following: underweight for age, short for age (stunted), thin for height (wasted), or functionally deficient in vitamins and/or minerals (micronutrient malnutrition or ‘hidden hunger’). Food insecurity and poor access to nutrient-dense food contribute not only to undernutrition but also to obesity and susceptibility to NCDs in low- and middle-income countries (FAO et al., 2018; Swinburn et al., 2019).
Globally, more than 690 million people are undernourished, 144 million children are stunted (chronic undernutrition), 47 million children are wasted (acute undernutrition), and more than 2 billion people have micronutrient deficiencies (FAO, 2020). More than 135 million people across 55 countries experienced acute hunger requiring urgent food, nutrition and livelihood assistance in 2019 (FSIN/GNAFC, 2020). The COVID-19 pandemic is projected to increase the number of acutely food insecure people to 270 million people (FSIN, 2020) and worsen malnutrition levels (FAO et al., 2020; Rippin et al., 2020). The relationships between climate change and obesity vary based on geography, population sub-groups and/or stages of economic growth and population growth (An et al., 2017). Increasing temperatures could contribute to obesity through reduced physical activity, increased prices of produce or shifts in eating patterns of populations towards more processed foods (An et al., 2018). In the largest global study to date exploring the connections between child diet diversity and recent climate, data from 19 countries in six regions (Asia, Central America, South America, north Africa, southeast Africa and west Africa) indicated significant reductions in diet diversity associated with higher temperatures and significant increases in diet diversity associated with higher precipitation (Niles et al., 2021).
Climate change can affect the four aspects of food security: food production and availability, stability of food supplies, access to food and food utilisation (IPCC, 2019b). Access to sufficient food does not guarantee nutrition security. Extreme weather and climate events can result in inadequate or insufficient food consumption, increasing susceptibility to infectious diseases (Rodriguez-Llanes et al., 2016; Gari et al., 2017; Kumar et al., 2016; Lazzaroni and Wagner, 2016) but also to being overweight or obese and increasing susceptibility to non-communicable diseases in low- and middle-income countries (FAO, 2018; Swinburn et al., 2019).
Nearly half of all deaths in children under five years of age are attributable to undernutrition, putting children at greater risk of dying from common infections. Undernutrition in the first 1,000 days of a child’s life can lead to stunted growth, which can result in impaired cognitive ability and reduced future school and work performance and the associated costs of stunting in terms of lost economic growth can be of the order of 10% of GDP yr –1 in Africa (UNICEF/WHO/WBG, 2019).
At the same time, diseases associated with high-calorie, unhealthy diets are increasing globally, with 38.3 million overweight children under five years of age (Global Nutrition Report, 2018), 2.1 billion overweight or obese adults and the global prevalence of diabetes almost doubling in the past 30 years (Swinburn et al., 2019). Unbalanced diets, such as diets low in fruits and vegetables and high in red and processed meat, are the number one risk factor for mortality globally and in most regions (Gakidou et al., 2018; Afshin et al., 2019).
Socioeconomic factors that mediate the influence of climate change on nutrition include cultural and societal norms; governance, institutions, policies and fragility; human capital and potential; and social position and access to healthcare, education and food aid (Rozenberg, 2017; Alkerwi et al. 2015; Tirado, 2017; FAO et al., 2018; Global Nutrition Report 2020). Extreme events may affect access to adequate diets, leading to malnutrition and increasing the risk of disease (Beveridge et al., 2019; Rodriguez-Llanes et al., 2016; Gari et al., 2017; Kumar et al., 2016; Lazzaroni and Wagner, 2016; Thiede and Gray, 2020).
7.2.4.5 Observed Impacts on Exposure to Chemical Contaminants
Climate change in northern regions, including Arctic ecosystems, is causing permafrost to thaw, creating the potential for mercury (Hg) to enter the food chain (medium agreement, low evidence)as methyl mercury (MeHg), which is highly neurotoxic and nephrotoxic and bioaccumulates and biomagnifies throughout the food chain via dietary uptake of fish, seafood and mammals. Mercury methylation processes in aquatic environments have been found to be exacerbated by ocean warming, coupled with more acidic and anoxic sediments (FAO, 2020). Consumption of mercury-contaminated fish has been found to be linked to neurological disorders due to methyl mercury poisoning (i.e., Minamata disease) that is associated with climate change-contaminant interactions that alter the bioaccumulation and biomagnification of toxic and fat-soluble persistent organic pollutants and polychlorinated biphenyls (PCBs) (Alava et al., 2017) in seafood and marine mammals (medium confidence). Indigenous Peoples have a higher exposure to such risks because of the accumulation of such toxins in traditional foods (J.J. et al., 2017). Contamination of food with PCBs and dioxins has a range of adverse health impacts (Lake et al., 2015).
Chapter 5 (Sections 5.4.3, 5.5.2.3, 5.8.1, 5.8.2, 5.8.3, 5.9.1, 5.11.1, 5.11.3, 5.12.3) discusses the possible impacts of climate change on food safety, including exposure to toxigenic fungi, PCBs and other POPs, mercury and harmful algal blooms.
Climate change may affect animal health management practices, potentially leading to an increased use of pesticides or veterinary drugs (such as preventive antimicrobials) that could result in increased levels of residues in foods (high agreement, medium/low evidence) (Beyene et al., 2015; FAO and WHO, 2018; European Food Safety Authority, 2020; MacFadden et al., 2018).
7.2.5 Observed Impacts on Mental Health and Well-Being
7.2.5.1 Observed Impacts on Mental Disorders
A wide range of climatic events and conditions have observed and detrimental impacts on mental health (very high confidence). The pathways through which climatic events affect mental health are varied, complex and inter-connected with other non-climatic influences that create vulnerability (Figure 7.6). The climatic exposure may be direct, such as experiencing an extreme weather event or prolonged high temperatures, or indirect, such as mental health consequences of undernutrition or displacement. Exposure may also be vicarious, with people experiencing decreased mental health associated with observing the impact of climate change on others or simply by learning about climate change. Non-climatic moderating influences range from an individual’s personality and pre-existing conditions, to social support, and to structural inequities (Gariepy et al., 2016; Hrabok et al., 2020; Nagy et al., 2018; Silva et al., 2016b). Depending on these background and contextual factors, similar climatic events may result in a range of potential mental health outcomes, including anxiety, depression, acute traumatic stress, PTSD, suicide, substance abuse and sleep problems, with conditions ranging from being mild in nature to those that require hospitalisation (Berry et al., 2010; Cianconi et al., 2020; Clayton et al., 2017; Ruszkiewicz et al., 2019; Bromet et al., 2017; Lowe, 2019). The line between mental health and more general well-being is permeable, but in this section we refer to diagnosable mental disorders—conditions that disrupt or impair normal functioning through impacts on mood, thinking or behaviour.

Figure 7.6 | Climate change impacts on mental health and key adaptation responses. PTSD: Post traumatic stress disorder.
There is an observable association between high temperatures and mental health decrements (high confidence), with an additional possible influence of increased precipitation (medium agreement, medium evidence). Heat-associated mental health outcomes include suicide (Williams et al., 2015a; Carleton, 2017; Burke et al., 2018; Kim et al., 2019b; Thompson et al., 2018; Schneider et al., 2020; Cheng et al., 2021; Baylis et al., 2018; Obradovich et al., 2018); psychiatric hospital admissions and emergency room visits for mental disorders (Hansen et al., 2008; Wang et al., 2014; Chan et al., 2018; Mullins and White, 2019; Yoo et al., 2021); experiences of anxiety, depression and acute stress (Obradovich et al., 2018; Mullins and White, 2019); and self-reported mental health (Li et al., 2020). In Canada, Wang et al. (2014) found an association between mean heat exposure of 28°C and greater hospital admissions within 0 to 4 days for mood and behavioural disorders (including schizophrenia, mood and neurotic disorders). A US study found mental health problems increased by 0.5% when average temperatures exceed 30°C, compared to averages between 25°C and 30°C; a 1°C warming over five years was associated with a 2% increase in mental health problems (Obradovich et al., 2018). Another study found a 1°C rise in monthly average temperatures over several decades was associated with a 2.1% rise in suicide rates in Mexico and a 0.7% rise in suicide rates in the USA (Burke et al., 2018). A systematic review of published research using a variety of methodologies from 19 countries (Thompson et al., 2018) found an increased risk of suicide associated with a 1°C rise in ambient temperature.
Discrete climate hazards including storms (Kessler et al., 2008; Boscarino et al., 2013; Boscarino et al., 2017; Obradovich et al., 2018), floods (Baryshnikova and Pham, 2019), heatwaves, wildfires and drought (Hanigan et al., 2012; Carleton, 2017; Zhong et al., 2018; Charlson et al., 2021) have significant negative consequences for mental health (very high confidence). A large body of research identifies the impacts of extreme weather events on PTSD, anxiety and depression; much of the research has been done in the USA and the UK, but a growing number of studies find evidence for similar impacts on mental health in other countries, including Spain (Foudi et al., 2017), Brazil (Alpino et al., 2016), Chile (Navarro et al., 2016), Small Island Developing States (Kelman et al., 2021) and Vietnam (Pollack et al., 2016). Approximately 20–30% of those who live through a hurricane develop depression and/or PTSD within the first few months following the event (Obradovich et al., 2018; Schwartz et al., 2015; Whaley, 2009), with similar rates for people who have experienced flooding (Waite et al., 2017; Fernandez et al., 2015). Studies conducted in South America and Asia indicate an increase in PTSD and depressive disorders after extreme weather events (Rataj et al., 2016). Evidence is lacking for African countries (Otto et al., 2017). Children and adolescents are particularly vulnerable to post-traumatic stress after extreme weather events (Brown et al., 2017; Hellden et al., 2021; Kousky, 2016), and increased susceptibility to mental health problems may linger into adulthood (Maclean et al., 2016).
Wildfires have observed negative impacts on mental health (high confidence). This is due to the trauma of the immediate experience and/or subsequent displacement and evacuation (Dodd et al., 2018; Brown et al., 2019; Psarros et al., 2017; Silveira et al., 2021b). Sub-clinical outcomes, such as increases in anxiety, sleeplessness or substance abuse are reported in response to wildfires and extreme weather events, with impacts being pronounced among those who experience greater losses or are more directly exposed to the event; this may include first responders.
Mental health impacts can emerge as result of climate impacts on economic, social and food systems (high confidence). For example, malnutrition among children has been associated with a variety of mental health problems (Adhvaryu et al., 2019; Hock et al., 2018; Yan et al., 2018), as has food insecurity among adults (Lund et al., 2018). The economic impacts of droughts have been associated with increases in suicide, particularly among farmers (Carleton, 2017; Edwards et al., 2015; Vins et al., 2015); those whose occupations are likely to be affected by climate change report that it is a source of stress that is linked to substance abuse and suicidal ideation (Kabir, 2018). Studies of Indigenous Peoples often describe food insecurity or reduced access to traditional foods as a link between climate change and reduced mental health (Middleton et al., 2020b). The loss of family members, for example due to an extreme weather event, increases the risk of mental illness (Keyes et al., 2014). Individuals in low- and middle-income countries may be more severely impacted due to lesser access to mental health services and lower financial resources to help cope with impacts compared with high-income countries (Abramson et al., 2015).
Anxiety about the potential risks of climate change and awareness of climate change itself can affect mental health even in the absence of direct impacts (low confidence). There is a need for more evidence about the prevalence or severity of climate change-related anxiety, sometimes called ecoanxiety, but national surveys in the USA, Europe and Australia show that people express high levels of concern and perceived harm associated with climate change (Steentjes et al., 2017; Clayton and Karazsia, 2020; Cunsolo and Ellis, 2018; Helm et al., 2018; Leiserowitz et al., 2017; Reser et al., 2012; Steentjes et al., 2017). In a US sample, perceived ecological stress, defined as personal stress associated with environmental problems, predicted depressive symptoms (Helm et al., 2018); in a sample of Filipinos, climate anxiety was correlated with lower mental health (Reyes et al., 2021) and a non-random study in 25 countries showed positive correlations between negative emotions about climate change and self-rated mental health (Ogunbode et al., 2021). However, an earlier study found no correlation between climate change worry and mental health issues (Berry and Peel, 2015). Because the perceived threat of climate change is based on subjective perceptions of risk and coping ability as well as on experiences and knowledge (Bradley et al., 2014), even people who have not been directly affected may be stressed by a perception of looming danger (Clayton and Karazsia, 2020). Not surprisingly, those who have directly experienced some of the effects of climate change may be more likely to show such responses. Indigenous Peoples, whose culture and well-being tend to be strongly linked to local environments, may experience mental health effects associated with changes in environmental risks; studies suggest connections to an increase in depression, substance abuse or suicide in some Indigenous Peoples (Canu et al., 2017; Cunsolo Willox et al., 2013; Middleton et al., 2020b; Jaakkola et al., 2018).
7.2.5.2 Observed Impacts on Well-Being
Overall, research suggests that climate change has already had negative effects on subjective well-being (medium confidence). C limate change can affect well-being through a number of pathways, including loss of access to green and blue spaces due to damage from storms, coastal erosion, drought or wildfires; heat; decreased air quality; and disruptions to one’s normal pattern of behaviour, residence, occupation or social interactions (Hayward and Ayeb-Karlsson, 2021). For example, substantial evidence shows a negative correlation between air pollution and subjective well-being or happiness (Apergis, 2018; Cunado and de Gracia, 2013; Lu, 2020; Luechinger, 2010; Menz and Welsch, 2010; Orru et al., 2016; Yuan et al., 2018; Zhang et al., 2017a); in the reverse direction, there is evidence not only that time in nature but more specifically a feeling of connectedness to nature are both associated with well-being (Martin et al., 2020) and healthy ecosystems offer opportunities for health improvements (Pretty and Barton, 2020). Negative emotions such as grief—often termed ‘solastalgia’ (Albrecht et al., 2007)—are associated with the degradation of local or valued landscapes (Eisenman et al., 2015; Ellis and Albrecht, 2017; Polain et al., 2011; Tschakert et al., 2017; Tschakert et al., 2019), which may threaten cultural rituals, especially among Indigenous Peoples (Cunsolo and Ellis, 2018; Cunsolo et al., 2020). Studies conducted in the Solomon Islands and Tuvalu found qualitative and quantitative evidence of experiences of climate change and worry about the future, with negative impacts on respondents’ well-being (Asugeni et al., 2015; Gibson et al., 2020).
Heat is one of the best-studied aspects of climate change observed to reduce well-being (high confidence). Higher summer temperatures are associated with decreased happiness and ratings of well-being (Carleton and Hsiang, 2016; Miles-Novelo and Anderson, 2019; Connolly, 2013; Noelke et al., 2016; Baylis et al., 2018; Moore et al., 2019; Wang et al., 2020 b). A study of 1.9 million Americans (Noelke et al., 2016) found that exposure to one day averaging 21°C–27°C was associated with reduced well-being by 1.6% of a standard deviation and days above 32°C were associated with reduced well-being by 4.4% of a standard deviation relative to a reference interval of 10°C–16°C. A similar relationship between heat and mood has been observed in China, where expressed mood began to decrease when the average daily temperature was over 20°C (Wang et al., 2020 b). The causal mechanism is unclear but could be due to impacts on health, economic costs or social interactions (Belkin and Kouchaki, 2017; Osberghaus and Kühling, 2016) or reduced quality or quantity of sleep (Fujii et al., 2015; Obradovich et al., 2017; Obradovich and Migliorini, 2018). Heat has also been associated with inter-personal and inter-group aggression and increases in violent crime (Heilmann et al., 2021; Mapou et al., 2017; Tiihonen et al., 2017). For the most part, studies have measured daily response to average daily temperatures and are unable to predict whether the effect is cumulative in response to a sequence of unusually warm days. However, there is no evidence that adaptation occurs over time to eliminate the negative response to very warm temperatures (Moore et al., 2019). Some research has found a negative effect of extreme cold on well-being (Yoo et al., 2021); increasing winter temperatures associated with climate change could serve to compensate for the impact of increased summer temperatures. However, the effect of high temperatures is typically found to be stronger than the effect of low temperatures, and in some cases no detrimental impacts of cold weather are found (Almendra et al., 2019; Mullins and White, 2019).
Climate change also threatens well-being defined in terms of capabilities or the capacity to fulfil one’s potential and fully participate in society. Heat can limit labour capacity; one study estimated that 45 billion hours of labour productivity were lost in 2018 compared to 2000 due to high temperatures (Watts et al., 2019). Both heat and air pollution also impair human capabilities through a negative effect on cognitive performance (Taylor et al., 2016b) and even impair skills acquisition, reducing the ability to learn (Park et al., 2021) and affecting marginalised groups more strongly (Park et al., 2020), although findings are inconsistent and depend in part on the nature of the task (low confidence).
Systematic reviews have found an association between higher ambient levels of fine airborne particles with cognitive impairment in the elderly and with behavioural problems (related to impulsivity and attention problems) in children (Power et al., 2016; Yorifuji et al., 2017; Younan et al., 2018; Zhao et al., 2018b) (medium confidence). Malnutrition has also been associated with reduced educational achievement and long-term decrements in cognitive function (Acharya et al., 2019; Asmare et al., 2018; Na et al., 2020; Kim et al., 2017; Talhaoui et al., 2019).
7.2.6 Observed Impacts on Migration
Consistent with peer-reviewed scholarship and with the United Nations Framework Convention on Climate Change (UNFCCC) Cancun Adaptation Framework section 14(f) and the Paris Agreement, this Chapter assesses the impacts of climate change on four types of migration: (a) adaptive migration (i.e., where migration is an outcome of individual or household choice), (b) involuntary migration and displacement (i.e., where people have few or no options except to move), (c) organised relocation of populations from sites highly exposed to climatic hazards and (d) immobility (i.e., an inability or unwillingness to move from areas of high exposure for cultural, economic or social reasons) (Cross-Chapter Box MIGRATE in Chapter 7).
A general theme across studies from all regions is that climate-related migration outcomes are diverse (high confidence)and may be manifest as decreases or increases in migration flows, and may lead to changes in the timing or duration of migration and to changes in migration source locations and destinations. Multi-country studies of climatic impacts on migration patterns in Africa have found that migration exhibits weak, inconsistent associations with variations in temperature and precipitation and that migration responses differ significantly between countries and between rural and urban areas (Gray and Wise, 2016; Mueller et al., 2020). Multi-directional findings such as these are also common in single-country studies from multiple regions (Call et al., 2017; Nawrotzki et al., 2017; Cattaneo et al., 2019; Kaczan and Orgill-Meyer, 2020). The diversity of potential migration and displacement outcomes reflects (a) the variable nature of climate hazards in terms of the rate of onset, intensity, duration, spatial extent and severity of damage caused to housing, infrastructure and livelihoods and (b) the wide range of social, economic, cultural, political and other non-climatic factors that influence exposure, vulnerability, adaptation options and the contexts in which migration decisions are made (Neumann and Hermans, 2015; McLeman, 2017; Barnett and McMichael, 2018; Cattaneo et al., 2019; Hoffmann et al., 2020) (high confidence).
Weather events and climate conditions can act as direct drivers of migration and displacement (e.g., destruction of homes by tropical cyclones) and as indirect drivers (e.g., rural income losses and/or food insecurity due to heat- or drought-related crop failures that in turn generate new population movements) (high confidence). Extreme storms, floods and wildfires are strongly associated with high levels of short- and long-term displacement, while droughts, extreme heat and precipitation anomalies are more likely to stimulate longer-term changes in migration patterns (Kaczan and Orgill-Meyer, 2020; Hoffmann et al., 2020). Longer-term environmental changes attributable to anthropogenic climate change—such as higher average temperatures, desertification, land degradation, biodiversity loss and sea level rise—have had observed effects on migration and displacement in a limited number of locations in recent decades but are projected to have wider-scale impacts on future population patterns and migration, and are therefore assessed in Section 7.3.2 (Projected Risks).
The diversity of potential migration and displacement outcomes reflects the scale and physical impacts of specific climate hazard events and the wide range of social, economic, cultural, political and other non-climatic factors that influence exposure, vulnerability, adaptation options and the contexts in which migration decisions are made (high confidence). The diversity in drivers, contexts and outcomes makes it difficult to offer simple generalisations about the relationship between climate change and migration. The characteristics of climatic drivers vary in terms of the rate of onset, intensity, duration, spatial extent and severity of damage caused to housing, infrastructure and livelihoods; the potential migration responses to these are further mediated by cultural, demographic, economic, political, social and other non-climatic factors operating across multiple scales (Neumann and Hermans, 2015; McLeman, 2017; Barnett and McMichael, 2018; Cattaneo et al., 2019; Hoffmann et al., 2020).
Climate-related migration and displacement outcomes display high variability in terms of migrant success, often reflecting pre-existing socioeconomic conditions and household wealth (high confidence). The decision to migrate or remain in place when confronted by climatic hazards is strongly influenced by the range and accessibility of alternative, in situ (i.e., non-migration) adaptation options that may be less costly or disruptive (Cattaneo et al., 2019). Migration decisions (whether climate-related or not) are typically made at the individual or household level and are influenced by a household’s perceptions of risk, social networks, wealth, age structure, health and livelihood choices (Koubi et al., 2016b; Gemenne and Blocher, 2017). Households with greater financial resources and higher levels of educational attainment have greater capacity to adapt in situ (Cattaneo and Massetti, 2019; Ocello et al., 2015) but are also better able to migrate and with greater agency once such a decision is made (Kubik and Maurel, 2016; Koubi et al., 2016b; Riosmena et al., 2018; Adams and Kay, 2019). By contrast, poor households with limited physical, social and financial resources have less capacity to adapt in situ and are often limited in their migration options (Nawrotzki and DeWaard, 2018; Suckall et al., 2017; Zickgraf et al., 2016). Thus, when poorer households do migrate after an extreme climate event, it is often in reaction to lost income or livelihood and occurs with low voluntarity (Mallick et al., 2017; Bhatta et al., 2015) and may perpetuate or amplify migrants’ socioeconomic precarity and/or their exposure to environmental hazards (Natarajan et al., 2019; see also Section 8.3.1).
Climate-related migration originates most often in rural areas in low- and middle-income countries, with migrant destinations usually being other rural areas or urban centres within their home countries (i.e., internal migration) (medium confidence). Rural livelihoods and incomes based on farming, livestock rearing and/or natural resource collection are inherently sensitive to climate variability and change, creating greater potential for migration as a response (Bohra-Mishra et al., 2017 ; Viswanathan and Kumar, 2015). Drought events have been associated with periods of higher rural to urban migration within Mexico (Chort and de la Rupelle, 2016; Leyk et al., 2017; Nawrotzki et al., 2017; Murray-Tortarolo and Martnez, 2021) and Senegal (Nawrotzki and Bakhtsiyarava, 2017). Extreme temperatures are associated with higher rates of temporary rural out-migration in South Africa and in Bangladesh (Mastrorillo et al., 2016; Call et al., 2017). In rural Tanzania, weather-related shocks to crop production have been observed to increase the likelihood of migration but typically only for households in the middle of community wealth distribution (Kubik and Maurel, 2016). Weather-related losses in rice production have been associated with small-percentage increases in internal migration in India (Viswanathan and Kumar, 2015) and the Philippines (Bohra-Mishra et al., 2017 ). In east Africa, temporary rural–urban labour migration does not show a strong response to climatic drivers (Mueller et al., 2020). There is limited literature on mobility as adaptation in urban populations, with the focus being on resettlement of flood-prone informal settlements within cities (Kita, 2017; Tadgell et al., 2017).
Most documented examples of international climate-related migration are intra-regional movements of people between countries with shared borders (high agreement, medium evidence). Systematic reviews find few documented examples of long-distance, inter-regional migration driven by climate events (Veronis et al., 2018; Kaczan and Orgill-Meyer, 2020; Hoffmann et al., 2020). One macro-economic analysis found a correlation between migrant flows from low- to high-income countries and adverse climatic events in the source country (Coniglio and Pesce, 2015). Another study found that high heat stimulates higher rates of international migration from middle-income countries but typically not from low-income countries (Cattaneo and Peri., 2016), while other studies found international climate-related migration originates primarily from agriculture-dependent countries (Cai et al., 2016; Nawrotzki and Bakhtsiyarava, 2017). Small-sample studies of migrants to Canada from Bangladesh, Haiti and sub-Saharan Africa suggest environmental factors in the source country can be a primary or secondary motivation for some migrants within larger flows of economic and family-reunification migrants (Veronis and McLeman, 2014; Mezdour et al., 2015; McLeman et al., 2017). Research on the links between climate hazards and international movements of refugees and/or asylum seekers shows differing results. One study found that asylum applications in Europe increase during climate fluctuations due to interactions with conflict (Missirian and Schlenker, 2017), and another found links between heat, drought, conflict and asylum-seeking migration originating in the Middle East between 2011 and 2015 (Abel et al., 2019). Other studies have found that asylum claims in Europe correspond minimally with climatic hazards in source countries (Schutte et al., 2021), with choices in baseline data, timeframes for analysis and methodological approaches potentially explaining the inconsistent results across studies (Boas et al., 2019). Media reports and other studies in recent years suggest that climate change has driven large numbers of migrants to the US from Central America and to Europe from the Middle East and Africa, but empirical studies were not identified for this assessment.
7.2.6.1 Relative Importance of Specific Climatic Drivers of Migration and Displacement
Reliable global estimates of voluntary climate-related migration within and between countries are not available due to a general absence of data of this specific nature, with existing national and global datasets often lacking information on migration causation or motivation. Better data are available for involuntary displacements within countries for reasons associated with weather-related hazards. Data collected annually since 2008 on internal displacements attributed to extreme weather events by the IDMC indicate that extreme storms and floods are the two most significant weather-related drivers of population displacements globally. Because of improvements in collection sources and methods since it first began reporting data in 2008, upward trends since that year in the total reported annual number of people displaced should be treated cautiously. However, it is reasonable to conclude that the average annual rate currently exceeds 20 million people globally, with considerable interannual variation due to the frequency and severity of extreme events in heavily populated areas. Regional distribution of displacement events has been consistent throughout the IDMC data collection period (high confidence), with displacement events occurring most often in East, Southeast and south Asia; sub-Saharan Africa; the USA; and the Caribbean region (Figure 7.7). Relative to their absolute population size, small island states experience a disproportionate risk of climate-related population displacements (Desai et al., 2021) (high confidence).
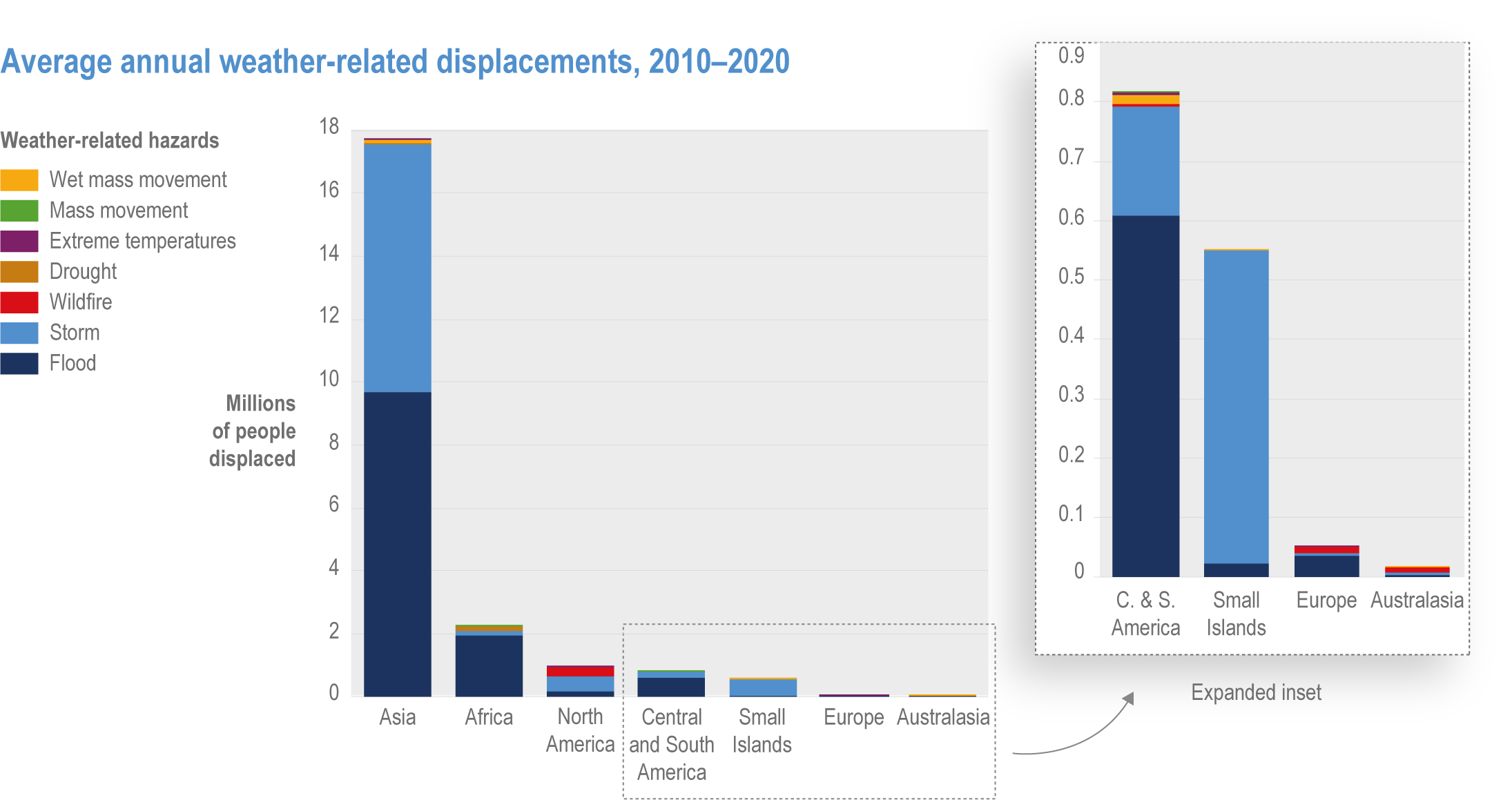
Figure 7.7 | Average number of people displaced annually by selected weather-related events from 2010 to 2020 by region. See text for important notes regarding data collection and trends. Source statistics provided by the Internal Displacement Monitoring Centre (https://www.internal-displacement.org/).
Tropical cyclones and extreme storms are a particularly significant displacement risk in East and Southeast Asia, the Caribbean region, the Bay of Bengal region and southeast Africa (IDMC 2020) (high confidence). The scale of immediate displacement from any given storm and potential for post-event migration depend heavily on the extent of damage to housing and livelihood assets and the responsive capacity of governments and humanitarian relief agencies (Saha, 2016; Islam et al., 2018; Mahajan, 2020; Spencer and Urquhart, 2018). In Bangladesh, the rural poor are most often displaced, with initial increases in short-term, labour-seeking migration followed by more permanent migration by some groups (Saha, 2016; Islam and Hasan, 2016; Islam and Shamsuddoha, 2017). Past hurricanes in the Caribbean basin have generated internal and inter-state migration within the region, typically along pre-existing social networks, and to the USA (Loebach, 2016; Chort and de la Rupelle, 2016). In 2017, Hurricanes Irma and Maria caused widespread damage to infrastructure and health services, and a slow recovery response by authorities was followed by the migration of tens of thousands of Puerto Ricans to Florida and New York (Zorrilla, 2017; Echenique and Melgar, 2018). In the US, coastal counties experience increased out-migration after hurricanes that flows along existing social networks (Hauer, 2017), with post-disaster reconstruction employment opportunities potentially attracting new labour migrants to affected areas (Ouattara and Strobl, 2014; Curtis et al., 2015; DeWaard et al., 2016; Fussell et al., 2018).
Riverine flood displacement can lead to increases or decreases in temporary or short-distance migration flows, depending on the local context (medium confidence) (Robalino et al., 2015; Ocello et al., 2015; Afifi et al., 2016; Koubi et al., 2016b). Floods are a particularly important driver of displacement in river valleys and deltas in Asia and Africa, although large flood-related displacements have been recorded by the IDMC in all regions. In Africa, populations exposed to low flood risks, as compared with other regions, are observed to have a greater vulnerability to displacement due to limited economic resources and adaptive capacity (Kakinuma et al., 2020). In areas where flooding is especially frequent, in situ adaptations may be more common, and out-migration may temporarily decline after a flood (Afifi et al., 2016; Chen et al., 2017; Call et al., 2017). Rates of indefinite or permanent migration tend not to change following riverine floods unless damage to homes and livelihood assets is especially severe and widespread, with household perceptions of short- and longer-term risks playing an important role (Koubi et al., 2016a).
Displacements due to droughts, extreme heat and associated impacts on food and water security are most frequent in east Africa and, to a lesser extent, south Asia and west and southern Africa (IDMC, 2020). Since droughts unfold progressively and typically do not cause permanent damage to housing or livelihood assets, there is greater opportunity for government and non-governmental organisation (NGO) interventions and greater use of in situ adaptation options (Koubi et al., 2016b; Koubi et al., 2016a; Cattaneo et al., 2019). Drought-related population movements are most common in dryland rural areas of low-income countries and occur after a threshold is crossed and in situ adaptation options are exhausted (Gautier et al., 2016; Wiederkehr et al., 2018; McLeman, 2017). Observed population movements may occur for an extended period after the event; one study of Mexican data found this lag to be up to 36 months (Nawrotzki et al., 2017). The most common response to drought is an increase in short-distance, rural–urban migration (medium confidence), with examples being documented in Bangladesh, Ethiopia, Pakistan, sub-Saharan Africa, Latin America and Brazil (Neumann and Hermans, 2015; Gautier et al., 2016; Gautier et al., 2016; Mastrorillo et al., 2016; Baez et al., 2017; Call et al., 2017; Nawrotzki et al., 2017; Jessoe et al., 2018 ; Carrico and Donato, 2019; Hermans and Garbe, 2019).
Few assessable studies were identified that examine links between wildfires and migration. Wildfire events are often associated with urgent evacuations and temporary relocations, which place significant stress on receiving communities (Spearing and Faust., 2020), but research in the USA suggests fires have only a modest influence on future migration patterns in exposed areas (Winkler and Rouleau., 2021). More research, particularly in other regions, is needed.
7.2.6.2 Immobility and Resettlement in the Context of Climatic Risks
Immobility in the context of climatic risks can reflect vulnerability and lack of agency (an inability to migrate), but can also be a deliberate choice (high confidence). Research since AR5 shows that immobility is best described as a continuum from people who are financially or physically unable to move away from hazards (involuntary immobility) to people who choose not to move (voluntary immobility) because of strong attachments to place, culture and people (Nawrotzki and DeWaard, 2018; Adams, 2016; Farbotko and McMichael, 2019; Zickgraf, 2019; Neef et al., 2018; Suckall et al., 2017; Ayeb-Karlsson et al., 2018; Zickgraf, 2018; Mallick and Schanze, 2020). Involuntary immobility is associated with individuals and households with low adaptive capacity and high exposure to hazard, and can exacerbate inequality and future vulnerability to climate change (Sheller, 2018), including through impacts on health (Schwerdtle et al., 2018). Voluntary immobility represents an assertion of the importance of culture, livelihoods and people to well-being, and is of particular relevance for Indigenous Peoples (Suliman et al., 2019).
Planned relocations by governments of settlements and populations exposed to climatic hazards are not presently commonplace, although the need is expected to grow in coming decades (Hino et al 2017). Examples include relocations of coastal settlements exposed to storm and erosion hazards as well as smaller numbers of cases of flood-prone settlements in river valleys; these examples suggest that organised relocations are expensive, contentious, create multiple challenges for governments and generate short- and longer-term disruptions for the people involved (high agreement, medium evidence) (Ajibade et al., 2020; Henrique and Tschakert, 2020; Desai et al., 2021).
Examples of relocations of small indigenous communities in coastal Alaska and villages in the Solomon Islands and Fiji suggest that relocated people experience significant financial and emotional distress as cultural and spiritual bonds to place and livelihoods are disrupted (Albert et al., 2018; Neef et al., 2018; McMichael and Katonivualiku, 2020; McMichael and Katonivualiku, 2020; McMichael et al., 2021; Piggott-McKellar et al., 2019; Bertana, 2020). Voluntary relocation programmes offered by US state governments in communities damaged by Hurricane Sandy in 2012 have been subject to multiple studies, and these show longer-term economic outcomes, social connections and mental well-being vary for a range of reasons unrelated to the impacts of the hazard event itself (Bukvic and Owen, 2017; Binder et al., 2019; Koslov and Merdjanoff, 2021).
7.2.6.3 Connections Between Climate-Related Migration and Health
The number of assessable peer-reviewed studies that make connections between climate-related migration and health and well-being is small. The health outcomes of migrants generally, and of climate-migrants in particular, vary according to geographical context, country and the particular circumstances of migration or immobility (Hunter and Simon, 2017; Hunter et al., 2021; Schwerdtle et al., 2020). Such linkages are ‘multi-directional’, with studies suggesting that healthy individuals may be more likely to migrate internationally in search of economic opportunities than people in poorer health, except during adverse climatic conditions when migration rates may change across all groups, and that migrants may have different long-term health outcomes than people born in destination areas, potentially displaying a range of positive and negative health outcomes compared to non-migrants (Kennedy et al., 2015; Dodd et al., 2017; Hunter and Simon, 2017; Riosmena et al., 2017). Refugees and other involuntary migrants often experience higher exposure to disease and malnutrition, adverse indirect health effects of changes in diet or activity and increased rates of mental health concerns. These latter may be attributable to a sense of loss or fear (Schwerdtle et al., 2018; Torres and Casey, 2017) as well as due to the interruption of healthcare; occupational injuries; sleep deprivation; non-hygienic lodgings and insufficient sanitary facilities; heightened exposure to vector- and WBDs; vulnerability to psychosocial, sexual and reproductive issues; behavioural disorders; substance abuse; and violence (Farhat et al., 2018; Wickramage et al., 2018) (high confidence). Linkages between climate migration and the spread of infectious disease are bidirectional; migrants may be exposed to diseases at the destination to which they have lower immunity than the host community; in other cases, migrants could introduce diseases to the receiving community (McMichael, 2015). Thus, receiving areas may have to pay greater attention to building migrant sensitive health systems and services (Hunter and Simon, 2017). The risk of migration leading to disease transmission is exacerbated by weak governance and lack of policy to support public health measures and access to medicines (Pottie et al., 2015).
Cross-Chapter Box MIGRATE | Climate-Related Migration
Authors: David Wrathall (USA, Chapter 8), Robert McLeman (Canada, Chapter 7), Helen Adams (United Kingdom, Chapter 7), Ibidun Adelekan (Nigeria, Chapter 9), Elisabeth Gilmore (USA/Canada, Chapter 14), François Gemenne (Belgium, Chapter 8), Nathalie Hilmi (Monaco, Chapter 18), Ben Orlove (USA, Chapter 17), Ritwika Basu (India/United Kingdom, Chapter 18), Halvard Buhaug (Norway, Chapter 16), Edwin Castellanos (Guatemala, Chapter 12), David Dodman (United Kingdom, Chapter 6), Felix Kanungwe Kalaba (Zambia, Chapter 9), Rupa Mukerji (Switzerland/India, Chapter 18), Karishma Patel (USA, Chapter 1), Chandni Singh (India, Chapter 10), Philip Thornton (United Kingdom, Chapter 5), Christopher Trisos (South Africa, Chapter 9), Olivia Warrick (New Zealand, Chapter 15), Vishnu Pandey (Nepal, Chapter 4)
Key messages on migration in this report
Migration is a universal strategy that individuals and households undertake to improve well-being and livelihoods in response to economic uncertainty, political instability and environmental change (high confidence). Migration, displacement and immobility that occur in response to climate hazards are assessed in general in Chapter 7, with specific sectoral and regional dimensions of climate-related migration assessed in sectoral and regional Chapters 5 to 15 (Table MIGRATE.1 in Chapter 7) and involuntary immobility and displacement being identified as representative key risks in Chapter 16 (Sections 16.2.3.8, 16.5.2.3.8). Since AR5 there has been a considerable expansion in research on climate–migration linkages, with five key messages from the present assessment report warranting emphasis.
Climatic conditions, events and variability are important drivers of migration and displacement (high confidence) (Table MIGRATE.1 in Chapter 7), with migration responses to specific climate hazards being strongly influenced by economic, social, political and demographic processes (high confidence) (Sections 7.2.6, 8.2.1.3). Migration is among a wider set of possible adaptation alternatives and often emerges when other forms of adaptation are insufficient (Sections 5.5.1.1, 5.5.3.5, 7.2.6, 8.2.1.3, 9.7.2). Involuntary displacement occurs when adaptation alternatives are exhausted or not viable and reflects non-climatic factors that constrain adaptive capacity and create high levels of exposure and vulnerability (high confidence) (Cross-Chapter Box SLR in Chapter 3; Sections 4.3.7, 7.2.6; Box 8.1; Section 10.3; Box 14.7). There is strong evidence that climatic disruptions to agricultural and other rural livelihoods can generate migration (high confidence) (Sections 5.5.4, 8.2.1.3, 9.8.3; Box 9.8).
Specific climate events and conditions may cause migration to increase, decrease or flow in new directions (high confidence), and the more agency migrants have (i.e., the degree of voluntarity and freedom of movement), the greater the potential benefits for sending and receiving areas (high agreement, medium evidence) (Sections 5.5.3.5, 7.2.6, 8.2.1.3; Box 12.2). Conversely, displacement or low-agency migration is associated with poor outcomes in terms of health, well-being and socioeconomic security for migrants and returns fewer benefits to sending or receiving communities (high agreement, medium evidence) (Sections 4.3.7, 4.5.7; Box 8.1; Sections 9.7.2, 10.3; Box 14.7).
Most climate-related migration and displacement observed currently takes place within countries (high confidence) (Sections 4.3.7, 4.5.7, 5.12.2, 7.2.6). The climate hazards most commonly associated with displacement are tropical cyclones and flooding in most regions, with droughts being an important driver in sub-Saharan Africa, parts of south Asia and South America (high confidence) (Sections 7.2.6.1, 9.7.2, 10.4.6.3, 11.4.1, 12.5.8.4, 13.8.1.3, 14.4.7.3). Currently, observed international migration associated with climatic hazards is considerably smaller relative to internal migration and is most often observed as flowing between states that are contiguous and have labour-migration agreements and/or longstanding cultural ties (high agreement, robust evidence) (Sections 4.3.7, 4.5.7, 5.12.2, 7.2.6).
In many regions, the frequency and/or severity of floods, extreme storms and droughts is projected to increase in coming decades, especially under high-emissions scenarios (WGI AR6 Chapter 12 (Ranasinghe et al. 2021)), raising future risk of displacement in the most exposed areas (high confidence) (Section 7.3.2.1). The additional impacts of climate change anticipated to generate future migration and displacement include mean sea level rise that increases flooding and saltwater contamination of soil and/or groundwater in low-lying coastal areas and small islands (high confidence) (Section 7.3.2.1; Cross-Chapter Box SLR in Chapter 3) and more frequent extreme heat events that threaten the habitability of urban centres in the tropics and arid/semiarid regions (medium confidence), although the causal links between heat and migration are less clear (Section 7.3.2.1).
There is growing evidence about the future prospects of immobile populations: groups and individuals that are unable or unwilling to move away from areas highly exposed to climatic hazards (high confidence) (Sections 4.6.9, 7.2.6.2; Box 8.1; Box 10.2). Involuntarily immobile populations may be anticipated to require government interventions to continue living in exposed locations or to relocate elsewhere (high agreement, medium evidence) (Box 8.1). Managed retreat and organised relocations of people from hazardous areas in recent years have proven to be politically and emotionally charged, socially disruptive and costly (high confidence) (Section 7.4.5.4).
Climate-migration interactions and outcomes
Figure MIGRATE.1 in Chapter 7 presents a simplified framework for understanding how migration and displacement may emerge from the interactions of climatic and non-climatic factors, based on the characteristic risk framework introduced in Chapter 1 (Section 1.3). Voluntary migration can be used by households when adapting to climate hazards, while less voluntary forms of migration and displacement emerge when other forms of adaptation (referred to in Figure MIGRATE.1 in Chapter 7 as in situ adaptation) are inadequate. Migration outcomes—expressed in Figure MIGRATE.1 in Chapter 7 as changes in future risks to the well-being of migrants, sending communities and destination communities—are heavily influenced by the political, legal, cultural and socioeconomic conditions under which migration occurs. Groups and individuals that are involuntarily immobile may find that their exposure, vulnerability and risk increase over time. Table MIGRATE.1 in Chapter 7 summarises the range of potential migration outcomes that may emerge from this dynamic and indicates specific sections in sectoral and regional chapters of the report that describe examples of each.
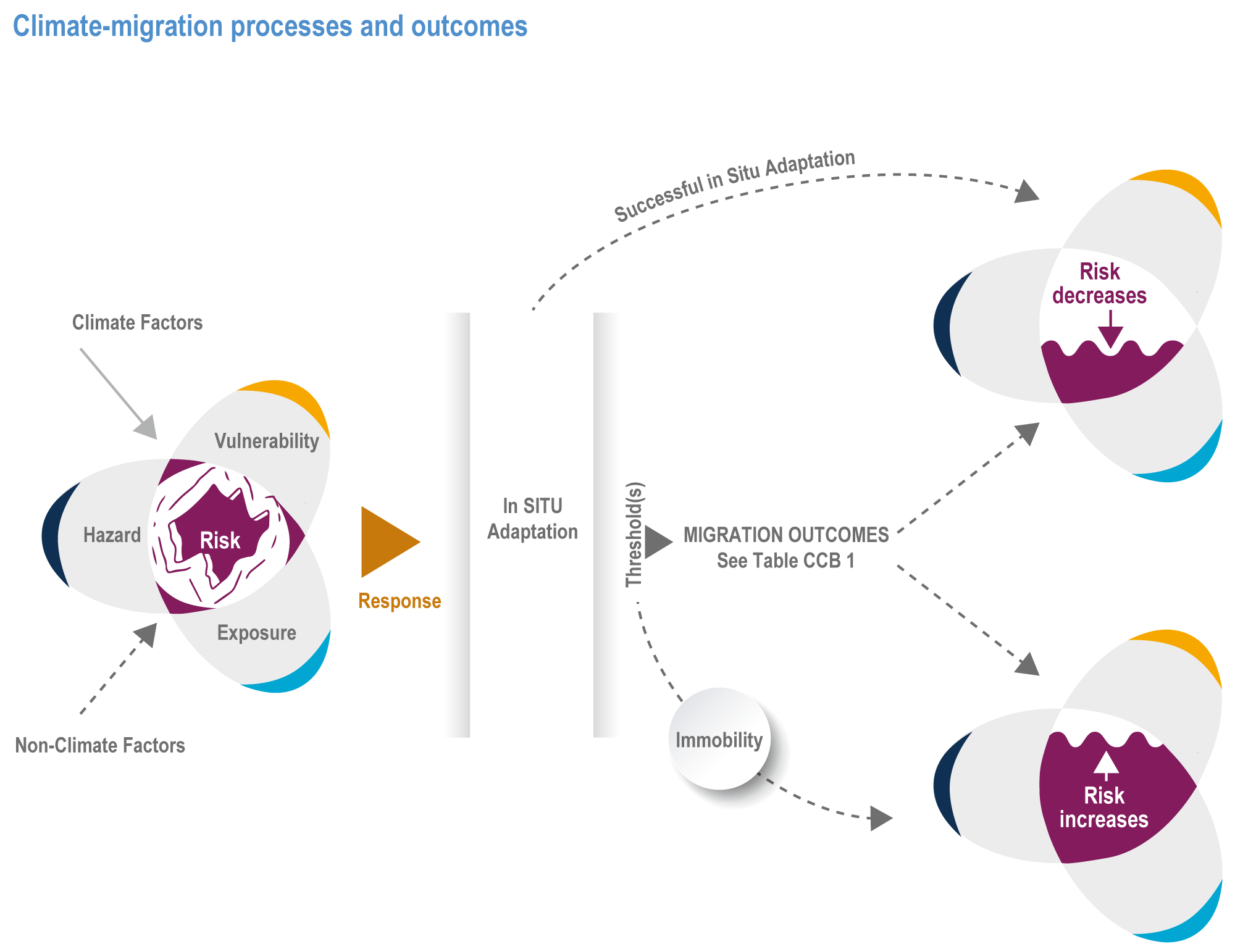
Figure MIGRATE.1 | General interactions between climatic and non-climatic processes, adaptation, potential migration outcomes and implications for future risk. Adapted from McLeman et al. (2021).
Table MIGRATE.1 | Typology of climate-related migration and examples in sectoral and regional chapters of AR6.
Type of climate-related migration | Characteristics | Recent or current examples | Examples in the literature | References in AR6 WGII |
Temporary and/or seasonal migration | Frequently used as a risk-reduction strategy by rural households in less-developed regions with highly seasonal precipitation; includes transhumance | Pastoralists in sub-Saharan Africa; seasonal farm workers in south Asia; rural–urban labour migration in Central America | Afifi et al. (2016); Call et al. (2017); Piguet et al. (2018); Borderon et al. (2019); Cattaneo et al. (2019); Hoffmann et al. (2020); Lopez-i-Gelats et al. (2015); Lu et al. (2016) Kaczan and Orgill-Meyer (2020) | Sections 5.5.1.1, 5.5.3.5; Section 7.2.6; Section 8.2.1.3; Section 9.8.3; Box 13.2 |
Indefinite or permanent migration | Less common than temporary or seasonal migration, particularly when the whole household permanently relocates | Numerous examples in all regions | See reviews listed in cell above | Section 7.2.6; Section 8.2.1.3; Box 10.2 |
Internal migration | Movements within state borders; most common form of climate-related migration | Numerous examples in all regions | See reviews listed in cell above | Section 4.3.7; Sections 5.5.4, 5.10.1.1; Section 7.2.6; Sections 9.7.2, 9.11; Box 9.8; Sections 10.3.3, 10.4.6.3, Box 10.2; Section 11.4.1; Section 12.5.8.4; Section 13.8.1.3; Section 14.4.7.3; Section 15.3.4.6 |
International migration | Less common than internal migration; most often occurs between contiguous countries within the same region; often undertaken for purpose of earning wages to remit home | Cross-border migration within south and Southeast Asia, sub-Saharan Africa | See reviews listed in cell above; also Veronis et al. (2018); McLeman (2019); Cattaneo and G. (2016); Missirian and Schlenker (2017); Schutte et al. (2021) | Sections 4.3.7, 4.5.7; Section 5.12.2; Section 7.2.6 |
Rural–urban or rural–rural | Typically internal but may also flow between contiguous states; may be for temporary or indefinite periods; migration may be undertaken by an individual household member or the entire household; may be followed by remittances | Drought migration in Mexico, east Africa and south Asia | See reviews in the cell above; also Adger et al. (2015); Gautier et al. (2016); Nawrotzki et al. (2017); Wiederkehr et al. (2018); Robalino et al. (2015); Borderon et al. (2019); Murray-Tortarolo and Martnez (2021) | Section 5.13.4; Section 7.2.6; Section 6.2.4.3; Section 8.2.1.3; Section 9.8.1.2; Section 12.5.8.4; Section 14.4.7.1 |
Displacement | Households are forced to leave homes for temporary or indefinite period; typically occurs as a result of extreme events and starts with seemingly temporary evacuation; risk is expected to rise in most regions due to sea level rise and changes in associated coastal hazards | Tropical cyclones in the Caribbean, Southeast Asia and Bay of Bengal region | Islam and Shamsuddoha (2017); Desai et al. (2021); see Internal Displacement Monitoring Centre annual reports for global statistics | Cross-Chapter Box SLR in Chapter 3; Section 4.3.7; 4.5.7; Cross-Chapter Box MOVING PLATE in Chapter 5; Section 7.2.6.1; Box 8.1; Section 9.7.2; Section 9.9.2; Section 10.3; Box 14.7; Sections 15.3.4.6; |
Planned and/or organised resettlement | Initiated in areas where settlements become permanently uninhabitable; requires assistance from governments and/or institutions; government-sponsored sedentarisation of pastoral populations | Fiji, Carteret Islands, Papua New Guinea, Gulf of Mexico coast and coastal Alaska, USA | Marino and Lazrus (2015); Hino et al. (2017); McNamara et al. (2018); McMichael and Katonivualiku (2020); Tadgell et al. (2017); Arnall (2014); Wilmsen and Webber (2015) | Section 4.6.9; Sections 5.14.1, 5.14.2; Section 7.4.4.4; Section 10.4.6; Section 15.5.3; CCP2.2.2; CCP6.3.2 |
Immobility | Adverse weather or climatic conditions warrant moving, but households are unable to relocate because of lack of resources or choose to remain because of strong social, economic or cultural attachments to place | Examples in most regions | Adams (2016); Zickgraf (2018); Nawrotzki and DeWaard (2018); Farbotko et al. (2020) | Section 4.6.9; Section 7.2.6.2; Box 8.1; Box 10.2 |
Policy implications
Future migration and displacement patterns in a changing climate will depend not only on the physical impacts of climate change, but also on future policies and planning at all scales of governance (high confidence) (4.6.9, 5.14.1, 5.14.1.2, 7.3.2, 7.4.4, 8.2.1.3; Box 8.1; CCP6.3.2). Policy interventions can remove barriers to and expand the alternatives for safe, orderly and regular migration that allows vulnerable people to adapt to climate change (high confidence) (Section 7.2.6). With adequate policy support, migration in the context of climate change can result in synergies for both adaptation and development (Sections 5.12.2, 7.4.4, 8.2.1.3). Migration governance at local, national and international levels will influence the outcomes of climate-related migration for the migrants themselves as well as for receiving and origin communities (Sections 5.13.4, 7.4.4, 8.2.1.3). At the international level, a number of relevant policy initiatives and agreements, including Global Compacts for Safe, Orderly and Regular Migration and for the protection of Refugees; the Warsaw International Mechanism of the UNFCCC; the Sustainable Development Goals; the Sendai Framework for Disaster Risk Reduction; and the Platform on Disaster Displacement, have already been established, merit continued pursuit and provide potential migration governance pathways (Section 7.4.4). Policy and planning decisions at regional, national and local scales that relate to housing, infrastructure, water provisioning, schools and healthcare are relevant for successful integration of migrants into receiving communities (Sections 5.5.4, 5.10.1.1, 5.12.2, 9.8.3). Policies and practices on movements of people across international borders are also relevant to climate-related migration, with restrictions on movement having implications for the adaptive capacity of communities exposed to climate hazards (Section 7.4.4.2; Box 8.1). Perceptions of migrants and the framing of policy discussions in receiving communities and nations are important determinants of the future success of migration as an adaptive response to climate change (Section 7.4.4.3) (high agreement, medium evidence).
Cross-Chapter Box MIGRATE
Reducing the future risk of large-scale population displacements, including those requiring active humanitarian interventions and organised relocations of people, requires the international community to meet the requirements of the Paris Agreement and take further action to control future warming (high confidence) (Cross-Chapter Box SLR in Chapter 3; Section 7.3.1; Box 8.1). Current emissions pathways lead to scenarios for the period between 2050 and 2100 in which hundreds of millions of people will be at risk of displacement due to rising sea levels, floods, tropical cyclones, droughts, extreme heat, wildfires and other hazards, with land degradation exacerbating these risks in many regions (Section 7.3.2; IPCC 2019b; Cross-Chapter Box SLR in Chapter 3). At high levels of warming, tipping points may exist, particularly related to sea level rise, that, if crossed, would further increase the global population potentially at risk of displacement (Ranasinghe et al. 2021). Populations in low-income countries and small-island states that have historically had low greenhouse gas (GHG) emissions are at particular risk of involuntary migration and displacement due to climate change, reinforcing the urgency for industrialised countries to continue lowering GHG emissions, to support adaptive capacity-building initiatives under the UNFCCC and to meet objectives expressed in the Global Compacts regarding safe, orderly and regular migration and the support and accommodation of displaced people (Sections 4.3.7, 4.5.7, 5.12.2, 7.4.5.5, 8.4.2; Box 8.1; Cross-Chapter Box SLR in Chapter 3).
Box 7.4 | Gender Dimensions of Climate-Related Migration
Migration decision-making and outcomes—in both general terms and in response to climatic risks—are strongly mediated by gender, social context, power dynamics and human capital (Bhagat, 2017; Singh and Basu, 2020; Rao et al., 2019a; Ravera et al., 2016). Women tend to suffer disproportionately from the negative impacts of extreme climate events for reasons ranging from caregiving responsibilities to lack of control over household resources to cultural norms for attire (Belay et al., 2017; Jost et al., 2016). In many cultures, migrants are most often able-bodied, young men (Call et al., 2017; Heaney and Winter, 2016). Women wait longer to migrate because of higher social costs and risks (Evertsen and Van Der Geest, 2019) and barriers such as social structures, cultural practices, lack of education and reproductive roles (Belay et al., 2017; Afriyie et al., 2018; Evertsen and Van Der Geest, 2019).
Research critiques the tendency to portray women as victims of climate hazards rather than recognising differences between women and the potential for women to use their agency and informal networks to negotiate their situations (Eriksen et al., 2015; Ngigi et al., 2017; Pollard et al., 2015; Rao et al., 2019b; Ravera et al., 2016). Migration can change household composition and structure, which in turn affects the adaptive capacity and choices of those who do not move (Rao et al., 2019a; Rao et al., 2019b; Singh, 2019). For example, when only male household members move, the remaining members of the now female-headed household must take on greater workloads (Goodrich et al., 2019; Rao et al., 2019b; Rigg and Salamanca, 2015), leading to increased workload and greater vulnerability for those left behind (Arora et al., 2017; Bhagat, 2017; Flatø et al., 2017; Lawson et al., 2019). It can, however, also increase women’s economic freedom and decision-making capacity, enhance their agency (Djoudi et al., 2016; Rao, 2019) and alter the gendered division of paid work, care and intra-household relations (Rigg et al., 2018; Singh and Basu, 2020), a process that may reduce household vulnerability to extreme climate events (Banerjee et al., 2019b).
7.2.7 Observed Impacts of Climate on Conflict
7.2.7.1 Introduction
In AR5, conflict was addressed in WGII Chapter 12 on human security. The chapter concluded that some of the factors that increase the risk of violent conflict within states are sensitive to climate change (medium evidence, medium agreement ), that people living in places affected by violent conflict are particularly vulnerable to climate change (medium confidence)and that climate change will lead to new challenges to states and will increasingly shape both conditions of security and national security policies (medium evidence, medium agreement ). AR5 characterised a major debate within the field as: authors supporting an association between climate anomalies and conflict that can be extrapolated into the future (e.g., Hsiang et al. (2013); Hsiang and Marshall (2014); Burke et al. (2015a)) and authors arguing that these associations are not universal and break down when contextual, scale and political factors are introduced (e.g., Buhaug et al. (2014); Buhaug (2016)).
Consistent with AR5 findings, there continues to be little observed evidence that climatic variability or change cause violent inter-state conflict. In intra-state settings, climate change has been associated with the onset of conflict, civil unrest or riots in urban settings (high agreement, medium evidence) (Ide (2020), and changes in the duration and severity of existing violent conflicts (Koubi, 2019). Climate change is conceptualised as one of many factors that interact to raise tensions (Boas and Rothe, 2016) through diverse causal mechanisms (Mach et al., 2019; Ide et al., 2020) and as part of the peace-vulnerability-development nexus (Barnett, 2019; Abrahams, 2020; Buhaug and von Uexkull, 2021). New areas of the literature assessed in this report include the security implications of responses to climate change, the gendered dynamics of conflict and exposure to violence under climate change and civil unrest in urban settings. The impact of violent conflict on vulnerability is not addressed in this chapter but does arise in other chapters (Sections 8.3.2.3, 17.2.2.2). Other chapters address non-violent conflict over changing availability and distribution of resources, for example, competing land uses and fish stocks migrating to different territories (Sections 5.8.2.3; 5.8.3, 5.9.3, 5.13, 9.8.1.1, 9.8.5.1). A commonly used definition of armed conflict is conflicts involving greater than 25 battle-related deaths in a year; this number represents the Uppsala Conflict Data Program threshold for inclusion in their database, a core resource in this field.
Climatic conditions have affected armed conflict within countries, but their influence has been small compared to socioeconomic, political and cultural factors (Mach et al., 2019) (high agreement, medium evidence). Inter-group inequality, and consequent relative deprivation can lead to conflict and the negative impacts of climate change lower the opportunity cost of involvement in conflict (Buhaug et al., 2020; Vestby, 2019). Potential pathways linking climate and conflict include direct impacts on physiology from heat or resource scarcity; indirect impacts of climatic variability on economic output, agricultural incomes, higher food prices and increasing migration flows; and the unintended effects of climate mitigation and adaptation policies (Koubi, 2019; Busby, 2018; Sawas et al., 2018). Relative deprivation, political exclusion and ethnic fractionalisation and ethnic grievances are other key variables (Schleussner et al., 2016; Theisen, 2017). Research shows that factors such as land tenure and competing land uses interacting with market-driven pressures and existing ethnic divisions produce conflict over land resources rather than a scarcity of natural resources caused by climate impacts such as drought (high agreement, medium evidence) (Theisen, 2017; Balestri and Maggioni, 2017; Kuusaana and Bukari, 2015; Box 8.3).
7.2.7.2 Impacts of Climate Change and Violent Conflict
Positive temperature anomalies and average increases in temperature over time have been associated with collective violent conflict in certain settings (medium agreement, low evidence). Helman and Zaitchik (2020) find statistical associations between temperature and violent conflict in Africa and the Middle East that are stronger in warmer places and identify seasonal temperature effects on violence. However, they are unable to detect the impact of regional temperature increases on violence. For Africa, Van Weezel (2019) found associations between average increases in temperature and conflict risk. Caruso et al. (2016) found an association between rises in minimum temperature and violence through the impact of temperature on rice yields (Box 9.4). However, the associations between temperature and violence are weak compared to those with political and social factors (e.g., Owain and Maslin (2018)) and research focuses on areas where conflict is already present and, as such, is sensitive to selection bias (Adams et al., 2018). There is a body of literature that finds statistical associations between temperature anomalies and inter-personal violence, crime and aggression in the Global North, predominantly in the USA (e.g., Ranson (2014); Mares and Moffett (2019); Tiihonen et al. (2017); Parks et al. (2020); Section 14.4.8). However, authors have cautioned against extrapolating seasonal associations into long-term trends and against focusing on individual crimes rather than wider social injustices associated with climate change and its impacts (Lynch et al., 2020).
Variation in availability of water has been associated with international political tension and intra-national collective violence (low agreement, medium evidence). Drought conditions have been associated with violence due to impacts on income from agriculture and water and food security, with studies focusing predominantly on sub-Saharan Africa and the Middle East (Ide and Frohlich, 2015; De Juan, 2015; Von Uexkull et al., 2016; Waha et al., 2017; Abbott et al., 2017; D’Odorico et al., 2018). A small set of published studies has argued inconclusively over the role of drought in causing the Syrian civil war (Gleick, 2014; Kelley et al., 2015; Selby et al., 2017; 16.2.3.9). In general, research stresses the underlying economic, social and political drivers of conflict. For example, research on conflict in the Lake Chad region has demonstrated that the lake drying was only one of many factors including lack of development and infrastructure (Okpara et al., 2016; Nagarajan et al., 2018; Tayimlong, 2020). Fewer studies examine the relationship between flooding (excess water) and violence and often rely on migration as the causal factor (see below). However, some studies have shown an association between flooding and civil unrest (Ide et al., 2020; Section 4.3.6; Section 12.5.3; Box 9.4).
Extreme weather events can be associated with increased conflict risk (low agreement, medium evidence). There is the potential for extreme weather events and disasters to cause political instability and increase the risk of violent conflict, although not conclusively (Brzoska, 2018). Post-disaster settings can be used to intensify state repression (Wood and Wright, 2016) and to alter insurgent groups’ behaviour (Walch, 2018). Different stakeholders use disasters to establish new narratives and alter public opinion (Venugopal and Yasir, 2017). Some research has demonstrated how post-disaster activities have had positive impacts on the social contract between people and the state, reducing the risk of conflict by strengthening relations between government and citizens and strengthening the citizenship of marginalised communities (Siddiqi, 2018; Pelling and Dill, 2010; Siddiqi, 2019). However, post-disaster and disaster risk-related activities themselves have limited capacity to support diplomatic efforts to build peace (Kelman et al., 2018).
7.2.7.3 Causal Pathways Between Climate Change Impacts and Violent Conflict
Increases in food prices due to reduced agricultural production and global food price shocks are associated with conflict risk and represent a key pathway linking climate variability and conflict (medium confidence). Increases in food prices are associated with civil unrest in urban areas among populations unable to afford or produce their own food and in rural populations due to changes in availability of agricultural employment with shifting commodity prices (Martin-Shields and Stojetz, 2019). Under such conditions, locally specific grievances, hunger and social inequalities can initiate or exacerbate conflicts. Food price volatility in general is not associated with violence, but sudden food price hikes have been linked to civil unrest in some circumstances (Bellemare, 2015; McGuirk and Burke, 2020; Winne and Peersman, 2019). In urban settings in Kenya, Koren et al. (2021) found an association between food and water insecurity that is mutually reinforcing and associated with social unrest (although insecurity in either food or water on its own was not). Analysing the global food riots in 2007/2008 and 2011, Heslin (2021) stresses the role of local politics and pre-existing grievances in determining whether people mobilise around food insecurity (Chapter 5).
Climate-related internal migration has been associated with the experience of violence by migrants, the prolongation of conflicts in migrant receiving areas and civil unrest in urban areas (medium agreement, low evidence). Research points to the potential for conflict to serve as an intervening factor between climate and migration. However, the nature of the relationship is diverse and context specific. For example, displaced people and migrants may be associated with heightened social tensions in receiving areas through mechanisms such as ecological degradation, reduced access to services and a disturbed demographic balance in the host area (Rüegger and Bohnet, 2020). Ghimire et al. (2015) observed that an influx of flood-displaced people prolonged conflict by causing a lack of access to services for some of the host population and feelings of grievance. Further, migration from drought-stricken areas to local urban centres has been used to suggest a climate trigger for the Syrian conflict (e.g., Ash and Obradovich (2020)). However, this link has been strongly contested by research that contextualises the drought in wider political economic approaches and existing migration patterns (De Châtel, 2014; Fröhlich, 2016; Selby, 2019; 16.2.3.9).
There is some evidence of an association between climate-related rural-to-urban migration and the risk of civil unrest (medium agreement, low evidence). Petrova (2021) found that while migration in general was associated with increased protests in urban receiving areas, the relationship did not hold for hazard-related migration. In other settings, the association of civil unrest with in-migration was found to depend on the political alignment of the host state with the capital (Bhavnani and Lacina, 2015), previous experience of extreme climate hazards (Koubi et al., 2021) and previous experience of violence among migrants (Linke et al., 2018). Climate-related migrants have reported higher levels of perception and experience of violence in their destination (Linke et al., 2018; Koubi et al., 2018). There has been no association established between international migration and conflict. The literature highlights how unjust racial logics may generate spurious links between climate migration and security (Fröhlich, 2016; Telford, 2018).
7.2.7.4 Gendered Dimensions of Climate-Related Conflict
Structural inequalities play out at an individual level to create gendered experiences of violence (high agreement, medium evidence). Violent conflict is experienced differently by men and women because of gender norms that already exist in society and shape vulnerabilities. For example, conflict deepens gendered vulnerabilities to climate change related to unequal access to land and livelihood opportunities (Chandra et al., 2017). Motivations for inter-group violence may be influenced by constructions of masculinity, for example the responsibility to secure their family’s survival or pay dowries (Myrttinen et al., 2017), and gendered roles may incentivise young men to protest or to join non-state armed groups during periods of adverse climate (Myrttinen et al., 2015; Myrttinen et al., 2017; Anwar et al., 2019; Hendrix and Haggard, 2015; Koren and Bagozzi, 2017). Research has found a positive correlation between crop failures and suicides by male farmers who could not adapt their livelihoods to rising temperatures (Bryant and Garnham 2015; Kennedy and King, 2014; Carleton, 2017).
Extreme weather and climate impacts are associated with increased violence against women, girls and vulnerable groups (high agreement, medium evidence). During and after extreme weather events, women, girls and LGBTQI people are at increased risk of domestic violence, harassment, sexual violence and trafficking (Le Masson et al., 2019; Nguyen, 2019;Myrttinen et al., 2015; Chindarkar, 2012). For example, early marriage is used as a coping strategy for managing the effects of extreme weather events (Ahmed et al., 2019) and women are exposed to increase risk of harassment and sexual assault as scarcity and gender-based roles cause them to walk longer distances to fetch water and fuel (Le Masson et al., 2019). Within the household, violent backlash or heightened tensions may arise from changing gender norms as men migrate to find work in post-disaster settings (Stork et al., 2015) and men’s use of negative coping mechanisms, such as alcoholism, when unable to meet norms of providing for the household (Anwar et al., 2019; Stork et al., 2015). Rates of intimate partner violence have been found to increase with higher temperatures (Sanz-Barbero et al., 2018).
7.2.7.5 Observed Impacts on Non-violent Conflict and Geopolitics
Climate adaptation and mitigation projects implemented without taking local interests and dynamics into account have the potential to cause conflict (high agreement, medium evidence). Reforestation or forest management programmes driven by reducing emissions through deforestation, land zoning and managed retreat due to sea level rise have been identified as having the potential to cause friction and conflict within and between groups and communities (de la Vega-Leinert et al., 2018; Froese and Schilling, 2019). Conflict may arise when there is resistance to a proposed project, where interventions favour one group over another, or when projects undermine livelihoods or displace populations (e.g., Nightingale (2017); Sovacool et al. (2015); Sovacool (2018); Corbera (2017); Hunsberger (2018); Sections 4.6.8, 5.13.4, 14.4.7.3). In addition to conflict generated by the poor implementation of land-based climate mitigation and adaptation projects, Gilmore and Buhaug (2021) highlight the links between climate policy and conflict through the potential effects of unequal distribution of economic burdens and fossil fuel markets on economic growth. There is a small literature that draws attention to the potential security of nuclear proliferation, if nuclear energy is increasingly employed as a low-carbon energy source (e.g., Parthemore et al. (2018); Bunn, (2019)).
Economic and social changes due to changes in sea ice extent in the Arctic are anticipated to be managed as part of existing governance structures (high agreement, medium evidence). The opening-up of the Arctic and associated geopolitical manoeuvring for access to shipping routes and sub-sea hydrocarbons is often highlighted as a potential source of climate conflict (e.g., Koivurova (2009); Åtland (2013); Tamnes and Offerdal (2014)). Research assessed in AR5 focused on the potential for resource wars and Arctic land grabs. However, research since AR5 is less sensationalist in its approach to Arctic security, focusing instead on the practicalities of polycentric Arctic governance under climate change, the economic impacts of climate change, protecting the human security of Arctic populations whose autonomy is at risk (Heininen and Exner-Pirot, 2020), understanding how different regions (e.g., the EU) are positioning themselves more prominently in the Arctic space (Raspotnik and Østhagen, 2019) and Arctic Indigenous Peoples’ understanding of security (Hossain, 2016; Chapter 3; Chapter 14; CCP6).
7.3 Projected Future Risks under Climate Change
7.3.1 Projected Future Risks for Health and Well-Being
7.3.1.1 Global Impacts
Climate change is expected to significantly increase the health risks resulting from a range of climate-sensitive diseases and conditions, with the scale of impacts depending on emissions and adaptation pathways in coming decades (very high confidence). Sections 7.3.1.2 to 7.3.1.11 assess the available studies on future projections for risks associated with specific climate-sensitive diseases and conditions previously described in Section 7.2.1. In the case of diabetes, cancer, injuries, mosquito-borne diseases other than dengue and malaria, rodent-borne diseases and most mental illnesses, insufficient literature was found to allow for assessment. Adaptation pathways and options for managing such risks are detailed in Section 7.4.
Even in the absence of further warming beyond current levels, the proportion of the overall global deaths caused by climate-sensitive diseases and conditions would increase marginally by mid-century (high confidence). Two global projections of climate change health impacts have been conducted since AR5. The first focused on cause-specific mortality for eight exposures for 2030 and 2050 for a mid-range emissions scenario (A1b) and three scenarios of economic growth (WHO, 2014). The study estimated that the climate change projected to occur by 2050 (compared to 1961–1990) could result in an excess of approximately 250,000 deaths yr –1, dominated by increases in deaths due to heat (94,000, mainly in Asia and high-income countries), childhood undernutrition (85,000, mainly in Africa but also in Asia), malaria (33,000, mainly in Africa) and diarrhoeal disease (33,000, mainly in Africa and Asia). Overall, more than half of this excess mortality is projected for Africa. Near-term projections (for 2030) are predominantly for childhood undernutrition (95,200 out of 241,000 total excess deaths) (Figure 7.8). The second study (Carleton et al. 2020) focused on all-cause mortality associated with warming under both a high emissions scenario (RCP8.5) and a middle emissions scenario (RCP4.5). The analyses created a metric of death equivalents that accounted for hot and cold temperature-related mortality and the costs of individual level adaptation; no acclimatization or community-level adaptation, such as early warning systems, were incorporated. Average annual temperature-mortality-income per capita relationships estimated from pooled data from 40 predominantly middle- and high-income countries (38% of the world population) were applied worldwide. Under the high emissions scenario, climate change was projected to result in approximately 85 deaths equivalents per 100,000 population.
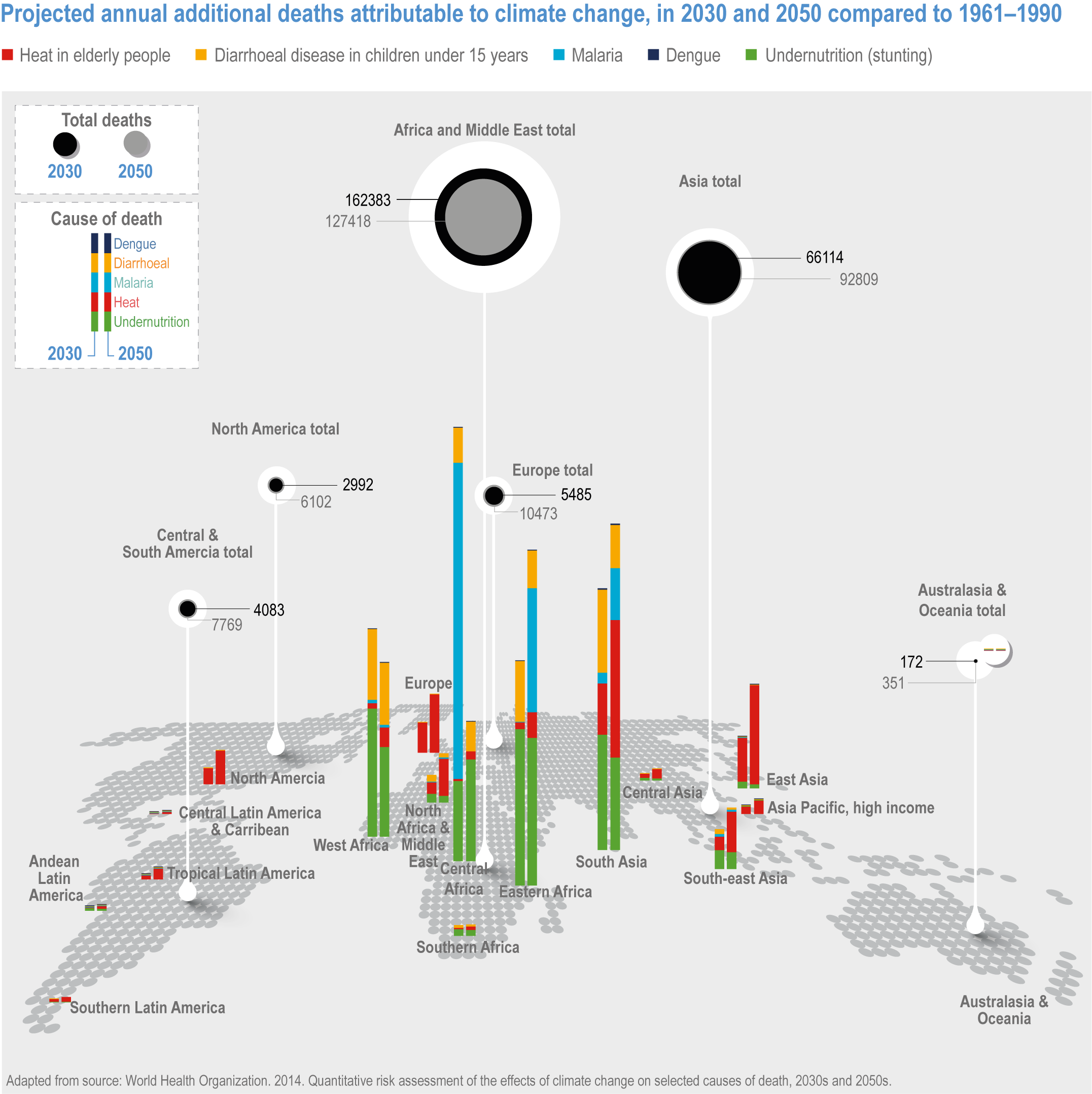
Figure 7.8 | Projected additional annual deaths attributable to climate change in 2030 and 2050 compared to 1961–1990 (WHO, 2014).
Temperature increases are projected to exceed critical risk thresholds for six key climate-sensitive health outcomes, highlighting the criticality of building adaptive capacity in health systems and in other sectors that influence health and well-being (high confidence). Recently reported research illustrates the temperature thresholds under three adaptation scenarios describing the effectiveness of health systems to manage additional risks from climate change for heat-related morbidity and mortality; ozone-related mortality; malaria incidence rates; incidence rates of Dengue and other diseases spread by Aedes sp. mosquitos; Lyme disease; and West Nile fever (Ebi et al., 2021a). As shown in Figure 7.9, these adaptation scenarios significantly alter the warming thresholds at which risks accelerate, with the proactive adaptation scenario, a scenario that emphasises international cooperation towards achieving sustainable development, having the greatest potential to avoid significant increases in risks under all but the highest levels of warming. The incomplete adaptation scenario describes a world with moderate challenges to adaptation and mitigation. The limited adaptation scenario describes a world with high challenges to adaptation and mitigation. In the figure, transitions are based on the peer-reviewed literature projecting risks for each of the health outcomes. Projections for time intervals were changed to temperature increase above pre-industrial levels based on the climate models and scenarios used in the projections.The assessed projections were based on a range of scenarios, including SRES, CMIP5, and ISIMIP, and, in some cases, demographic trends. The black dots are levels of confidence, from very high (four dots) to low (one dot). The diagrams for the proactive and incomplete adaptation scenarios are truncated at the nearest whole °C within the range of temperature change in 2100 under three SSP scenarios used in panel (a) of SPM.3.
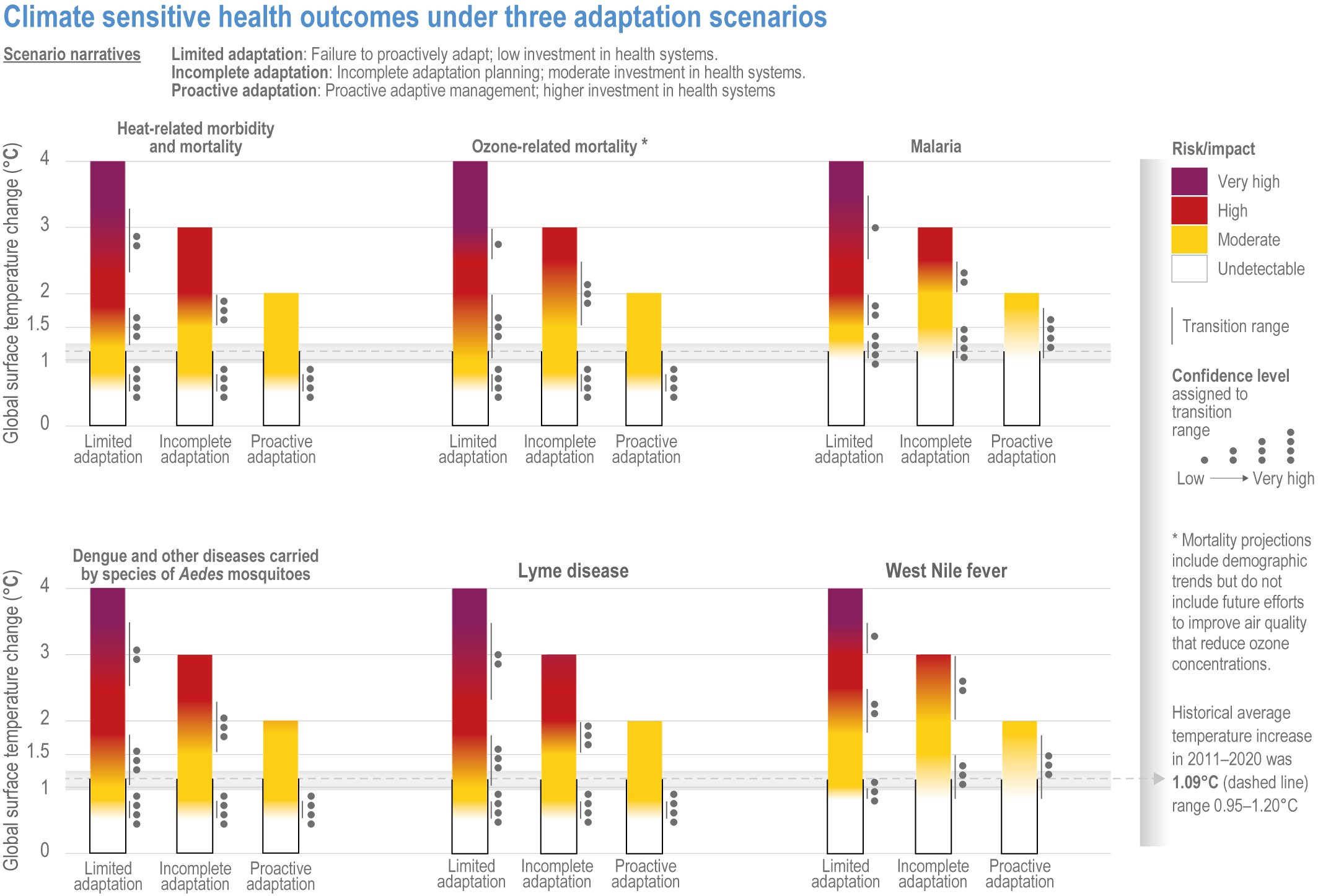
Figure 7.9 | Climate-sensitive human health outcomes under three adaptation scenarios.
7.3.1.2 Projected Changes in Heat- and Cold-Related Exposure and Related Health Outcomes
This section considers the broad impacts of projected changes in heat- and cold-related exposure and related outcomes including mortality and work productivity. Several of the most common heat- and cold-related specific health outcomes (e.g., CVD) are assessed individually in later sections of this chapter.
Population heat exposure will increase under climate change (very high confidence). Since AR5 there has been considerable progress with quantifying future human exposure to extreme heat (Schwingshackl et al., 2021), especially as determined by different combinations of SSPs and RCPs (Chambers, 2020; Cheng et al., 2020; Jones et al., 2018; Liu et al., 2017; Ma and Yuan, 2021; Russo et al., 2019). For example, Table 7.1 shows projections of population exposure to heatwaves, as expressed by the number of person-days, for the 2061–2080 period aggregated by geographical region and SSP/RCP. At the global level, projected future exposure increases from approximately 15 million person-days for the current period to 535 billion person-days for high population growth under the high GHG emission SSP3-RCP8.5 scenario, while for the low population growth/high urbanisation and business as usual SSP5-RCP4.5 scenario, the exposure is substantially lower at 170 billion person-days. Spatial variations in future heatwave frequency and population growth play out in the form of significant geographical contrasts in exposure, with the largest increases projected for low latitude regions such as India and significant portions of sub-Saharan Africa, where increases in heatwave frequency and population are expected. Over East Asia and especially eastern China, exposures are projected to rise, with the effect of increases in heatwave frequency exceeding the countering effect of projected reductions in population, especially in non-urban areas. Further, for North America and Europe, where rural depopulation is projected, the predominant driver of increases in exposure is urban growth (Jones et al., 2018).
Table 7.1 | Projected exposure to heatwaves in millions of person-days by region under different SSP/RCP combinations.
Region | Exposure in millions of person-days | ||||
Current | SSP3-4.5 | SSP5-4.5 | SSP3-8.5 | SSP5-8.5 | |
Global USA North America Europe Latin America and Caribbean North Africa and Middle East Sub-Saharan Africa Russia and Central Asia South Asia East Asia Southeast Asia Oceania | 14,811 375 376 191 803 1,335 1,427 272 7,194 977 711 37 | 244,807 4,769 4,821 2,967 17,287 34,721 67,442 3,074 84,044 12,176 12, 452 247 | 168,488 8,671 8,778 3,775 10,856 23,160 41,339 1,951 53,655 10,855 9,146 492 | 534,848 10,802 10,990 7,326 45,612 65,072 158,290 6,554 146,709 35,381 60,909 822 | 374,269 19,646 20,153 9,969 28,435 43,648 96,054 4,360 94,288 31,918 47,141 1,158 |
Comparisons of heatwave exposure for 1.5°C and 2.0°C warming for different SSPs indicate strong geographical contrasts in potential heatwave risk (high confidence). One global level assessment for a 1.5°C warming projects that low human development index countries will experience exposure levels equal to or greater than the exposure levels for very high human development index countries under a 2°C warming (Russo, 2019). The same assessment also finds that holding global warming below 1.5°C in tandem with achieving sustainable socioeconomic development (e.g., SSP1 as opposed to SSP4) yields reduced levels of heatwave exposure, especially for low human development index countries, particularly across sub-Saharan Africa. Similar findings were found in other global level assessments. Global exposure to extreme heat increases almost 30 times under a SSP3-8.5 combination, with the average exposure for Africa 118 times greater than historical levels, in stark contrast to the four-fold increase projected for Europe. Compared to a SSP3-8.5 scenario, exposure was reduced by 65% and 85% under the SSP2-4.5 and SSP1-2.6 scenarios, respectively (Liu et al., 2017).
Regional level assessments of changes in population heat exposure for Africa, Europe, the USA, China and India corroborate general findings at the global level, that the impact of warming is amplified under divergent regional development pathways (e.g., SSP4 – inequality) compared to those fostering sustainable development (e.g., SSP1 – sustainability) (high confidence) (Rohat et al., 2019a; Weber et al., 2020; Broadbent et al., 2020; Dahl et al., 2019; Harrington and Otto, 2018; Rohat et al., 2019b; Vahmani et al., 2019; Huang and et al., 2018; Zhang et al., 2020a; Liu et al., 2017). For some regions, such as Europe, changes in exposure are projected to be largely a consequence of climate change, while for others, such as Africa and to a lesser extent Asia, Oceania, North America and South America, the interactive effects of demographic and climate change are projected to be important (Jones et al., 2018; Liu et al., 2017; Russo et al., 2016; Ma and Yuan, 2021) (medium confidence).
Compared to research that estimates the temperature only impacts of climate change on heat-related mortality (see below), the number of studies that explicitly model mortality responses considering various combinations of SSPs and RCPs is small and mostly restricted to the country or regional level. These studies point to increases in heat-related mortality especially amongst the elderly across a range of SSPs, with the greatest increases under SSP5 and RCP8.5 (Rail et al., 2019; Yang et al., 2021).
Estimates of heat-related mortality based solely on changes in temperature point to elevated levels of global and regional level mortality compared to the present, with the magnitude of this increasing from RCP4.5 through to RCP8.5 (high confidence) (Ahmadalipour and Moradkhani, 2018; Cheng et al., 2019; Kendrovski et al., 2017; Lee et al., 2020; Limaye et al., 2018; Morefield et al., 2018). Further support comes from the projection that heat-related health impacts for a 2°C increase in global temperatures will be greater than those for 1.5°C warming (very high confidence) (Dosio et al., 2018; Mitchell et al., 2018; King and Karoly, 2017; Vicedo-Cabrera et al., 2018a).
Estimates of future mortality that incorporate adaptation in addition to temperature change point to increases in heat-related mortality under global warming, albeit at lower levels than the case of no adaptation (high confidence) (Anderson et al., 2018; Gosling et al., 2017; Guo et al., 2018; Honda and Onozuka, 2020; Vicedo-Cabrera et al., 2018b; Wang et al., 2018b). Whether adaptation is considered or not, the consensus is Central and South America, southern Europe, southern and Southeast Asia and Africa will be the most affected by climate change in terms of heat-related mortality (high confidence). Similarly, projections of the impacts of future heat on occupational health, worker productivity and workability point to these regions as problematic under climate change (high confidence) (Andrews et al., 2018; de Lima et al., 2021; Dillender, 2021; Kjellstrom et al., 2018; Orlov et al., 2020; Rao et al., 2020; Tigchelaar et al., 2020), especially for occupations with high exposure to heat, such as agriculture and construction. This accords with the findings from independent projections of population heat exposure as outlined above (high confidence).
The effect of climate change on productivity is projected to reduce GDP at a range of geographical scales (high confidence) (Borg et al., 2021; Oppermann et al., 2021; Orlov et al., 2020). For example, measuring economic costs using occupational health and safety recommendations, it was estimated that RCP8.5 would result in a 2.4% reduction in global GDP compared to a 0.5% reduction under RCP2.6 (Orlov et al., 2020). For the USA, it was estimated that the total hours of labour supplied declined ∼0.11% (±0.004%) per degree Celsius increase in global mean surface temperature for low-risk workers and 0.53% (±0.01%) per degree Celsius increase for high-risk workers exposed to outdoor temperatures (Hsiang et al., 2017). Further, a systematic review of the literature indicates that extreme heat exacts a substantial economic burden on health systems, which bears implications for future heat-attributable healthcare costs (Wondmagegn et al., 2019).
Since AR5, there has been an increase in the understanding of the extent to which a warming world is likely to affect cold- or winter-related health impacts. Future increases in heat-related deaths are expected to outweigh those related to cold (high confidence) (Aboubakri et al., 2020; Achebak et al., 2020; Burkart et al., 2021; Huber et al., 2020b; Martinez et al., 2018; Rodrigues et al., 2020; Vardoulakis et al., 2014; Weinberger et al., 2017; Weinberger et al., 2018a; Weitensfelder and Moshammer, 2020). However, strong regional contrasts in heat- and cold-related mortality trends are likely under a RCP8.5 scenario, with countries in the Global North experiencing minimal to moderate decreases in cold-related mortality while warm climate countries in the Global South are projected to experience increases in heat-attributable deaths by the end of the century (Gasparrini et al., 2017; Burkart et al., 2021). Projections of the magnitude of change in the temperature-related burden of disease do, however, demonstrate great variability, due to the application of a wide range of climate change, adaptation and demographic scenarios (Cheng et al., 2019).
A particular focus since AR5 has been the impact of climate change on cities (see AR6 Chapter 6). Heat risks are expected to be greater in urban areas due to changes in regional heat exacerbated by ‘heat island’ effects (high confidence) (Doan and Kusaka, 2018; Heaviside et al., 2016; Li et al., 2021; Rohat et al., 2019a; Rohat et al., 2019c; Varquez et al., 2020; Wouters et al., 2017; Zhao et al., 2021), with intra-urban scale variations in heat exposure attributable to land cover contrasts and urban form and function (Avashia et al., 2021; Jang et al., 2020; Macintyre et al., 2018; Schinasi et al., 2018). However, further research is required to establish the health implications of increasing chronic slow-onset extreme heat (Oppermann et al., 2021) in addition to the acute health outcomes of UHI–heatwave synergies under climate change. The latter is particularly important as studies that address UHI–heatwave interactions have mainly focused on changes in UHI intensity (e.g., Ramamurthy and Bou-Zeid (2017); Scott et al. (2018)). Whether significant urban mortality anomalies arise from the interplay of heatwaves and UHIs largely remains an open question although at least one study demonstrated higher urban compared to rural mortality rates during heatwaves (Ruuhela et al., 2021). The benefits of the winter UHI effect for cold-related mortality remain largely unexplored, but one study for Birmingham, UK, indicates the winter UHI will continue to have a protective effect in future climate (Macintyre et al., 2021).
7.3.1.3 Projected Impacts on Vector-Borne Diseases
The distribution and abundance of disease vectors, and the transmission of the infections that they carry, are influenced both by changes in climate and by trends such as human population growth and migration, urbanisation, land use change, biodiversity loss and public health measures. Each of these may increase or decrease risk, interact with climate effects and may contribute to the emergence of infectious disease, although there are few studies assessing future risk of emergence (Gibb et al., 2020). Unless stated otherwise, the assessments below are specifically for the effects of climate change on individual diseases, assuming other determinants remain constant.
There is a high likelihood that climate change will contribute to increased distributional range and vectorial capacity of malaria vectors in parts of sub-Saharan Africa, Asia and South America (high confidence). In Nigeria, the range and abundance of Anopheles mosquitoes are projected to increase under both lower (RCP2.6) and especially under higher emissions scenarios (RCP8.5) due to increasing and fluctuating temperature, longer tropical rainfall seasons and rapid land use changes (Akpan et al., 2018). Similarly, vegetation acclimation due to elevated atmospheric CO2 under climate change will likely increase the abundance of Anopheles vectors in Kenya (Le et al., 2019). Distribution of Anopheles may decrease in parts of India and Southeast Asia, but there is an expected increase in vectorial capacity in China (Khormi and Kumar, 2016). In South America, climate change is projected to expand the distributions of malaria vectors to 35–46% of the continent by 2070, particularly species of the Albitarsis complex (Laporta et al., 2015).
Malaria infections have significant potential to increase in parts of sub-Saharan Africa and Asia, with risk varying according to the warming scenario (medium confidence). In Africa, where most malaria is due to the more deadly Plasmodium falciparum parasite, climate change is likely to increase the overall transmission risk due to the likely expansion of vector distribution and increase in biting rates (Bouma et al., 2016; M’Bra et al., 2018; Nkumama et al., 2017; Ryan et al., 2015b; Tompkins and Caporaso, 2016a). The projected effect of climate change varies markedly by region, with projections for west Africa tending to indicate a shortening of transmission seasons and neutral or small net reductions in overall risk, whereas studies consistently project increases in southern and eastern Africa, with potentially an additional 76 million people at risk of endemic exposure (10–12 months yr –1) by the 2080s (Nkumama et al., 2017; Ryan et al., 2015b; Semakula et al., 2017; Zaitchik, 2019; Leedale et al., 2016; Murdock et al., 2016; Yamana et al., 2016; Ryan et al., 2020). In sub-Saharan Africa, malaria case incidence associated with dams in malaria-endemic regions will likely be exacerbated by climate change, with significantly higher rates projected under RCP8.5 in comparison to lower-emission scenarios (Kibret et al., 2016). Incidence of malaria in Madagascar is projected to increase under RCP4.5 through RCP8.5 (Rakotoarison et al., 2018). Distribution of P. vivax and P. falciparum malaria in China is likely to increase under RCPs higher than 2.6, especially RCP8.5 (Hundessa et al., 2018). In India, projected scenarios for the 2030s under RCP4.5 indicate changes in the spatial distribution of malaria, with new foci and potential outbreaks in the Himalayan region, southern and eastern states, and an overall increase in months suitable for transmission overall, with some other areas experiencing a reduction in transmission months (Sarkar et al., 2019).
Rising temperatures are likely to cause poleward shifts and overall expansion in the distribution of mosquitoesAedes aegypti andAedes albopictus , the principal vectors of dengue, yellow fever, chikungunya and Zika (high confidence). Globally, the population exposed to disease transmission by one of these vectors is expected to increase significantly due to the combination of climate change and non-climatic processes including urbanisation and socioeconomic inter-connectivity, with exposure rates rising under higher warming scenarios (Kamal et al., 2018; Kraemer et al., 2019). For example, approximately 50% of the global population is projected to be exposed to these vectors by 2050 under RCP6.0 (Kraemer et al., 2019). The effect of climate change alone is projected to increase the population exposed to Aedes aegypti by 8–12% by 2061–2080 (Monaghan et al., 2018), and its abundance is projected to increase by 20% under RCP2.6 and 30% under RCP8.5 by the end of the century (Liu-Helmersson et al., 2019; Figure 7.10). Exposure to transmission by Aedes albopictus specifically would be highest at intermediate climate change scenarios and would decrease in the warmest scenarios (Ryan et al., 2019). Under scenarios other than RCP2.6, most of Europe would experience significant increases in exposure to viruses transmitted by both vectors (Liu-Helmersson et al., 2019).
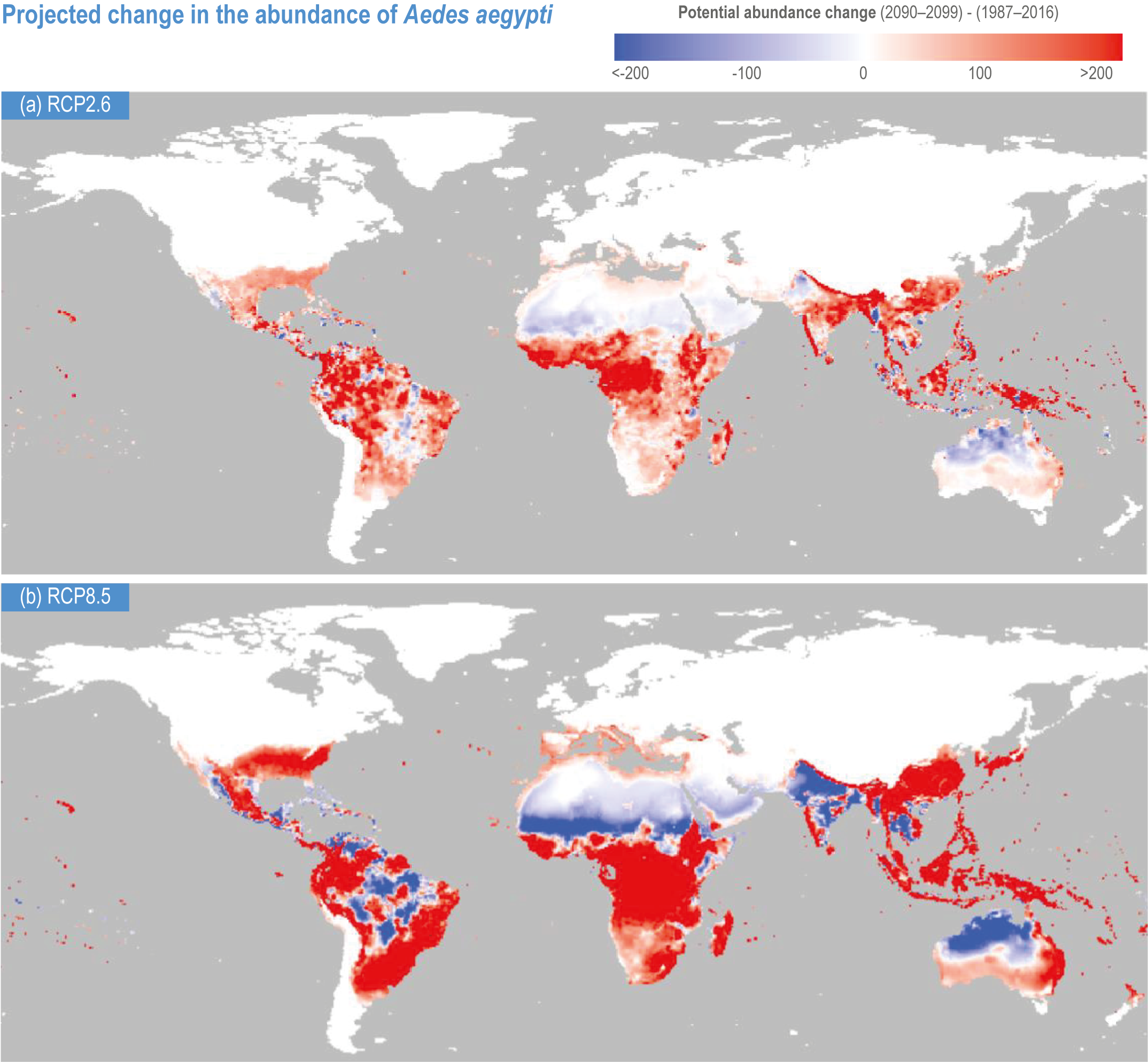
Figure 7.10 | Projected change in the potential abundance of Aedes aegyptiover the 21st century (2090–2099 relative to 1987–2016) (Liu-Helmersson et al. , 2019).
Climate change is expected to increase dengue risk and facilitate its global spread, with the risk being greatest under high emissions scenarios (high confidence). Future exposure to risk will be influenced by the combined effects of climate change and non-climatic factors such as population density and economic development (Akter et al., 2017). Overall, risk levels are expected to rise on all continents (Akter et al., 2017; Messina et al., 2015; Rogers, 2015; Liu-Helmersson et al., 2016; Messina et al., 2019). Compared to 2015, an additional 1 billion people are projected to be at risk of dengue exposure by 2080 under an SSP1-4.5 scenario, 2.25 billion under SSP2-6.0, and 5 billion under SSP3-8.5 (Messina et al., 2019). In North America, risk is projected to expand in north-central Mexico, with annual dengue incidence in Mexico increasing by up to 40% by 2080, and expand from US southern states to mid-western regions (Proestos et al., 2015; Colon-Gonzalez et al., 2013). In China, under RCP8.5, dengue exposure would increase from 168 million people in 142 counties to 490 million people in 456 counties by the late 2100s (Fan and Liu, 2019). In Nepal, dengue fever is expected to expand throughout the 2050s and 2070s under all RCPs (Acharya et al., 2018). In Tanzania, there is a projected shift in distribution towards central and northeastern areas and risk intensification in nearly all parts of the country by 2050 (Mweya et al., 2016). Dengue vectorial capacity is projected to increase in Korea under higher RCP scenarios (Lee et al., 2018a).
There are insufficient studies for assessment of projected effects of climate change on other arboviral diseases, such as chikungunya and Zika. Zika virus transmits under different temperature optimums than does dengue, suggesting environmental suitability for Zika transmission could expand with future warming (low confidence) (Tesla et al., 2018).
Climate change can be expected to continue to contribute to the geographical spread of the Lyme disease vectorIxodes scapularis (high confidence)and the spread of tick-borne encephalitis and Lyme disease vectorIxodes ricinus in Europe (medium confidence). In Canada, vector surveillance of the black-legged tick I. scapularis identified strong temperature effects on the limits of their occurrence, on recent geographic spread, temporal coincidence in emergence of tick populations and acceleration of the speed of spread (Clow et al., 2017; Cheng et al., 2017). In Europe, increasing temperatures over the 1950–2018 period significantly accelerated the life cycle of Ixodes ricinus and contributed to its spread (Estrada-Peña and Fernández-Ruiz, 2020). Under RCP4.5 and RCP8.5 scenarios, projections indicate a northward and eastward shift of the distribution of I. persulcatus and I. ricinus, vectors of Lyme disease and tick-borne encephalitis in northern Europe and Russia, with an overall large increase in distribution in the second half of the current century (Popov and Yasyukevich, 2014; Yasjukevich et al., 2018) and increases in intensity of tick-borne encephalitis transmission in central Europe (Nah et al., 2020).
Climate change is projected to increase the incidence of Lyme disease and tick-borne encephalitis in the Northern Hemisphere (high confidence) (Figure 7.9). The basic reproduction number (R0) of I. scapularis in at least some regions of Canada is projected to increase under all RCP scenarios (McPherson et al., 2017). In the USA, a 2°C warming could increase the number of Lyme disease cases by over 20% over the coming decades and lead to an earlier onset and longer length of the annual Lyme disease season (Dumic and Severnini, 2018; Monaghan et al., 2015).
Climate change is projected to change the distribution of schistosomiasis in Africa and Asia (high confidence), with a possible increase in global land area suitable for transmission (medium confidence). A global increase in land area with temperatures suitable for transmission by the three main species of Schistosoma (S. japonicum, S. mansoni and S. haematobium) is projected under the RCP4.5 scenario for the 2021–2050 and 2071–2100 periods (Yang and Bergquist, 2018), but regional outcomes are expected to vary. In Africa, shifting temperature regimes associated with climate change are expected to lead to reduced snail populations in areas with already high temperatures and higher populations in areas with currently low winter temperatures (Kalinda et al., 2017; McCreesh and Booth, 2014). Infection risk with Schistosoma mansoni may increase by up to 20% over most of eastern Africa over the next 20–50 years but decrease by more than 50% in parts of north and east Kenya, southern South Sudan and eastern People’s Democratic Republic of Congo (PDRC) (McCreesh et al., 2015), with a possible overall net contraction (Stensgaard et al., 2013). In China, currently endemic areas in Sichuan Province may become unsuitable for snail habitats, but currently non-endemic areas in Sichuan and Hunan/Hubei provinces may see a new emergence (Yang and Bergquist, 2018). In addition to the projected effects of temperature described above, distribution and transmission of schistosomiasis will also be affected positively or negatively by changes in the availability of freshwater bodies, which were not included in these models.
7.3.1.4 Projected Impacts on Waterborne Diseases
Climate change will contribute to additional deaths and mortality due to diarrhoeal diseases in the absence of adaptation (medium confidence) (see Figure 7.8). Risk factors for future excess deaths due to diarrhoeal diseases are highly mediated by future levels of socioeconomic development and adaptation. An additional 1°C increase in mean average temperature is expected to result in a 7% (95% CI, 3–10%) increase in all-cause diarrhoea (Carlton et al., 2016), an 8% (95% CI, 5–11%) increase in the incidence of diarrheic E. coli (Philipsborn et al., 2016) and a 3–11% increase in deaths attributable to diarrhoea (WHO, 2014). WHO Quantitative Risk Assessments for the effects of climate change on selected causes of death for the 2030s and 2050s project that overall deaths from diarrhoea should fall due to socioeconomic development but that the effect of climate change under higher emission scenarios could cause an additional 48,000 deaths in children aged under 15 years in 2030 and 33,000 deaths for 2050, particularly in Africa and parts of Asia. In Ecuador, projected increases in rainfall variability and heavy rainfall events may increase diarrhoea burden in urban regions (Deshpande et al., 2020). A limit in the assessable literature is a lack of studies in the highest risk areas (Liang and Gong, 2017; UNEP, 2018).
Climate change is expected to increase future health risks associated with a range of other WBDs and parasites, with effects varying by region (medium confidence). WBDs attributable to protozoan parasites including Cryptosporidium spp. and Giardia duodenalis (intestinalis) are expected to increase in Africa due to increasing temperatures and drought (Ahmed et al., 2018; Efstratiou et al., 2017). Recent data suggest a poleward expansion of Vibrios to areas with no previous incidence, particularly in mid- to high-latitude regions in areas where rapid warming is taking place (Baker-Austin et al., 2017). The number of Vibrio-induced diarrhoea cases yr –1 increased in past decades in the Baltic Sea region, and the projected risk of vibriosis will increase in northern areas, where waters are expected to become warmer and more saline due to reduced precipitation and have higher chlorophyll concentrations (Escobar et al., 2015; Semenza et al., 2017).
The risk of Campylobacteriosis and other enteric pathogens could rise in regions where heavy precipitation events or flooding are projected to increase (medium confidence). In Europe, the risk of Campylobacteriosis and diseases caused by other enteric pathogens could rise in regions where precipitation or extreme flooding are projected to increase (European Environment Agency, 2017), although incidence rates may be further mediated by seasonal social activities (Rushton et al., 2019; Williams et al., 2015b). Accelerated releases of dissolved organic matter to inland and coastal waters through increases in precipitation are expected to reduce the potential for solar ultraviolet inactivation of pathogens and increase risks for associated WBDs (Williamson et al., 2017). The combined relative risk for waterborne campylobacteriosis, salmonellosis and diseases due to Verotoxin-producing Escherichia coli was estimated to be 1.1 (i.e., a 10% increase) for every 1°C in mean annual temperature, while by the 2080s, under RCP8.5, annual rates of cryptosporidiosis and giardiasis could rise by approximately 16% due to more severe precipitation events (Brubacher et al., 2020; Chhetri et al., 2019).
7.3.1.5 Projected Impacts on Food-Borne Diseases
The prevalence of Salmonella infections is expected to rise as higher temperatures enable more rapid replication (medium confidence). Research from Canada finds a very strong association of salmonellosis and other FBDs with higher temperatures, suggesting that climate change could increase food safety risks ranging from increased public health burden to emergent risks not currently seen in the food chain (Smith and Fazil, 2019). In Europe, the average annual number of temperature-related cases of salmonellosis under high emissions scenarios could increase by up to 50% more than would be expected on the basis of on population change alone by 2100 (Lake, 2017; European Environment Agency, 2017). Warming trends in the southern USA may lead to increased rates of Salmonella infections (Akil et al., 2014).
7.3.1.6 Projected Impacts on Pollution- and Aeroallergens-Related Health Outcomes
Global air pollution-related mortality attributable directly to climate change—the human health climate penalty associated with climate-induced changes in air quality—is likely to increase and partially counteract any decreases in air pollution-related mortality achieved through ambitious emission reduction scenarios or stabilisation of global temperature change at 2°C (medium confidence). Demographic trends in aging and more vulnerable population are likely to be important determinants of future air quality—a human health climate penalty (high confidence).
Poor air quality contributes to a range of NCDs, including cardiovascular, respiratory and neurological, commonly resulting in hospitalisation or death. This section considers the possible risks for health of future climate-related changes in ozone and PM. The climate penalty, the degree to which global warming could affect future air quality, is better understood for ozone than for PM (von Schneidemesser et al., 2020). This is because increases in air temperature enhance ozone formation via associated photochemical processes (Archibald et al., 2020; Fu and Tian, 2019). The association between climate and PM is complex and moderated by a diverse range of PM components as well as formation and removal mechanisms (von Schneidemesser et al., 2020), added to which is uncertainty about future climate-related PM sources such as wildfires (Ford et al., 2018) and changes in aridity (Achakulwisut et al., 2019). As noted in AR6 WGI Chapter 6 (Naik et al 2021), future air quality will largely depend on precursor emissions, with climate change projected to have mixed effects. Because of the uncertainty in how natural processes will respond, there is low confidence in the projections of surface ozone and PM under climate change (Naik et al., 2021). This has implications on the levels of confidence in the projections of the health climate penalty associated with climate-induced changes in air quality (Orru et al., 2017; Orru et al., 2019; Silva et al., 2017).
There is a rich literature on global and regional level projections of air quality-related health effects arising from changes in emissions. Comparatively few studies assess how changes in air pollution directly attributable to climate change are likely to affect future mortality levels. Projections indicate that emission reduction scenarios consistent with stabilisation of global temperature change at 2°C or below would yield substantial co-benefits for air quality-related health outcomes (Chowdhury et al., 2018b; von Schneidemesser et al., 2020; Silva et al., 2016c; Markandya et al., 2018; Orru et al., 2019; Shindell et al., 2018) (high confidence). For example, by 2030, compared to 2000, it was estimated that globally and annually 289,000 PM2.5-related premature deaths could have been avoided under RCP4.5 compared to 17,200 PM2.5-related excess premature deaths under RCP8.5 (Silva et al., 2016c). Further, and notwithstanding estimated reductions in global PM2.5 levels and an associated increase in the number of avoidable deaths, the benefits of following a low emissions pathway are expected to be apparent by 2100, with avoidable deaths estimated at 2.39 million deaths yr –1 under RCP4.5. This contrasts with the 1.31 million deaths estimated under RCP8.5. A few projections of the health-related climate penalty indicate a possible increase in ozone and PM2.5-associated mortality under RCP8.5 (Doherty et al., 2017; Orru et al., 2019; Silva et al., 2017).
At the global level for PM2.5, annual premature deaths due to climate change were projected to be 55,600 (−34,300 to 164,000) and 215,000 (−76,100 to 595,000) in 2030 and 2100, respectively, countering by 16% the projected decline in PM2.5-related mortality between 2000 and 2100 without climate change (Silva et al., 2017). Similarly for ozone, the number of annual premature ozone-related deaths due to climate change was projected to be 3,340 in 2030 and 43,600 in 2050, with climate change accounting for 1.2% (14%) of the annual premature deaths in 2030 (2100) (Silva et al., 2017). These global level projections average over considerable geographical variations (Silva et al., 2017). Projections of the climate change effect on ozone mortality in 2100 were greatest for East Asia (41 deaths yr –1 per million people), India (8 deaths yr –1 per million people) and North America (13 deaths yr –1 per million people). For PM2.5, mortality was projected to increase across all regions except Africa (−25,200 deaths yr –1 per million people) by 2100, with estimated increases greatest for India (40 deaths yr –1 per million people), the Middle East (45 deaths yr –1 per million people), East Asia (43 deaths yr –1 per million people) and the Former Soviet Union (57 deaths yr –1 per million people). Overall, higher ozone-related health burdens were projected to occur in highly populated regions, and greater PM2.5 health burdens were projected in high PM emission regions (Doherty et al., 2017).
For central and southern Europe, climate change alone could result in an 11% increase in ozone-associated mortality by 2050. However, projected declines in ozone precursor emissions could reduce the EU-wide climate change effect on ozone-related mortality by up to 30%; the reduction was projected to be approximately 24% if aging and an increasingly susceptible population were accounted for in projections to 2050 (Orru et al., 2019). For the USA in 2069, the impact of climate change alone on annual PM2.5- and ozone-related deaths was estimated to be 13,000 and 3,000 deaths, respectively, with heat-driven adaptation of air conditioning accounting for 645 and 315 of the PM2.5- and ozone-related annual excess deaths, respectively (Abel et al., 2018). An aging population is a determinant of future air quality-related mortality levels. An aging population along with an increase in the number of vulnerable people may work to offset the decrease in deaths associated with a low emission pathway (RCP4.5) and possibly dominate the net increase in deaths under a business as usual pathway (RCP8.5) (Chen et al., 2020; Doherty et al., 2017; Hong et al., 2019; Schucht et al., 2015).
Complementing the longer-term changes in air quality arising from climate change are those associated with air pollution sensitive short-term meteorological events, such as heatwaves. Studies of individual heat events (Garrido-Perez et al., 2019; Johansson et al., 2020; Kalisa et al., 2018; Pu et al., 2017; Pyrgou et al., 2018; Schnell and Prather, 2017; Varotsos et al., 2019) and systematic reviews (Anenberg et al., 2020) provide evidence for synergistic effects of heat and air pollution. However, the health consequences of a possible additive effect of air pollutants during heatwave events were heterogeneous, varying by location and moderated by socioeconomic factors at the intra-urban scale (Analitis et al., 2014; Fenech et al., 2019; Krug et al., 2020; Pascal et al., 2021; Schwarz et al., 2021; Scortichini et al., 2018). This, combined with the challenges associated with projecting future concentrations of health-relevant pollutants during heatwave events (Jahn and Hertig, 2021; Meehl et al., 2018), makes it difficult to say with any certainty that synergistic effects of heat and poor air quality will result in a heatwave–air pollution health penalty under climate change.
The burden of disease associated with aeroallergens is anticipated to grow due to climate change (high confidence). The incidence of pollen allergy and associated allergic disease increases with pollen exposure, and the timing of the pollen season and pollen concentrations are expected to change under climate change (Beggs, 2021; Ziska et al., 2019; Ziska, 2020). The overall length of the pollen season and total seasonal pollen counts/concentrations for allergenic species such as birch (Betula) and ragweed (Ambrosia) are expected to increase as a result of CO2 fertilisation and warming, leading to greater sensitisation (Hamaoui-Laguel et al., 2015; Lake et al., 2017; Zhang et al., 2013). Changes in pollen levels for several species of trees and grasses are projected to increase annual emergency department visits in the USA by between 8% for RCP4.5 and 14% for RCP8.5 by the year 2090 (Neumann et al., 2019) with the exposure to some pollen types estimated to double beyond present levels in Europe by 2041–2060 (Lake et al., 2017). The prospect of increases in summer thunderstorm events under climate change (Brooks, 2013) may hold implications for changes in the occurrence of epidemic thunderstorm asthma (Bannister et al., 2021; Emmerson et al., 2021; Price et al., 2021). Similarly, projected alterations in hydroclimate under climate change may bear implications for increased exposure to mould allergens in some climates (D’Amato et al., 2020; Paudel et al., 2021).
7.3.1.7 Future Risks Related to Cardiovascular Diseases
Climate change is expected to increase heat-related CVD mortality by the end of the 21st century, particularly under higher emission scenarios (high confidence). Most modelling studies conducted since AR5 project higher rates of heat-related CVD mortality throughout the remainder of this century (Huang and et al., 2018; Li et al., 2015; Li et al., 2018; Limaye et al., 2018; Zhang et al., 2018a; Silveira et al., 2021a; Yang et al., 2021). CVD mortality in Beijing, China, could increase by an average of 18.4%, 47.8% and 69.0% in the 2020s, 2050s and 2080s, respectively, under RCP4.5 and by 16.6%, 73.8% and 134%, respectively, under RCP8.5 relative to a 1980s baseline (Li et al., 2015). Projections of temperature-related mortality from CVD for Beijing in the 2080s vary depending on RCP and population assumptions (Zhang et al., 2018a). Projections for Ningo, China, suggest heat-related years of life lost (YLL) could increase significantly in the month of August by between 3 and 11.5 times over current baselines by the 2070s, even with adaptation (Huang and et al., 2018). Yang and colleagues project that heat-related excess CVD mortality in China could increase to approximately 6% (from a 2010 baseline of under 2%) by the end of the century under RCP8.5 and to over 3% under RCP4.5 (Yang et al., 2021). The future burden of temperature-related myocardial infarctions in Germany is projected to rise under high emissions scenarios (Chen et al., 2019), while in the eastern USA, Limaye et al. (2018) projected an additional 11,562 annual deaths (95% CI: 2,641–20,095) by mid-century due to cardiovascular stress in the population 65 years of age and above. CVD mortality in Brazil is projected to increase up to 8.6% by the end of the century under RCP8.5, compared with an increase of 0.7% for RCP4.5 (Silveira et al., 2021a).
It is important to note that the assessed studies typically take an observed epidemiological relationship and apply future temperature projections (often derived from regional climate projections) to these relationships. Because the relationships between temperature and CVD deaths are influenced by both climatic and non-climatic factors (such as population fitness and aging), future projections are highly sensitive to assumptions about interactions between climate, population characteristics and adaptation pathways. Changes in air quality because of climate change are an additional important factor. For example, an assessment of future annual and seasonal excess mortality from short-term exposure to higher levels of ambient ozone in Chinese cities under RCP8.5 projected approximately 1,500 excess annual CVD deaths in 2050 (Chen et al., 2018). To the extent possible, the relationships reported above reflect changes derived from changes in heat exposure driven by climate change and not changes in population demographics or air pollution exposure.
Climate change could impact CVD through other pathways, including exposure to fine dust. For example, adult mortality attributable to fine dust exposure in the American southwest could increase by 750 deaths yr –1 (a 130% increase over baseline) by the end of the century under RCP8.5 (Achakulwisut et al., 2018).
7.3.1.8 Future Risks Related to Maternal, Foetal and Neonatal Health
Additional research is needed on future impacts of climate change on maternal, foetal and neonatal health . Maternal heat exposure is a risk factor for several adverse maternal, foetal and neonatal outcomes (Kuehn and McCormick, 2017), including foetal growth (Sun et al., 2019) and congenital anomalies (Haghighi et al., 2021). There is very limited research on this subject, an exception being Zhang et al. (2020), which projected a 34% increase in congenital health disease risk in the USA in 2025 and 2035 based on increased maternal extreme heat exposure.
7.3.1.9 Future Health Risks Related to Food, Diets and Nutrition
7.3.1.9.1 Malnutrition
Climate change is projected to exacerbate malnutrition (high confidence). Moderate and severe stunting in children less than five years of age was projected for 2030 across 44 countries to be an additional 570,000 cases under a prosperity and low climate change scenario (RCP2.6) to one million cases under a poverty and high climate change scenario (RCP8.5), with the highest effects in rural areas (Lloyd, 2018). Future DALYs lost due to protein-energy undernutrition and micronutrient deficiencies without climate change have been projected to increase between 2010 and 2050 by over 30 million; with climate change (RCP8.5), DALYs were projected to increase by nearly 10%, with the largest increases in Africa and Asia (Sulser et al., 2021).
The projected risks of hunger and childhood underweight vary under the five SSPs, with population growth, improvement in the equality of food distribution and income-related increases in food consumption influencing future risks (Ishida et al., 2014; Hasegawa et al., 2015). A review of 57 studies projecting global food security to 2050 under the SSPs concluded that global food demand was expected to increase by 35–56% between 2010 and 2050 (van Dijk et al., 2021). In the same review, estimates of the change in population at risk of hunger by 2050 range between −91 to +8% if climate change is not considered and between -91 to +30% if climate change is considered, with the inclusion of climate change not leading to statistically significant differences in projections (van Dijk et al., 2021).
7.3.1.9.2 Climate Change, Carbon Dioxide, Diets and Health
Climate change could further limit equitable access to affordable, culturally acceptable, and healthy diets (high confidence). Climate impacts on agricultural production and regional food availability will affect the composition of diets, which can have major consequences for health. Variable by region and context, healthy diets are an outcome of the four inter-connected domains of sustainable food systems, namely ecosystems, society, economics and health (Drewnowski et al., 2020; Fanzo et al., 2020). Climate change limits the potential for healthy diets through adverse impacts on natural and human systems that are disproportionately experienced by low-income countries and communities (FAO et al., 2021). Climate-driven droughts, floods, storms, wildfires and extreme temperatures reduce food production potential by diminishing soil health, water security and biological and genetic diversity (Macdiarmid and Whybrow, 2019). Models project that climate-related reductions in food availability, specifically fruit and vegetables, could result in an additional 529,000 deaths a year by 2050 (Springmann et al., 2016b).
Diets reliant on marine fisheries and fish also face complex climate-driven challenges (Hollowed et al., 2013). Rapidly warming oceans (Cheng et al., 2020) limit the size of many fish and hamper their ability to relocate or adapt; many commonly consumed fish, like sardines, pilchards and herring, could face extinction due to these pressures (Avaria-Llautureo et al., 2021). Other fisheries models project end-of-century pollock and Pacific cod fisheries decreasing by > 70% and > 35% under RCP8.5 (Holsman et al., 2020). Climate-driven increases in marine mercury concentrations (Booth and Zeller, 2005) and harmful algal blooms (Jardine et al., 2020) could impact dietary quality and human health.
Global crop and economic models project higher cereal prices of up to 29% by 2050 under RCP6.0, resulting in an additional 183 million people in low-income households at risk of hunger (Hasegawa et al., 2018). Climate impacts on human health disrupt agricultural labour, food supply chain workers and ultimately regional food availability and affordability. A recent meta-analysis focused on sub-Saharan Africa and Southeast Asia combined metrics of heat stress and labour to project that a 3°C increase in global mean temperature, without adaptation or mechanisation, could reduce agricultural labour capacity by 30–50%, leading to 5% higher crop prices and a global welfare loss of USD 136 billion (de Lima et al., 2021).
The nutritional density, including protein content, micronutrients and B-vitamins, of wheat, rice, barley and other important food crops is negatively affected by higher CO2concentrations (very high confidence) (Mbow, 2019 ; Smith and Myers, 2018). Projections indicate negative impacts on human nutrition by rising CO2 concentrations by mid- to late-century (Medek et al., 2017; Smith and Myers, 2018; Weyant et al., 2018; Zhu et al., 2018; Beach et al., 2019). Staple crops are projected to have protein and mineral concentrations decreased by 5–15% and B vitamins up to 30% when the concentrations of CO2 double above pre-industrial levels (Ebi and Loladze, 2019; Beach et al., 2019; Smith and Myers, 2018). Without changes in diets and accounting for nutrient declines in staple crops, a projected additional 175 million people could be zinc deficient and an additional 122 million people could become protein deficient (Smith and Myers, 2018). Weyant et al. (2018) projected that CO2-related reductions in crop zinc and iron levels could result in 125.8 million DALYs lost globally, with Southeast Asian and sub-Saharan African countries most affected. Zhu et al. (2018) estimated 600 million people at risk from reductions in the protein, micronutrient and B-vitamin content of widely grown rice cultivars in Southeast Asia.
The combined effect of CO2 and rising temperatures because of climate change could result in a 2.4–4.3% penalty on expected gains by mid-century in nutritional content because of technology change, market responses and the fertilisation effects of CO2 on yield (Beach et al., 2019). These penalties are expected to slow progress in achieving reductions in global nutrient deficiencies, disproportionately affecting countries with high levels of such deficiencies.
7.3.1.10 Projected Impacts on Harmful Algal Blooms, Mycotoxins, Aflatoxins and Chemical Contaminants
Harmful algal blooms are projected to increase globally, thus increasing the risk of seafood contamination with marine toxins (high confidence) (European Food Safety Authority et al., 2020; Gobler et al., 2017; Barange et al., 2018; IPCC, 2019b; Wells et al., 2020). Climate change impacts on oceans could generate increased risks of ciguatera poisoning in some regions (medium confidence). Studies suggest that rising sea surface temperatures could increase rates of ciguatera poisoning in Spain (Botana, 2016) and other parts of Europe (European Food Safety Authority et al., 2020).
Mycotoxins and aflatoxins may become more prevalent due to climate change (medium agreement, low evidence). Models of aflatoxin occurrence in maize under climate change scenarios of +2°C and +5°C in Europe over the next 100 years project that aflatoxin B1 may become a major food safety issue in maize, especially in Eastern Europe, the Balkan Peninsula and the Mediterranean regions (Battilani, 2016). The occurrence of toxin-producing fungal phytopathogens has the potential to increase and expand from tropical and subtropical regions into regions where such contamination does not currently occur (Battilani, 2016).
Climate change may alter regional and local exposures to anthropogenic chemical contaminants (medium agreement, low evidence). Changes in future occurrences of wildfires could lead to a 14% increase in global emissions of mercury by 2050, depending on the scenarios used (Kumar et al., 2018a). Mercury exposure via consumption of fish may be affected by warming waters. Warming trends in the Gulf of Maine could increase the methyl mercury levels in resident tuna by 30% between 2015 and 2030 (Schartup et al., 2019). An observed annual 3.5% increase in mercury levels was attributed to fish having higher metabolism in warmer waters, leading them to consume more prey. The combined impacts of climate change and the presence of arsenic in paddy fields are projected to potentially double the toxic heavy metal content of rice in some regions, potentially leading to a 39% reduction in overall production by 2100 under some models (Muehe et al., 2019).
7.3.1.11 Future Risks Related to Mental Health and Well-Being
Climate change is expected to have adverse impacts on well-being, some of which will become serious enough to threaten mental health (very high confidence). However, changes (Hayes and Poland, 2018) in extreme events due to climate change, including floods (Baryshnikova, 2019), droughts (Carleton, 2017) and hurricanes (Kessler et al., 2008; Boscarino et al., 2013, Boscarino et al., 2017; Obradovich et al., 2018), which are projected to increase due to climate change, directly worsen mental health and well-being and increase anxiety (high confidence). Projections suggest that sub-Saharan African children and adolescents, particularly girls, are extremely vulnerable to negative direct and indirect impacts on their mental health and well-being (Atkinson and Bruce, 2015; Owen et al., 2016). The direct risks are greatest for people with existing mental disorders, physical injuries, and compromised respiratory, cardiovascular and reproductive systems, with indirect impacts potentially arising from displacement, migration, famine and malnutrition, degradation or destruction of health and social care systems, conflict, and climate-related economic and social losses (high to very high confidence) (Burke et al., 2018; Curtis et al., 2017; Hayes et al., 2018; Serdeczny et al., 2017; Watts et al., 2019). Demographic factors increasing vulnerability include age, gender and low socioeconomic status, though the effect of these will vary depending on the specific manifestation of climate change; overall, climate change is predicted to increase inequality in mental health across the globe (Cianconi et al., 2020). Based on evidence assessed in Section 7.2, future direct impacts of increased heat risks and associated illnesses can be expected to have negative implications for mental health and well-being, with outcomes being highly mediated by adaptation, but there are no assessable studies that quantify such risks. There may be some benefits to mental health and well-being associated with fewer very cold days in the winter; however, research is inconsistent. Any positive effect associated with reduced low-temperature days is projected to be outweighed by the negative effects of increased high temperatures (Cianconi et al., 2020).
Human behaviours and systems will be disrupted by climate change in a myriad of ways, and the potential consequences for mental health and well-being are correspondingly large in number and complex in mechanism (high confidence). For example, climate change may alter human physical activity and mobility patterns, in turn producing alterations in the mental health statuses promoted by regular physical activity (Obradovich and Fowler, 2017; Obradovich and Rahwan, 2019). Climate change may affect labour capacity, because heat can compromise the ability to engage in manual labour as well as cognitive functioning, with impacts on the economic status of individual households as well as societies (Kjellstrom et al., 2016; Liu, 2020). Migrations and displacement caused by climate change may worsen the well-being of those affected (Vins et al., 2015; Missirian and Schlenker, 2017). Climate change is expected to increase aggression through both direct and indirect mechanisms, with one study predicting a 6% increase in homicides globally for a 1°C temperature increase, although noting significant variability across countries (Mares and Moffett, 2016). Broad societal outcomes such as economic unrest, political conflict or governmental dysfunction assessed in Section 7.3.5 may undermine the mental health of populations in the future (medium confidence). Food insecurity presents its own severe risks for mental health and cognitive function (Jones, 2017).
7.3.2 Migration and Displacement in a Changing Climate
Future changes in climate-related migration and displacement are expected to vary by region and over time according to: (a) region-specific changes in climatic drivers, (b) changes in the future adaptive capacity of exposed populations, (c) population growth in areas most exposed to climatic risks and (d) future changes in mediating factors such as international development and migration policies (high agreement, medium evidence) (Gemenne and Blocher, 2017; Cattaneo et al., 2019; McLeman, 2019). This section assesses future risks associated with changes in the frequency and/or severity of storms, floods, droughts, extreme heat, wildfires and other events assessed in Section 7.2 that currently affect migration and displacement patterns, as well as the impacts of emerging hazards, including average temperature increases that may affect the habitability of settlements in arid regions and the tropics, and sea level rise and associated hazards that threaten low-lying coastal settlements. Studies assessed here consider projected changes in future exposure to hazards over a variety of geographical and temporal periods, with some considering changes in population numbers in exposed areas. The uneven distribution of exposure of age cohorts is typically overlooked in existing research. For example, people younger than age 10 in the year 2020 are projected to experience a nearly four-fold increase in extreme events under 1.5°C of global warming and a five-fold increase under 3°C warming; such increases in exposure would not be experienced by a person of the age of 55 in 2020 in their remaining lifetime under any warming scenario (Thiery et al., 2021).
7.3.2.1 Region-Specific Changes in Climatic Risks
As outlined in 7.2, the most common drivers of observed climate-related migration and displacement are extreme storms (particularly tropical cyclones), floods and droughts (high confidence). The future frequency and/or severity of such events due to anthropogenic climate change are expected to vary by region according to future GHG emission pathways (Naik et al 2021; Regional Chapters, this report), with there being an increased potential for compound effects of successive or multiple hazards (e.g., tropical storms accompanied by extreme heat events (Matthews et al., 2019)). Table 7.2 summarises anticipated changes in future migration and displacement risks due to sudden-onset climate events by region (and by sub-regions for Africa and Asia, where climatic risks vary within the region).
Table 7.2 | Projected changes in sudden-onset climate events associated with migration and displacement by region.
Region | Main directions of current migration flows (from Abel and Sander (2014)) | Current climatic drivers of migration and displacement (Section 7.2.6.1) | Expected changes in drivers (including confidence statements) from IPCC WGI 2021 Technical Summary, 4.3.1–4.3.2 |
Asia |
| Floods, extreme storms, extreme heat | Increased risk of flooding in East, north, south and Southeast Asia due to increases in annual mean precipitation (high confidence) and extreme precipitation events in East, south, west central, north and Southeast Asia (medium confidence); uncertainty regarding future trends in cyclones (current trend = decreased frequency, increased intensity); higher average temperatures across region (high confidence) |
Africa |
| Floods, droughts, extreme heat | Decrease in total annual precipitation in northernmost and southernmost parts of Africa (high confidence); west-to-east pattern of decreasing-to-increasing annual precipitation in west Africa and east Africa (medium confidence); increased risk of heavy precipitation events that trigger flooding, across most parts of Africa (medium confidence); increased aridity and drought risks in north Africa, southern Africa and western parts of west Africa (medium-high confidence) |
Europe |
| Floods | Increased risk of floods across all areas of Europe except Mediterranean areas (high confidence); higher risks of drought and fire weather in Mediterranean areas (high confidence) |
North America |
| Floods, tropical cyclones (US Atlantic and Caribbean coast), tornadoes, wildfires | Increased frequency of heavy precipitation events across most areas (high confidence); tropical cyclones to become more severe (medium confidence); increased risk of drought and fire weather in central and western North America |
Central and South America |
| Floods (Central and South America), extreme storms (Central America) | Increases in mean annual precipitation and extreme precipitation events with higher risks of floods in most areas of South America (medium confidence); increased risk of droughts in northeastern and southern South America and northern Central America (medium confidence); tropical cyclones becoming more extreme (medium confidence) |
Australasia |
| Wildfires | Increases in fire weather across Australia and New Zealand (medium confidence) |
Small island states |
| Extreme storms | Potentially fewer but more extreme tropical cyclones (medium confidence) |
In low-lying coastal areas of most regions, future increases in mean sea levels will amplify the impacts of coastal hazards on settlements, including erosion, inland penetration of storm surges and groundwater contamination by salt water, and eventually lead to inundation of very low-lying coastal settlements (high confidence) (Diaz, 2016; Hauer et al., 2016; Neumann et al., 2015; Rahman et al., 2019; IPCC, 2019a). Projections of the number of people at risk of future displacement by sea level rise range from tens of millions to hundreds of millions by the end of this century, depending on (a) the sea level rise scenario or RCP selected, (b) projections of future population growth in exposed areas and (c) the criteria used for identifying exposure. These latter measures can include estimates of populations situated within selected elevations above sea level (with 1 m, 2 m and 10 m being common parameters), populations situated in 1-in-100 year floodplains or populations in areas likely to be entirely inundated under specific RCPs (Neumann et al., 2015; Hauer et al., 2016; Merkens et al., 2018; McMichael et al., 2020; Hooijer and Vernimmen, 2021). As an illustrative example, an estimated 267 million people (error range = 197–347 million at 68% confidence level) worldwide lived within 2 m of sea level in 2020, 59% of whom reside in tropical regions of Asia (Hooijer and Vernimmen, 2021). At a 1 m increase in sea level and holding coastal population numbers constant, the number of people worldwide living within 2 m of sea level expands to 410 million (error range = 341–473 million). However, it is unlikely that coastal population growth rates will remain constant at global or regional scales in future decades. At present, coastal cities in many regions have relatively high rates of population growth due to the combined effects of in-migration from other regions and natural increase, with coastal areas of Africa having the highest projected future population growth rates (Neumann et al., 2015; Hooijer and Vernimmen, 2021; Box 7.5). Further complicating future estimates is that many large coastal cities are situated in deltas with high rates of subsidence, meaning that locally experienced changes in relative sea level may be much greater than sea level rise attributable to climate change, thereby further increasing the number of people exposed (Edmonds et al., 2020; Nicholls et al., 2021).
Sea level rise is not presently a significant driver of migration in comparison with hazards assessed in Section 7.2.6, but it has been attributed as a factor necessitating the near-term resettlement of small coastal settlements in Alaska, Louisiana, Fiji, Tuvalu and the Carteret Islands of Papua New Guinea (Marino and Lazrus, 2015; Connell, 2016; Hamilton et al., 2016; Nichols, 2019). In coastal Louisiana, communities tend to resist leaving exposed settlements until approximately 50% of available land has been lost (Hauer et al., 2019). Movements away from highly exposed areas may have longer-term demographic implications for inland settlements (Hauer, 2017), but this requires further study. Based on the available empirical evidence, sea level rise does not appear to currently be a primary motivation for international migration originating in small island states in the Indian and Pacific Oceans; rather, economic considerations and family reunification appear to be the dominant drivers (McCubbin et al., 2015; Stojanov and Du, 2016; Heslin, 2019; Kelman et al., 2019). However, climatic drivers of migration are anticipated to take on a much greater causal role in migration decisions in coming decades (Thomas et al., 2020) and may discourage return migration to small island states (van der Geest et al., 2020). Even under best-case sustainable development scenarios, rising sea levels and associated hazards create risks of involuntary displacement in low-lying coastal areas and should be expected to generate a need for organised relocation of populations where protective infrastructure cannot be constructed (Horton and de Sherbinin, 2021; Hamilton et al., 2016). In high emissions scenarios, low-lying island states may face the long-term risk of becoming uninhabitable, creating the potential for a new phenomenon of climate-induced statelessness (Piguet, 2019; Desai et al., 2021).
Increased frequency of extreme heat events and long-term increases in average temperatures pose future risks to the habitability of settlements in tropical and subtropical regions, and may in the long term affect migration patterns in exposed areas, especially under high emissions scenarios (medium agreement, low evidence). Greater research into the specific dynamics between extreme heat and population movements is required in order to make an accurate assessment of this risk. Recent studies suggest that future increases in average temperatures could expose populations across wide areas of the tropics and subtropics to ambient temperatures for extended periods each year that are beyond the threshold for human habitability (Pal and Eltahir, 2016; Im et al., 2017; Xu et al., 2020). This effect would be amplified in urban settings where heat-island effects occur and create a heightened need for air conditioning and other adaptation measures. In addition to risks associated with average temperature changes, Dosio et al. (2018) project that at 1.5°C warming, between 9% and 18% of the global population will be regularly exposed to extreme heat events at least once in five years, with the exposure rate nearly tripling with 2°C warming. How these changes in exposure to high temperatures will affect future migration patterns, particularly among vulnerable groups, will depend heavily on future adaptation responses (Horton and de Sherbinin, 2021). Multiple country-level studies assessed in Section 7.2 observe existing associations between extreme heat, its impacts on agricultural livelihoods and changes in rural-to-urban migration flows in parts of south Asia and sub-Saharan Africa. A study conducted in Indonesia, Malaysia and the Philippines suggests that an increased risk of heat stress would likely influence migration intentions of significant numbers of people (Zander et al., 2019).
7.3.2.2 Interactions with Non-climatic Determinants and Projections of Future Migration Flows
Only a very small number of studies have attempted to make systematic projections of future regional or global migration and displacement numbers under climate change. Key methodological challenges for making such projections include the availability of reliable data on migration within and between countries, definitional ambiguity in distinguishing climate-related migration from migration undertaken for other reasons, and accounting for the future influence of non-climatic factors. The most reliable example of such studies to date is a World Bank report by Rigaud et al. (2018) that generated projections of future internal population displacements in south Asia, sub-Saharan Africa and Latin America by 2050 using multiple climate and development scenarios, resulting in a very large range of possible outcomes (from 31 to 143 million people being displaced, depending on assumptions). An important outcome is the study’s emphasis on how the potential for future migration and displacement will be strongly mediated by socioeconomic development pathways in low- and middle-income countries. Hoffmann et al. (2020) used meta-regression-based analyses to project that future environmental influences on migration are likely to be greatest in low- and middle-income countries in Latin America and the Caribbean, sub-Saharan Africa, the Middle East and most of continental Asia.
Research reviewed in AR4 and AR5 observed that at higher rates of socioeconomic development, the in situ adaptive capacity of households and institutions rises, and climatic influences on migration correspondingly decline. Recent evidence adds further support for such conclusions (high confidence) (Kumar et al., 2018b; Mallick, 2019; Gray et al., 2020; Box 7.5). Population growth rates are currently highest in low-income countries (UN DESA Population Division, 2019), many of which have high rates of exposure to climatic hazards associated with population displacement, further emphasising the importance of socioeconomic development and adaptive capacity-building. Although country-specific scenarios for socioeconomic development and population are embedded in SSPs, research into future migration flows under climate change has not made great use of these. One of the few studies to do so found that safe and orderly international migration tends to increase wealth at regional and global scales in all SSP narratives, which in turn reduces income inequality between countries (Benveniste et al., 2021). International barriers to safe and orderly migration may potentially impede progress towards attainment of the objectives described in the SDGs and increase exposure to climatic hazards in low- and middle-income countries (McLeman, 2019; Benveniste et al., 2020).
Box 7.5 | Uncertainties in projections of future demographic patterns at global, regional and national scales
Projections of future numbers of people exposed to climate change-related hazards described in this chapter and elsewhere in this report are heavily influenced by assumptions about population change over time at global, regional and national scales. One challenge concerns global and regional variability of baseline data for current populations, which is typically aggregated from national censuses that vary considerably in terms of frequency, timing and reliability, especially in low-income countries. A number of gridded mapping dataset initiatives emerged in recent years to support population–environment modelling research at global and regional levels, common ones being the Gridded Population of the World, the Global Rural Urban Mapping Project, and LandScan Global Population dataset (McMichael et al., 2020). For future population projections at national levels, researchers commonly draw upon data generated by the Population Division of the United Nations Department of Economic and Social Affairs, which publishes periodic projections for future fertility, mortality, and international migration rates for over 200 countries, the most recent projections being for the 2020 to 2100 period (UN DESA Population Division, 2019). There have been debates among demographers regarding the precision of DESA projections, and whether these overestimate or underestimate future population growth in some regions (Ezeh et al., 2020). Population growth rates are highly influenced by socioeconomic conditions, meaning that future population levels at local, national and regional scales are likely to respond to relative rates of progress towards meeting the Sustainable Development Goals (Abel et al., 2016). The Shared Socioeconomic Pathways (SSPs) used in climate impacts and adaptation research include a variety of assumptions about future mortality, fertility and migration rates and provide a range of population growth scenarios that diverge after the year 2030 according to future development trajectories (Samir and Lutz, 2017) and are then further modified and downscaled by researchers for national-level studies. Understanding future risks of climate change will benefit from continued efforts by the international community to collect and share data on observed population numbers and trends, and to work towards better projected data for population characteristics that strongly influence vulnerability to climate risks, such as gender, age and indigeneity.
7.3.3 Climate Change and Future Risks of Conflict
Climate change may increase susceptibility to violent conflict, primarily intra-state conflicts, by strengthening climate-sensitive drivers of conflict (medium confidence). Section 7.2.7 described how climate variability and extremes affect violent conflict through food and water insecurity, loss of income and loss of livelihoods. Risks are amplified by insecure land tenure, competing land uses and weather-sensitive economic activities when they occur in the context of weak institutions and poor governance, poverty and inequality (Section 7.2.7). These known, climate-sensitive risk factors allow projections of where conflict is more likely to arise or worsen under climate change impacts (see Chapters 1, 4, 5, 6 and 16) (Mach et al., 2020). However, there is also the potential for new causal pathways to emerge as climate changes beyond the variability observed in available datasets and adaptation limits are met (Theisen, 2017; Mach et al., 2019; von Uexkull and Buhaug, 2021).
Future violent conflict risk is highly mediated by socioeconomic development trajectories (high confidence). Development trajectories that prioritise economic growth, political rights and sustainability are associated with lower conflict risk (medium confidence, low evidence). Hegre et al. (2016) forecast future conflict under the SSPs and found that SSP1, which prioritises sustainable development, is associated with lower risks of conflict. Using data from sub-Saharan Africa, Witmer et al. (2017) forecast conflict along the SSPs and find that any increases in conflict that may be associated with climate change could be offset by increases in political rights. Strong predictors of future conflict are a recent history of conflict, large populations and low levels of socioeconomic development (Hegre and Sambanis, 2006; Blattman and Miguel, 2010).
Increases in conflict-related deaths with climate change have been estimated but results are inconclusive (high agreement, medium evidence). Some studies attempted to attribute observed conflict outbreaks to changes in the physical environment and quantify future conflict risk associated with climate change (von Uexkull and Buhaug, 2021; Theisen, 2017). Burke et al. (2015b) concluded that with each one standard deviation increase in temperature, inter-personal conflict increased by 2.4% and inter-group conflict by 11.3%. However, the statistical methods have been criticised for under-representing the known role that socioeconomic conditions and conflict history play in determining the prevalence of violence (Buhaug et al., 2014; van Weezel, 2019; Abel et al., 2019). Forecasting armed conflict is used as a heuristic policy tool rather than a representation of the future (Cederman and Weidmann, 2017) and forecasts have limitations. For example, what constitutes and is experienced as hazards and as drivers of conflict will shift over time as societies adapt to climate change (Roche et al., 2020). The SSPs assume economic convergence between countries and do not reflect growth disruptions (e.g., commodity price shocks) that are often a key conflict risk factor (Dellink et al., 2017; Buhaug and Vestby, 2019 ; Hegre et al., 2021).
Asia represents a key region where the peace, vulnerability and development nexus has been analysed. In central, south and Southeast Asia, there are large numbers of people exposed to changing climate (Busby et al., 2018; Vinke et al., 2017; Reyer et al., 2017). South Asia is one of the less peaceful regions in the world due to intra-state communal conflict, international military conflict and political tension (Wischnath and Buhaug, 2014; Huda, 2021), and many of the factors that drive conflict risk (e.g. large populations with high levels of inequality) are present (Nordqvist and Krampe, 2018). Despite these risks, studies in this region also support the case for environmental peacebuilding and resource sharing, as it relates to transboundary water sharing (Berndtsson and Tussupova, 2020; Huda and Ali, 2018; Section 4.3.6; Section 7.4.5.2).
There is little evidence of weather-related impacts on conflict risk or prevalence, but the region is under-studied in general (Wischnath and Buhaug, 2014; Nordqvist and Krampe, 2018). Climate stressors may have contributed in part to local-level conflicts in Bangladesh and Nepal (Sultana et al., 2019) and intensified water use conflict in peri-urban areas (Roth et al., 2019). In the future there is the potential for climate change to stretch the effectiveness of transboundary water agreements by raising regional geopolitical tensions (Atef et al., 2019; Scott et al., 2019) or to generate water use conflicts between hydropower and irrigation within countries (Jalilov et al., 2018). Climate change may have an impact on conflict by affecting food security (Caruso et al., 2016; Raghavan et al., 2019). There may be greater military involvement in humanitarian response to cyclones, flooding and to other impacts of climate change that might contribute to increased instability (Pai, 2008; Busby and Krishnan, 2017).
7.4 Adaptation to Key Risks and Climate Resilient Development Pathways
With proactive, timely and effective adaptation, many observed and projected risks for human health and well-being, health systems and those associated with migration and conflict can be reduced or potentially avoided (high confidence). Given the key health risks identified in this chapter, adaptation that increases resilience and sustainability will require moving beyond incremental adaptation to sustained, adaptive management (Ebi, 2011; Hess et al., 2012) with the goal of transformative change for integrated protection of human, animal and ecosystem health. This includes differentiating adaptation to climate variability from adaptation to climate change (Ebi and Hess, 2020). Health adaptation efforts are increasingly aiming to transition to building climate-resilient and environmentally sustainable health systems (WHO, 2015b; WHO, 2020a) and healthcare facilities, emphasising service delivery including climate-informed health policies and programmes; management of the environmental determinants of health; emergency preparedness and management; health information systems such as health and climate research, integrated risk monitoring and early warning systems; and vulnerability, capacity and adaptation assessments (Marinucci et al., 2014; Mousavi et al., 2020; WHO 2015a; Centres for Disease Control , 2019; WHO, 2020a).
Migration can contribute to or work against adaptation goals and progress, depending on the circumstances under which it occurs. Policies that support safe and orderly movements of people, protect migrant rights, and facilitate flows of financial and other resources between sending and receiving communities are consistent with adaptive capacity-building and building sustainability and are part of CRDPs (section 7.4.4).
Adaptation to prevent climate change from exacerbating conflict risk involves meeting development objectives encapsulated in the SDGs. Conflict-sensitive adaptation and climate-sensitive peacebuilding offer promising avenues to addressing conflict risk, but their efficacy is yet to be demonstrated through effective monitoring and evaluation (Gilmore et al., 2018). Associations between environmental factors and conflict are weak in comparison to socioeconomic and political drivers. Therefore, meeting the SDGs, including Goal 16 on peace, justice and strong institutions represent unambiguous pathways to reducing conflict risk under climate change (Singh and Chudasama, 2021). Actively pursuing peace rather than taking conflict for granted (Barnett, 2019), improving focus on gender within peacebuilding (Dunn and Matthew, 2015; UNEP, 2021) and understanding how natural resources and their governance interact with peacebuilding (Krampe et al., 2021) present key elements of CRDPs for sustainable peace.
As documented across this chapter, there is a large adaptation deficit for health and well-being, with climate change causing avoidable injuries, illnesses, disabilities, diseases and deaths (high confidence). Implementation of health adaptation has been incremental because of significant constraints, primarily relating to financial and human resources and because of limited research funding on adaptation (Berrang-Ford et al., 2021). Current global investments in health adaptation are insufficient to protect the health of populations and communities (high confidence) from most climate-sensitive risks, with large variability across and within countries and regions (UNEP, 2018). Climate change adaptation in health is < 1% of international climate finance despite health being a priority sector in 54% of NDCs featuring adaptation (UNEP, 2018).
As climate change progresses and the likelihood of dangerous risks to human health continue to increase, there will be greater pressure for more transformational changes to health systems to reduce future vulnerabilities and limit further dangerous climate change (Ebi et al., 2021a). Transformational resilience would need parallel investments in social and health protections, including achieving the SDGs, coupled with investments in mitigation (Ebi and Hess, 2020). Further, investments in mitigating GHG emissions will not only reduce risks associated with dangerous climate change but will improve population health and well-being through several salutary pathways.
This chapter section identifies and assesses specific elements in adapting to the risks identified in 7.2 and 7.3 and the opportunities for fostering sustainability and pursuing CRDPs.
7.4.1 Adaptation Solution Space for Health and Well-Being
The solution space is the space within which opportunities and constraints determine why, how, when and who adapts to climate change (Chapter 1). There is increased understanding of exposure and vulnerabilities to climate variability and change, the capacities to manage the health risks, the effectiveness of adaptation (including a growing number of lessons learned and best practices), and the co-benefits of mitigation policies and technologies (high confidence).
Effectively preparing for and managing the health risks of climate change requires considering the multiple interacting sectors that affect population health and the effective functioning of health systems (high confidence). Given the wide range of causal pathways through which climate change affects environmental and social systems resulting in health impacts, a systems-based approach can promote identifying, implementing and evaluating solutions that support population health and health systems in the short and longer term (high agreement, medium evidence). Such an approach provides insights into policies and programmes that promote health and well-being via multiple sectors (e.g., water and food safety and security) and can ensure that health policies do not have adverse consequences in other sectors (WHO, 2015b; Ebi and Otmani del Barrio, 2017; Wright et al., 2021).
Figure 7.11 illustrates the context within which risks to health outcomes and health systems emerge because of climate change. The figure presents the emergence of risk from interactions between specific types of climatic hazards, the exposure and vulnerability to those hazards, and the responses taken within the health sector. The figure also illustrates how health risks are situated within larger interactions between the health system and other sectors and systems, with underlying enabling conditions making adaptation and transformation possible. Within this context, response options can decrease the impacts of climate change on human health, well-being and health systems by (a) reducing exposure to climate-related hazards; (b) reducing vulnerability to such hazards and (c) strengthening health system responses to future risks. Such approaches are described as ‘Lateral Public Health’ and emphasise the importance of involving community members and stakeholders in the planning and coordination of activities (Semenza, 2021; Semenza, 2011). Lateral public health strives for community engagement (e.g., through access to technology in decision-making, such as low-cost air sensors for wildfire smoke) in preparedness and response.
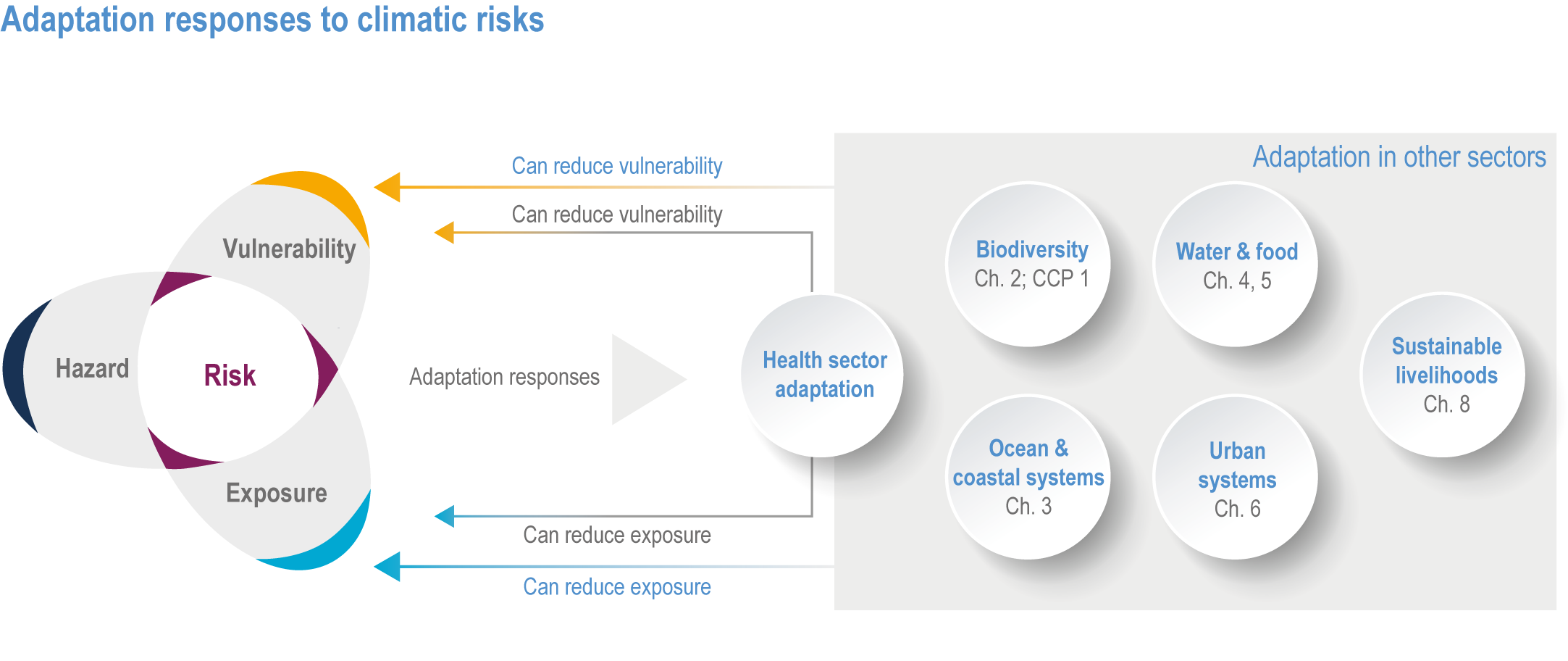
Figure 7.11 | Context within which adaptation responses to climatic risks to health are implemented in the frame of interactions between health and multiple other sectors.
Effective health risk management incorporates the magnitude and pattern of future climate risks as well as potential changes in factors that determine vulnerability and exposure to climate hazards, such as determinants of healthcare access, demographic shifts, urbanisation patterns and changes in ecosystems (very high confidence). Climate change is associated with shocks and stresses that can affect the capacity and resilience of health systems and healthcare facilities (WHO, 2020a). Figure 7.12 illustrates some possible extents to which the capacity of health systems could be reduced when exposed to a stress or shock, and possible pathways forward, from collapse to transformation. The subsequent sections of this chapter assess adaptation and mitigation options to facilitate building the resilience of health systems and healthcare facilities to recover better than before or to transform.
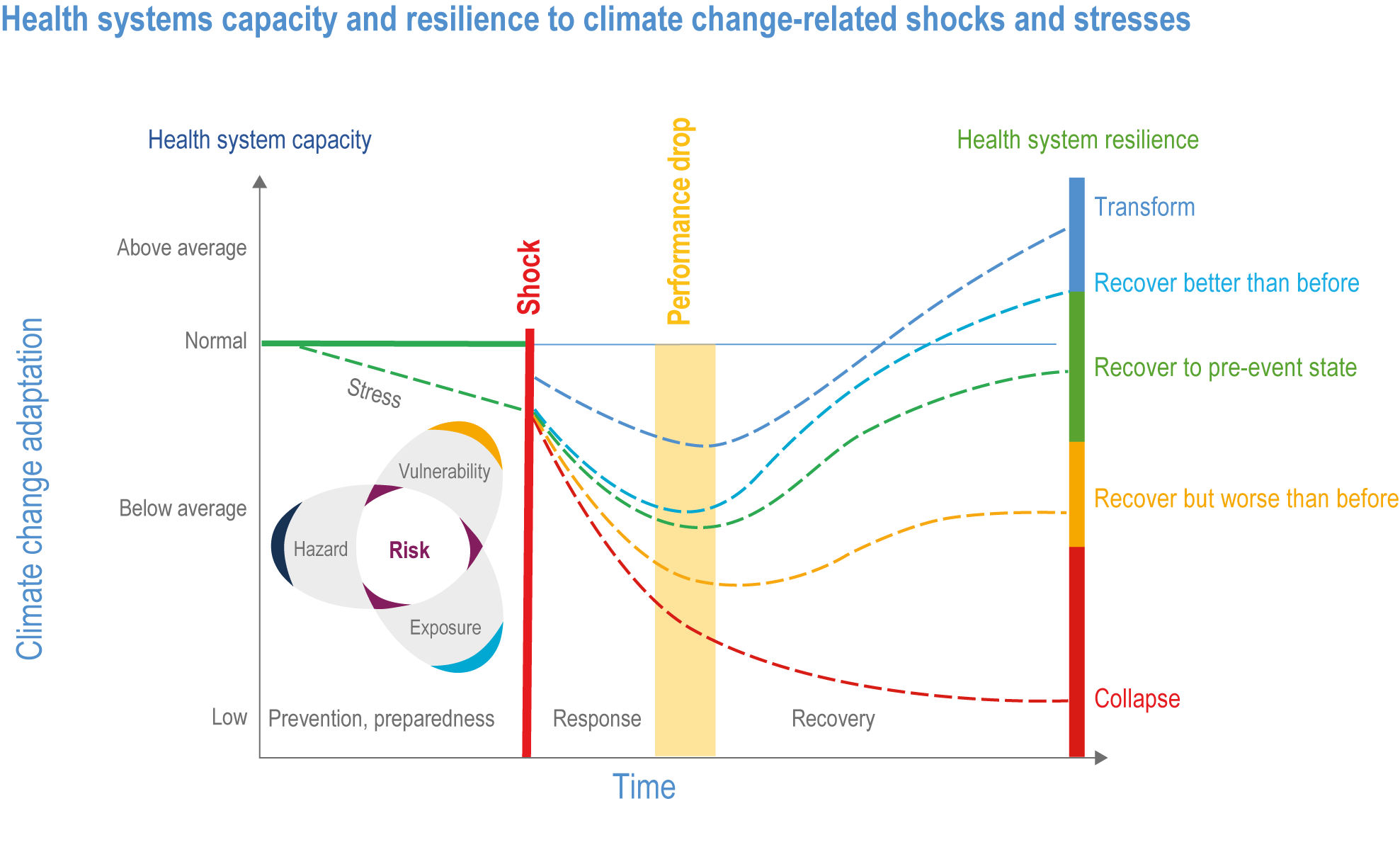
Figure 7.12 | Health systems capacity and resilience to climate change-related shocks and stresses. From WHO (2020).
7.4.2 Adaptation Strategies, Policies and Interventions
7.4.2.1 Current State of Health Adaptation
Analysis of the NDCs to the Paris Agreement to determine how health was incorporated, including impacts, adaptation and co-benefits, concluded that most low- and middle-income countries referred to health in their NDC (Dasandi et al., 2021). Figure 7.13 shows the degree of health engagement; this engagement is based on indicators measuring the specificity and detail of health references within a country’s NDC. Many vulnerable countries had high engagement of the health sector in the country NDC. However, this analysis did not determine whether the ambition expressed was sufficient to address the health adaptation needs.
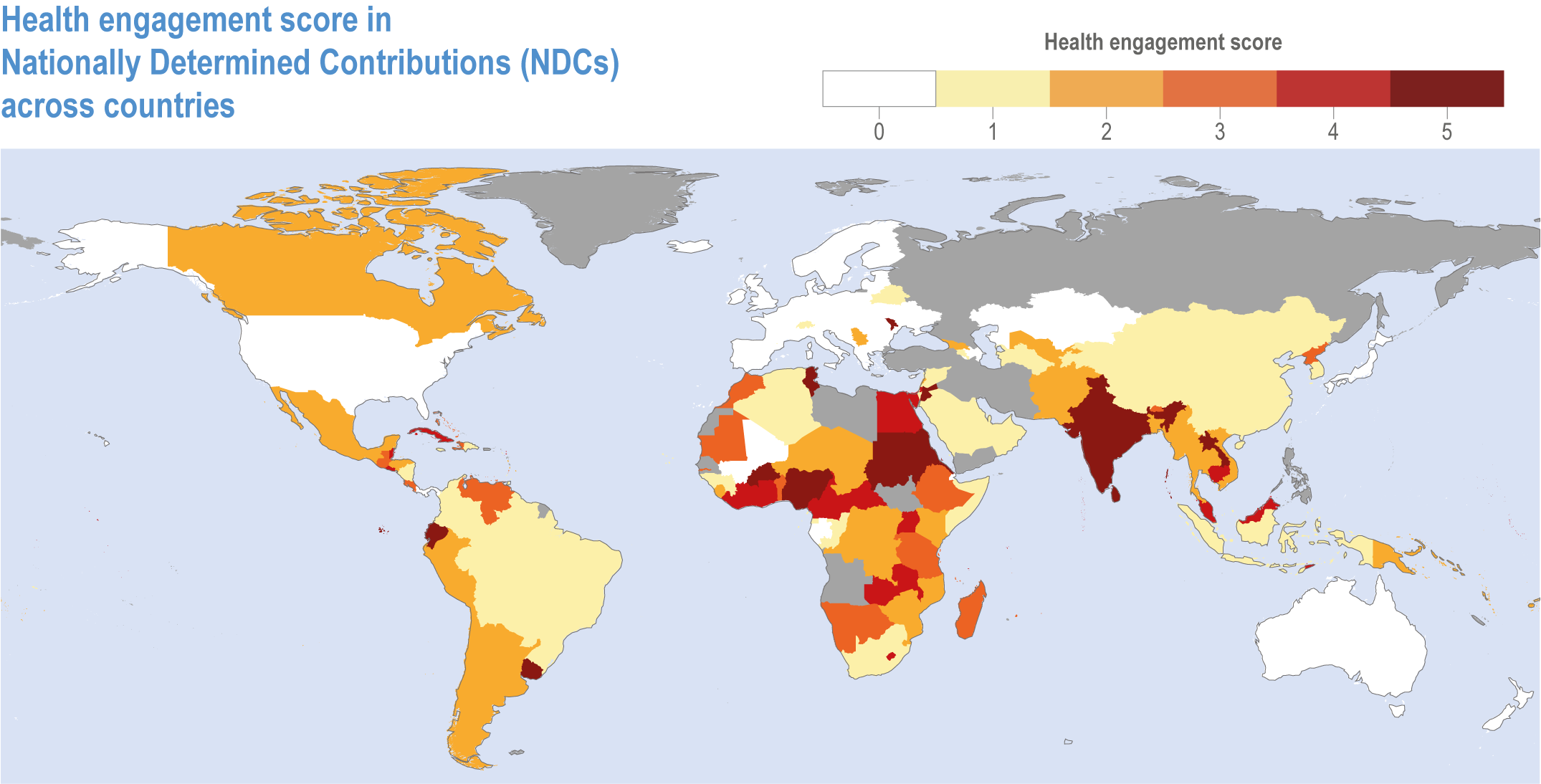
Figure 7.13 | Health engagement score in NDCs by country. Figure adapted from Dasandi et al. (2021).
The 2018 WHO Health and Climate Change Survey, a voluntary national survey sent to all 194 WHO member states, to which 101 responded, found that national planning on health and climate change is advancing, but the comprehensiveness of strategies and plans need to be strengthened. Implementing action on key health and climate change priorities remains challenging and multi-sectoral collaboration on health and climate change policy is evident, with uneven progress (Watts et al., 2021). Approximately 50% of respondent countries had developed national health and climate strategies, with over two-thirds doing so within the preceding five years, and 48 of 101 countries had conducted a health vulnerability and adaptation assessment (Watts et al., 2019). However, most countries reported only moderate or low levels of implementation, with financing cited as the most common barrier due to a lack of information on opportunities, in turn linked to a lack of connection by health actors to climate change policy processes and a lack of capacity to participate in national planning. A review of public health systems in 34 countries found that only slightly more than half considered climate change impacts and adaptation needs (Berry et al., 2018). Because the health risks of climate change often vary within a country, sub-national assessments and plans are needed to help local authorities protect and promote population health in a changing climate (Aracena et al., 2021; Basel et al., 2020; Schramm et al., 2020a).
7.4.2.2 Adaptation in Health Policies and Programmes
Health policies were historically not designed or implemented taking into consideration the risks of climate change and as currently structured are likely insufficient to manage the changing health burdens in coming decades (very high confidence). The magnitude and pattern of future health burdens attributable to climate change, at least until mid-century, will be determined primarily by adaptation and development choices. Current and future emissions will play an increasing role in determining attributable burdens after mid-century. Increased investment in strengthening general health systems, along with targeted investments to enhance protection against specific climate-sensitive exposures (e.g., hazard early warning and response systems and integrated vector control programmes for VBDs) will increase resilience if implemented to at least keep pace with climate change (high confidence). Investments to address the social determinants of health can reduce inequities and increase resilience (high confidence) (Thornton et al., 2016; Marmot et al., 2020; Wallace et al., 2015; Semenza and Paz, 2021).
Peer-reviewed publications of health adaptation to climate change in low- and middle-income countries have typically focused on flooding, rainfall, drought and extreme heat through improving community resilience, DRR and policy, governance and finance (Berrang-Ford et al., 2021; Scheelbeek et al., 2021). Health outcomes of successful adaptation have included reductions in infectious disease incidence, improved access to water and sanitation and improved food security. Figure 7.14 shows a Sankey diagram of climate hazards, adaptation responses and health outcomes. The figure highlights the range of health adaptation responses that are discussed in more detail earlier in this chapter and demonstrates the potential health benefit of adaptation efforts that affect a broad range of health determinants.
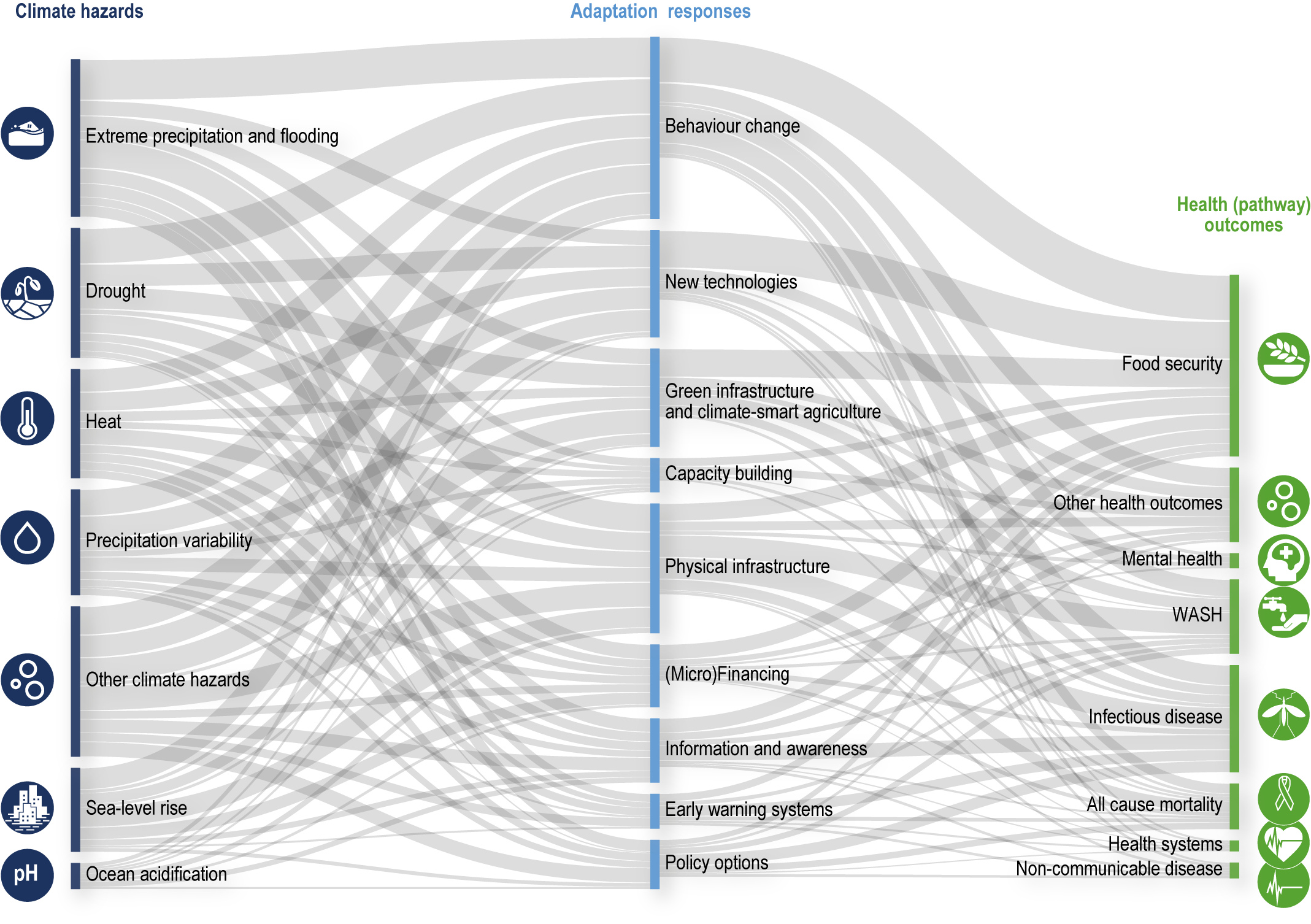
Figure 7.14 | Sankey diagram of climate hazards, adaptation responses and health outcomes. CSA is climate-smart agriculture. Source: Scheelbeek et al. (2021).
Questions of the feasibility and effectiveness of health adaptation options differ from those in other sectors because public health is a societal enterprise that cuts across many different spheres of society. Consequently, there are dependencies that lie outside the jurisdiction of the health sector. All the health risks of a changing climate currently cause adverse outcomes, with policies and programmes implemented in at least some health programmes in some places. Policies and programmes are continuously modified to increase effectiveness; this will need to accelerate in a changing climate. Improvements are needed as more is understood about disease aetiology, changing socioeconomic and environmental conditions, obstacles to uptake and other factors.
Policies and programmes for climate-sensitive health outcomes are only beginning to incorporate the challenges and opportunities of climate change, although this is critical for increasing resilience. The fundamentals of many policies and programmes in a changing climate will remain the same: implementing infectious disease control programmes, preventing heat-related mortality and morbidity and reducing the burden of other climate-related health endpoints, but activities will need to explicitly account for climate change to continue to protect health. Even with such attention to climate change, there are limits to the feasibility and effectiveness of health adaptation options for extreme heat, controlling emerging infectious diseases and controlling cascading risk pathways.
As discussed in Sections 1.4.2 and 1.5, an adaptation option is feasible when it is capable of being implemented by one or more relevant actors. In the health sector, WHO, the United Nations Children’s Fund (UNICEF) and other organisations provide technical expertise to ministries of health, who then provide national to local healthcare and public health services. Generally, the question is less of overall feasibility, given the range of potential adaptation options that have yet to be fully explored and implemented, but more of readiness to buy into the adaptation efforts required from health and other sectors. In specific contexts, feasibility also depends on governance capacity, financial capacity, public opinion and the distribution of political and economic power (Chapter 17). In other words, adaptation to climate change is broadly feasible with adequate investment and engagement, although this has yet to materialise, and in specific contexts feasibility is contingent and time-varying, and needs to be assessed at national to sub-national scales. For example, a scoping review in the Pacific region noted the following areas where further and significant investment and support are needed to increase feasibility of climate and health action: (a) health workforce capacity development, (b) enhanced surveillance and monitoring systems and (c) research to address priorities and their subsequent translation into practice and policy (Bowen et al., 2021). Vulnerability, adaptation and capacity assessments include consideration of the feasibility and effectiveness of priority health adaptation options and can help decision makers identify strategies for enhancing adaptation feasibility in specific contexts.
7.4.2.3 Adaptation Options for Vector-borne, Water-borne and Food-Borne Diseases
Integrated vector control approaches are crucial to effectively manage the geographic spread, distribution and transmission of VBDs associated with climate change (high confidence). Some of the projected risks of climate change on VBDs can be offset through enhanced commitment to existing approaches to integrated case management and integrated vector control management (Cissé et al., 2018; Confalonieri et al., 2017; Semenza and Paz, 2021). Important components include enhanced disease surveillance and early warning and response systems that can identify potential outbreaks at sub-seasonal to decadal time scales (Rocklöv and Dubrow, 2020; Semenza and Zeller, 2014; Table 7.3). In many cases, the exposure dynamics of VBDs are strongly influenced by socioeconomic dynamics that should be considered when developing and deploying adaptation options (UNEP, 2018). This is especially the case in low-income countries. For example, insufficient access to sanitation and the presence of standing water are important determinants of the presence of Aedes aegypti populations and the pathogens that cause visceral leishmaniasis (L. donovani and L. infantum) in urban and peri-urban areas. Low housing quality and lack of refuse management are associated with higher rodent infestation. Strategies expected to have important health co-benefits include those that support health systems strengthening and ecosystem health, improve access to health coverage, increase awareness and education and address the underlying conditions of uneven development and a lack of adequate housing and access to water and sanitation systems in areas endemic to mosquito-borne diseases (Semenza and Paz, 2021; Cross-Chapter Box ILLNESS in Chapter 2).
Table 7.3 | Summary of adaptation options for key risks associated with climate-sensitive vector-, water- and food-borne diseases (VBDs, WBDs, FBDs).
Key risk | Geographic region(s) at higher risk | Consequence that would be considered severe and to whom | Hazard conditions that would contribute to this risk being severe | Exposure conditions that would contribute to this risk being severe | Vulnerability conditions that would contribute to this risk being severe | Adaptation options with high potential for reducing risk | Selected key references |
VBDs | Global | Increase in the incidence of some VBDs, such as malaria, dengue and other mosquito-borne diseases, in endemic areas and in new risk areas (e.g., cities, mountains and Northern Hemisphere) | Increased climatic suitability for transmission (e.g., enhanced vectorial capacity through a temperature shift) | Large increases in human exposure to vectors driven by growth in human and vector populations, globalisation, population mobility and urbanisation | Few effective vaccines, weak health systems, ineffective personal and household protections, susceptibility to disease, poverty, poor hygiene conditions, insecticide resistance and behavioural factors | Improved housing, better sanitation conditions and self-protection awareness; insecticide-treated bed nets and indoor spraying of insecticide; broader access to healthcare for the most vulnerable; establishment of disease surveillance and early warning systems for VBDs; cross-border joint control of outbreaks; effective vector control; targeted efforts to develop vaccines | Cissé et al. (2018); Semenza (2021); Rocklöv and Dubrow. (2020) |
WBDs | Mostly low- and middle-income countries (Africa and Asia); small islands; global for Vibrios | Increase in the occurrence and intensity of WBDs such as Vibrios (particularly V. cholerae), diarrhoeal diseases and other waterborne GI illnesses | Substantial changes in temperature and precipitation patterns, increased frequency and intensity of extreme weather events (e.g., droughts, storms and floods), ocean warming and acidification | Large increases in exposure, particularly in flood-prone areas with poor sanitation and favourable ecological environments for WBD pathogens | Poor hygiene conditions, lack of clean drinking water and safe food, flood- and drought-prone areas and vulnerable water and sanitation systems | Improved WASH conditions and surveillance systems; improved personal drinking and eating habits; behaviour change | Brubacher et al. (2020); Ford and Hamner (2018); Lake (2018); Levy et al. (2018); Nichols et al. (2018); Rocklöv et al. (2021) |
FBDs | Global | Increase in the occurrence and intensity of FBDs such as Salmonella and Campylobacter, including in high-income countries | Substantial changes in temperature and precipitation patterns, increased frequency and intensity of extreme weather events (e.g., droughts, storms and floods), ocean warming and acidification | Large increases in exposure, particularly in flood-prone areas with poor sanitation and favourable ecological environments for FBD pathogens | Poor hygiene conditions; lack of clean drinking water and safe food; flood- and drought-prone areas; vulnerable water and sanitation systems, food storage systems, food processes, food preservation and cold chain/storage | Improved WASH conditions and surveillance systems; improved personal drinking and eating habits; behaviour change; improved food storage, food processing, food preservation and cold chain/storage | Brubacher et al. (2020); Ford and Hamner (2018); Lake (2018); Levy et al. (2018); Nichols et al. (2018); Rocklöv et al. (2021) |
Adaptation options for climate-related risks for WBDs and FBDs are strongly associated with wider, multi-sectoral initiatives to improve sustainable development in low-income communities (high confidence). Effective measures include improving access to potable water and reducing exposure of water and sanitation systems to flooding and extreme weather events (Brubacher et al., 2020; Cisse, 2019; Table 7.3). This requires focusing on farm-level interventions that limit the spread of pathogens into adjacent waterways, preventing the ongoing contamination of water and sanitation systems and the promotion of food-safe human behaviours (Levy et al., 2018; Nichols et al., 2018). It is also important to implement well-targeted and integrated WASH interventions, including at schools and ensuring proper disposal of excreta and wastewater. Cities can integrate regional climate projections into their engineering models to produce lower-risk source waters and increase the resilience of water and sanitation technologies and management systems under a range of climate scenarios. Technologies can help abstract source waters from depth, introduce or increase secondary booster disinfection, design or modify systems to reduce residence times within pipes and/or coat exposed pipes (Levy et al., 2018). Other efficient interventions include source water protection, promoting water filtration, testing the presence of waterborne pathogens in shellfish, imposing trade restrictions where necessary and improving hygiene at all levels (Semenza and Paz, 2021). Needed actions include early warning and response systems, strengthening the resilience of communities and health systems and promoting ecosystem health, water safety plans and sanitation safety plans (Brubacher et al., 2020; Cisse, 2019; Ford and Hamner, 2018; Lake and Barker, 2018; Levy et al., 2018; Nichols et al., 2018; WHO and International Water Association, 2009; WHO, 2016a; WHO, 2018b; Semenza, 2021; Rocklöv et al., 2021).
7.4.2.4 Adaptation Options for Heat-Related Morbidity and Mortality
Adaptations options for heat refer to strategies implemented at short time scales such as air conditioning and HAPs, including heat warning systems and longer-term solutions such as urban design and planning and NbS (Table 7.4).
Table 7.4 | Summary of adaptation options for key health risks associated with heat.
Key risk | Geographic region | Consequence that would be considered severe, and to whom | Hazard conditions that would contribute to this risk being severe | Exposure conditions that would contribute to this risk being severe | Vulnerability conditions that would contribute to this risk being severe | Adaptation options with high potential for reducing risk | Selected key references |
Heat-related mortality, morbidity and mental illness |
|
|
|
|
|
| Benmarhnia et al. (2016); Chen et al. (2019); Jay et al. (2021); Heo et al. (2019b); Martinez-Solanas and Basagana (2019); Morabito et al. (2021); Schwingshackl et al. (2021) |
To date, air conditioning is the main adaptation approach for mitigating the health effects of high temperatures, especially in relation to cardiorespiratory health (Madureira et al., 2021). However, air conditioning may constitute a maladaptation because of its high demands on energy and associated heat emissions, especially in high-density cities (Eriksen et al., 2021; Magnan et al., 2016; Schipper, 2020), and also lead to ‘heat inequities’ as this is not an affordable or practical option for many (Jay et al., 2021; Turek-Hankins et al., 2021). HAPs link weather forecasts with alert and communication systems and response activities, including public cooling centres, enhanced heat-related disease surveillance and a range of individual actions designed to reduce the health effects of extreme heat events such as seeking shade and altering the pattern of work (McGregor et al., 2015). While well-designed and operationalisable HAPs possess the potential to reduce the likelihood of mortality from extreme heat events (medium confidence) (Benmarhnia et al., 2016; Heo et al., 2019b; Martinez-Solanas and Basagana, 2019; Martinez et al., 2019; De’Donato et al., 2018), full process and outcome-based evaluations of HAPs and their constituent components are lacking (Boeckmann and Rohn, 2014; Chiabai et al., 2018b; Boeckmann and Rohn, 2014; Nitschke et al., 2016; Diaz et al., 2019; Benmarhnia et al., 2016; Heo et al., 2019a; Heo et al., 2019b; Ragettli and Roosli, 2019). Evaluations of heatwave early warning systems as a component within HAPs show inconsistent results in terms of their impact on predicting mortality rates (Nitschke et al., 2016; Benmarhnia et al., 2016; Heo et al., 2019a; Heo et al., 2019b; Ragettli and Roosli, 2019; Martinez et al., 2019; De’Donato et al., 2018; Weinberger et al., 2018b), indicating climate-based heat warning systems, which use a range of heat stress metrics (Schwingshackl et al., 2021), are not sufficient as a stand-alone approach to heat risk management (high confidence). To support HAP and heat risk-related policy development, identification and mapping of heat vulnerability ‘hot spots’ within urban areas have been proposed (Chen et al., 2019; Hatvani-Kovacs et al., 2018)
A multi-sectoral approach, including the engagement of a range of stakeholders will likely benefit the response to longer-term heat risks through the implementation of measures such as climate-sensitive urban design and planning that mitigates UHI effects (high confidence) (Ebi, 2019; Jay et al., 2021; Alexander et al., 2016; Levy, 2016; Masson et al., 2018; McEvoy, 2019; Pisello et al., 2018). In the shorter-term, potentially localised solutions can include awnings, louvers, directional reflective materials, altering roof albedo, mist sprays, evaporative materials, green roofs and building facades and cooling centres (Jay et al., 2021; Macintyre and Heaviside, 2019; Spentzou et al., 2021; Takebayashi, 2018). NbS to reduce heat that offer co-benefits for ecological systems include green and blue infrastructure (e.g., urban greening/forestry and the creation of water bodies) (Koc et al., 2018; Lai et al., 2019; Shooshtarian et al., 2018; Ulpiani, 2019; Zuvela-Aloise et al., 2016; Hobbie and Grimm, 2020). The implementation of climate-sensitive design and planning can be constrained by governance issues (Jim et al., 2018) and the benefits are not always evenly distributed among residents. Implementation of climate-sensitive design and NbS does, however, need to be carried out within the context of wider public health planning because water bodies and moist vegetated surfaces provide suitable habitats for a range of disease vectors (Nasir et al., 2017; Tian et al., 2016; Trewin et al., 2020). Solutions recommended for managing exposure to heat in outdoor workers include improved basic protection (including shade and planned rest breaks), heat-appropriate personal protective equipment, work scheduling for cooler times of the day, heat acclimation, improved aerobic fitness, access to sufficient cold drinking water and on-site cooling facilities and mechanisation of work (Morabito et al., 2021; Morris et al., 2020; Varghese et al., 2020; Williams et al., 2020).
Most adaptation options were developed in high- and middle-income countries and typically require significant financial resources for their planning and implementation. Studies are needed of the benefits of indigenous and non-Western approaches to managing and adapting to extreme heat risk. Recently published reviews of approaches to heat adaptation outline the nature and limitations of a range of cooling strategies with optimal solutions for a number of settings recommended (Jay et al., 2021; Turek-Hankins et al., 2021).
7.4.2.5 Adaptation Options for Air Pollution-related Health Effects
As noted in Section 7.3.1.6, air pollution projections indicate ambitious emission reduction scenarios or stabilisation of global temperature change at 2°C or below would yield substantial co-benefits for air quality-related health outcomes. Improvements in air quality could be achieved by the deliberate adoption of a range of adaptation options to complement mitigation measures such as decarbonisation (e.g., renewable energy, fuel switching, energy efficiency gains and carbon capture storage and utilisation) and negative emissions technologies (e.g., bioenergy carbon capture and storage, soil carbon sequestration, afforestation and reforestation and wetland construction and restoration).
Adaptation options for air pollution include implementing ozone precursor emission control programmes; developing mass transit/efficient public transport systems in large cities; encouraging car-pooling, cycling and walking (active transport); traffic congestion charges; low emission zones in cities; integrated urban planning implementing NbS such as green infrastructure for pollutant interception and removal; managing wildfire risk regionally and across jurisdictional boundaries; developing air quality warning systems; altering activity on high pollution days; effective air pollution risk communication and education; wearing protective equipment such as face masks; avoiding solid fuels for cooking and indoor heating; ventilating and isolating cooking areas; and using portable air cleaners fitted with high-efficiency particulate air filters (Abhijith et al., 2017; Carlsten et al., 2020; Cromar et al., 2020; Ding et al., 2021; Holman et al., 2015; Jennings et al., 2021; Kelly et al., 2021; Kumar et al., 2019; Masselot et al., 2019; Ng et al., 2021; Riley, 2021; Voordeckers et al., 2021; Xu et al., 2017; Table 7.5). While the range of air pollution adaptation options is potentially extensive, barriers may need to be overcome to achieve successful implementation, including financial, institutional, political (i.e. inter- and intra-governmental) and social barriers (Barnes et al., 2014; Ekstrom and Bedsworth, 2018; Fogg-Rogers et al., 2021; Schumacher and Shandas, 2019).
Table 7.5 | Summary of adaptation options for key health risks associated with air pollution.
Key risk | Geographic region | Consequence that would be considered severe and to whom | Hazard conditions that would contribute to this risk being severe | Exposure conditions that would contribute to this risk being severe | Vulnerability conditions that would contribute to this risk being severe | Adaptation options with high potential for reducing risk | Selected key references |
Air pollution-related health effects |
|
|
|
|
|
| Carlsten et al. (2020); Doherty et al. (2017); Jennings et al. (2021); Kumar et al. (2019); Orru et al. (2017); Orru et al. (2019); Schumacher and Shandas (2019); Silva et al. (2017); Voordeckers et al. (2021) |
7.4.2.6 Multi-sectoral Adaptation for Risks of Malnutrition
Adaptation to reduce the risk of malnutrition requires multi-sectoral, integrated approaches (very high confidence). Adaptation actions include access to healthy, affordable diverse diets from sustainable food systems (high confidence) ; a combination of access to health—including maternal, child and reproductive health— and nutrition services, water and sanitation (high confidence); access to nutrition-sensitive and shock-responsive social protection (high confidence); and early warning systems (high agreement ), risk sharing, transfer, and risk reduction schemes such as index-based weather insurance (medium confidence) (Mbow et al., 2019; Swinburn et al., 2019; UNICEF/WHO/WBG, 2019; FAO et al., 2021; Macdiarmid and Whybrow, 2019; Liverpool-Tasie et al., 2021). Common enablers across adaptation actions that enhance the effectiveness and feasibility of the adaptation include: education, women’s and girls’ empowerment (high confidence), rights-based governance and peacebuilding social cohesion initiatives such as the framework of the Humanitarian Development and Peace Nexus (medium confidence).
Nutrition-sensitive and integrated agroecological farming systems offer opportunities to increase dietary diversity at household levels while building local resilience to climate-related food insecurity (high confidence) (Bezner Kerr et al., 2021; IPES-Food, 2020; Altieri et al., 2015) especially when gender equity, racial equity and social justice are integrated (Bezner Kerr et al., 2021). Adaptation responses include a combination of healthy, culturally appropriate and sustainable food systems and diets; soil and water conservation; social protection schemes and safety nets; access to health services; nutrition-sensitive risk reduction; community-based development; women’s empowerment; nutrition-smart investments; increased policy coherence; and institutional and cross-sectoral collaboration (high agreement, medium evidence) (FAO et al., 2018; Mbow et al., 2019; Pozza and Field, 2020; FAO et al., 2021; Table 7.7). Nutrition security can be enhanced through consideration of nutrient flows in food systems (Harder et al., 2021).This ‘circular nutrient economy’ perspective highlights the potential for adaptations throughout the food supply chain, including sustainable production practices that promote nutrient diversity and density, processing, storage, and distribution that conserves nutrition; equitable access and consumption of available, affordable, appropriate, and healthy foods; and waste management that supports nutrient recovery (Harder et al., 2021; Boon and Anuga, 2020; FAO et al., 2021; Pozza and Field, 2020; Ritchie et al., 2018). Traditional, indigenous and small-scale agroecology and regional food systems provide context-specific adaptations that promote food and nutrition security as well as principles of food sovereignty and food systems resilience (HLPE, 2020; Bezner Kerr et al., 2021; IPES-Food, 2020; IPES-Food, 2018).
A feasibility and effectiveness assessment was conducted for six adaptation strategies often used and recommended by the UN to respond to malnutrition risks that combined a literature review and expert judgment assessment of 80 peer-reviewed studies (UNSCN, 2010; Tirado et al. 2013; methods adapted from de Coninck et al. (2018) and Singh et al. (2020)). Nineteen indicators of six dimensions of feasibility (economic, technical, social, institutional, environmental and geophysical) were considered. The lead time to initiate and the expected longevity of each option were examined. Feasibility was defined as how significant the reported barriers were to implement a particular adaptation option. Highly feasible options were those where no or very few barriers were reported. Moderately feasible were those where barriers existed but did not have a strong negative effect on the adaptation option (or evidence was mixed). Low feasibility options had multiple barriers reported that could block implementation. Effectiveness ratings were based on expert consultation and reflected the potential of the adaptation option to reduce risk. The final effectiveness and feasibility scores were categorised as high, medium or low and reflect the combined results of all studies for a given adaptation option (Table 7.6).
Table 7.6 | Feasibility and effectiveness assessments of multi-sectoral adaptation for food security and nutrition.
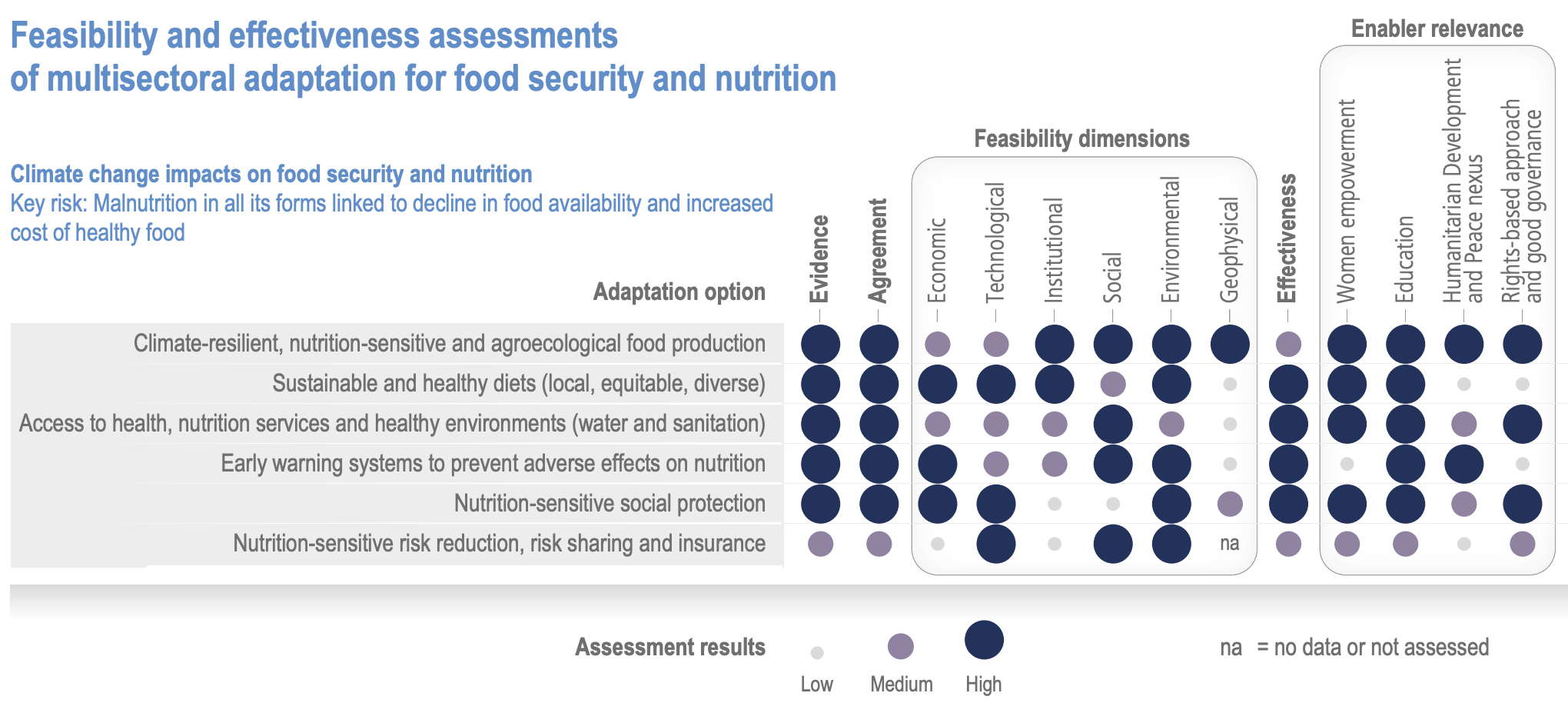
Adaptive social protection programmes and mechanisms that can support food insecure households and individuals include cash transfers or public work programmes, land reforms, and extension of credit and insurance services that reduce food insecurity and malnutrition during times of environmental stress (Carter and Janzen, 2018; Johnson et al., 2013; Alderman, 2016). For example, children from families participating in Ethiopia’s Productive Safety Net Program experienced improved nutritional outcomes, partly due to better household food consumption patterns and reduced child labour (Porter and Goyal, 2016). School feeding programmes improve nutritional outcomes, especially among girls, by promoting education, and by reducing child pregnancy and fertility rates (Bukvic and Owen, 2017). Adaptive social protection is most effective when it combines climate risk assessment with DRR and wider socioeconomic development objectives (Davies et al., 2013).
Transformative approaches towards healthier, more sustainable, plant-based diets require integrated strategies, policies and measures, including economic incentives for the agroecological production and equitable access to and consumption of more fruits, vegetables and pulses; inclusion of sustainability criteria in dietary guidelines, labelling and public education programmes; and promoting collaboration, good governance and policy coherence (Glover, 2019).
Table 7.7 | Summary of adaptation options for key risks associated with malnutrition.
Key risk | Geographic region | Consequence that would be considered severe and to whom | Hazard conditions that would contribute to this risk being severe | Exposure conditions that would contribute to this risk being severe | Vulnerability conditions that would contribute to this risk being severe | Adaptation options with high potential for reducing risk | Selected key references |
Malnutrition due to decline in food availability and increased cost of healthy food |
|
|
|
|
|
| Glover and Poole (2019); Mbow et al. (2019); Swinburn et al. (2019) |
7.4.2.7 Adaptation Options for Risks to Mental Health
Adaptation options for reducing mental health risks associated with extreme weather include preventive and post-event responses (high confidence) (Brown et al., 2017; Cohen, 2019; James et al., 2020; Table 7.8). Responses include improving funding and access to mental healthcare, which is under-resourced (WHO, 2019a); surveillance and monitoring of psychosocial impacts of extreme weather events; community-level planning for mental health as part of climate-resilience planning (Clayton et al., 2017); and mental health and psychological first aid training for care providers and first responders (Hayes et al., 2018; O’Donnell et al., 2021; Hayes et al., 2018; Taylor, 2020; Morgan et al., 2018; Sijbrandij et al., 2020). Legislation can ensure access to services as well as establish a regulatory framework (Ayano, 2018). Advanced disaster risk planning reduces post-event mental health challenges. One example is from China, where pre-planning of temporary shelters resulted in significantly lower rates of anxiety, depression and PTSD in the aftermath of flooding among displaced people who accessed them (Zhong et al., 2020). Key elements of successful initiatives include coordinated planning and action between key regional agencies and governments with a focus on improving accountability and removing barriers to implementation and subsequent access to programmes (Ali et al., 2020). As an example, following the 2019/2020 Australian bushfires, the federal government allocated funds to support mental health through free counselling for those affected, increased access to telehealth, extended hours for mental health services and programmes designed specifically for youth (Newnham et al., 2020).
Table 7.8 | Summary of adaptation options for key risks associated with mental health.
Key Risk | Geographic region | Consequence that would be considered severe and to whom | Hazard conditions that would contribute to this risk being severe | Exposure conditions that would contribute to this risk being severe | Vulnerability conditions that would contribute to this risk being severe | Adaptation options with high potential for reducing risk | Selected key references |
Mental health impacts in response to floods, storms, and wildfires |
|
|
|
|
|
| Ali et al. (2020); Ayano (2018); Buckley et al. (2019); Clayton et al. (2017); Hayes et al. (2019); James et al. (2020); Sijbrandij et al. (2020) |
Because mental health is fundamentally inter-twined with social and economic well-being, adaptation for climate-related mental health risks benefits from wider multi-sectoral initiatives to enhance well-being, with the potential for co-benefits to emerge (high confidence). Improvements in education, quality of housing, safety and social protection support enhance general well-being and make individuals more resilient to climate risks (Lund et al., 2018; Hayes et al., 2019). Among Indigenous Peoples, connections to traditional culture and to place are associated with health and well-being (Bourke et al., 2018) as well as with resilience to environmental change (Ford et al., 2020). As an example of the connection between infrastructure improvements and mental health, a study of domestic rainwater harvesting initiatives to promote household water security also improved mental health in participating households (Mercer and Hanrahan, 2017). Adaptive urban design that provides access to healthy natural spaces—an option for reducing risks associated with heat stress—also promotes social cohesion and mitigates mental health challenges (high confidence) (Buckley et al., 2019; Clayton et al., 2017; Jennings and Bamkole, 2019; Liu et al., 2020b; Mygind et al., 2019; Marselle et al., 2020).
7.4.2.8 Adaptation Options to Facilitate Early-Warning and Response Systems
Early warning systems are a potentially valuable tool in adapting to climate-related risks associated with infectious diseases when based on forecasts with high skill and when there are effective responses within the time frame of the forecast (high confidence). Through advanced seasonal weather forecasting that draws upon established associations between weather/climate and infection/transmission conditions, conditions conducive to disease outbreaks can be identified months in advance, providing time to implement effective population health responses (Morin et al., 2018). Most current early warning systems are focused on malaria and dengue but there are examples for other diseases, such as an early warning system developed for Vibrios monitoring in the Baltic Sea (Semenza et al., 2017). An early warning system for dengue outbreaks in Colombia based on temperature, precipitation and humidity successfully detected 75% of all outbreaks between one and five months in advance, detecting 12.5% in the same month (Lee et al., 2017b). Dengue warning systems in Brazil, Malaysia and Mexico have generated satisfactory results (Hussain-Alkhateeb et al., 2018). An effective early warning system for malaria was implemented in the Amhara region of Ethiopia (Merkord et al., 2017).
Early warning systems are effective at detecting and potentially reducing food security and nutrition risks (high confidence). Examples of proven systems include the United States Agency for International Development (USAID) Famine Early Warning System, the Food and Agricultural Organization’s Global Information and Early Warning System and the World Food Programme’s Corporate Alert System. Such systems are fundamental for anticipating when a crisis might occur and setting priorities for interventions (Funk et al., 2019). Financial investments to develop early warning systems are cost-effective and reduce human suffering (Choularton and Krishnamurthy, 2019) (high confidence). For instance, during the 2017 drought-induced food crisis in Kenya, 500,000 fewer people required humanitarian assistance than would have been expected based on past experiences; this was largely due to timely and effective interventions triggered by the early warning (Funk et al., 2018).
Early warning systems have been established for other climate-sensitive health outcomes, such as respiratory diseases associated with air pollution (Shih et al., 2019; Li and Zhu, 2018; Yang and Wang, 2017). Early warning systems for non-heat extreme weather and climate events, such as storms and floods, are designed to protect human health and well-being; disaster risk management organisations and institutions typically communicate these warnings through their networks. Research is ongoing to extend the time period for warnings.
7.4.2.9 Incorporating Disaster Risk Reduction into Health Adaptation
Integrating health into national disaster risk management plans has wider benefits for resilience and adaptation to climate change risks (high confidence) (UNFCCC, 2017a; Watts et al., 2019). DRR, including disaster preparedness, management and response, is widely recognised as important for reducing health consequences of climate-related hazards and extreme weather events (Keim, 2008; Phalkey and Louis, 2016). A systematic review by Islam et al. (2020) identified multiple, ongoing challenges to integrating climate adaptation and DRR at global and national levels, including a lack of capacity among key actors and institutions, a lack of coordination and collaboration across scales of government and general lack of funding—challenges that are particularly relevant for the health sector. Global events, including climate-related extreme events and public health emergencies of international concern (for example, Ebola, Middle East respiratory syndrome (MERS) and COVID-19) have influenced the development of national public health preparedness and response systems and attracted significant investment over the last two decades (Khan et al., 2015; Murthy et al., 2017; Watson et al., 2017). The Sendai Framework for Disaster Risk Reduction and the International Health Regulations establish important global and regional goals for increasing health system resilience and reducing health impacts from biological hazards and extreme climate events (Aitsi-Selmi et al., 2015; Maini et al., 2017; UNFCCC, 2017b; Wright et al., 2020). There are explicit links between the health aspect of the Sendai Framework and UN SDGs 1, 2, 3, 4, 6, 9, 11, 13, 14, 15 and 17 (Wright et al., 2020). More specifically, reducing the number of disaster-related deaths, illnesses and injuries, as well as damage to health facilities are key indicators for achieving the goals set out in the Sendai Framework (UNFCCC, 2017b).
The intersection of health and multi-sectoral DRR and management, generally described as health emergency and disaster risk management (health-EDRM), encompasses multi-sectoral approaches from epidemic preparedness and response including the capacities for implementing the International Health Regulations (IHR, 2005), health systems strengthening and health systems resilience (Lo Iacono et al., 2017; WHO 2019; Wright et al., 2020). Health-EDRM costs to governments are notably lower than the cost of inaction (Peters et al., 2019). Additional per capita costs in low-income countries have been estimated to range from USD 4.33 (capital) and USD 4.16 (annual recurrent costs), and in upper middle-income countries to an additional USD 1.35 in capital costs and USD 1.41 in extra annual recurrent costs (Peters et al., 2019). Adopting a health-EDRM approach supports the systematic integration of health and multi-sectoral EDRM to ensure a holistic approach to health risks and assists in the alignment of action in health security, climate change and sustainable development (Chan and Peijun, 2017; Dar et al., 2014; WHO, 2019; Wright et al., 2020).
Climate-informed health-EDRM is crucial for the climate resilience of health systems (WHO, 2015a), particularly to account for additional risks and uncertainties associated with climate change and allow for well-planned, effective and appropriate EDRM and adaptation (Watts et al., 2018a; WHO, 2013; WHO, 2015a). Potential coherent approaches to addressing climate change and disaster risks to health include: strengthening health systems; vulnerability and risk assessments that incorporate disaster and climate change risk; building resilience of health systems and health infrastructure; and climate-informed EWSs (Banwell et al., 2018; Phalkey and Louis, 2016). However, a review of DRR projects including climate change in south Asia found that the health sector was the least represented with only 2% of 371 projects relating to health (Mall et al., 2019), indicating a need to strengthen the incorporation of climate change in health-EDRM. Current tracking under the Sendai Framework of Disaster Risk Reduction 2015–2030 shows that most countries (particularly low-income countries and lower middle-income countries) still lack robust systems for integrated risk monitoring and early warning (UNEP, 2018). The incorporation of DRR and management strategies into climate adaptation for health and health systems at local scales is particularly important, given that it is at local scales where health services are most often delivered and where knowledge of specific needs and challenges is often greatest (Amaratunga et al., 2018; Schramm et al., 2020a). Indigenous knowledge has been shown to be valuable in DRR, with particularly strong evidence existing for drought risk reduction in sub-Saharan Africa (Fummi et al., 2017; Muyambo et al., 2017; Dube and Munsaka, 2018; Macnight Ngwese et al., 2018). In the USA, DRR strategies that draw upon traditional knowledge and local expertise are being incorporated into climate adaptation planning for health in a number of indigenous communities under the ‘Climate-ready Tribes Initiative’ (Schramm et al., 2020b).
7.4.2.10 Monitoring, Evaluation and Learning
Monitoring, evaluation and learning (MEL) can assess the ability of nations and communities to prepare for and adequately respond to the health risks of climate change over time (high confidence) (Boyer et al., 2020). MEL describes a process that includes baseline assessment, prioritising actions and activities, identifying key indicators to track, ongoing data collection and periodically considering new information (Kruk et al., 2015). MEL determines whether adaptation options achieved their goals and whether resources were used effectively and efficiently (Boyer et al., 2020). One of the challenges for MEL in the context of adaptation is that climate risks vary as a function of time, location, socioeconomic development, demographics and activities in other sectors (Ebi et al., 2018a). MEL indicators in the health sector need to account for factors related to governance, implementation and learning as well as for exposures, impacts and programmatic activities, all of which are context dependent and are often outside the health sector (Boyer et al., 2020; Ebi et al., 2018a; Fox et al., 2019).
No universal standardised approach exists for monitoring or evaluating adaptation activities in the health sector (high confidence). Candidate indicators of climate change health impacts and adaptation activity, typically at the national level, are available (Bowen and Ebi, 2017; Cheng and Berry, 2013; Kenney et al., 2016; Navi et al., 2017; WHO, 2015b). Indicators are best grouped by category of activity, that is, vulnerability, risk and exposure; impacts; and adaptation and resilience (Ebi et al., 2018a). As health adaptation expands, enhanced monitoring will be needed to ensure that scientific advances are translated into policy and practice. A promising initiative that emerged since the AR5 is the Lancet Countdown, which represents a global effort at tracking various indicators of exposures, impacts, adaptation activities, finance and media activity related to climate change and health (Watts et al., 2018a), although this effort is principally focused on monitoring and does not explicitly focus on evaluation adaptation efforts or learning from adaptation efforts.
Community-based monitoring of adaptation responses to health impacts, especially by Indigenous Peoples, has not been widely undertaken, despite its potential to improve monitoring of and local adaptation to environmental change (Kipp et al., 2019). The health sector has been particularly weak at recognising the climate impacts on and the adaptation needs of Indigenous Peoples and in engaging Indigenous Peoples in monitoring progress (Ford et al., 2018; David-Chavez and Gavin, 2018; Ramos-Castillo et al., 2017). Successful adaptation to the health impacts of climate change in Indigenous Peoples requires recognition of their rights to self-determination, focusing on indigenous conceptualisations of well-being, prioritising Indigenous knowledge and understanding the broader agenda of decolonisation, health and human rights (high confidence) (Ford and King, 2015; Green and Minchin, 2014; Hoy et al., 2014; Jones, 2019; Jones et al., 2014; Mugambiwa, 2018; Nursey-Bray and Palmer, 2018).
Indicators should capture measures of processes that drive adaptation readiness, including leadership, institutional learning and inter-sectoral collaboration (Boyer et al., 2020; Ford and King, 2015) as well as outcome measures such as the presence of programming known to reduce risks (Ebi et al., 2018a). Additionally, indicators related to scaling up of effective interventions and relying on the implementation of science frameworks are important (Damschroder et al., 2009; Theobald et al., 2018, 2020; Ebi et al., 2018a; Fox et al., 2019). Measuring impacts attributable to climate change could be addressed with a combination of indicators related to overall health system performance and population vulnerability (Ebi et al., 2017; Ebi et al., 2018a).
7.4.3 Enabling Conditions and Constraints for Health Adaptation
7.4.3.1 Governance, Collaboration and Coordination
Effective governance institutions, arrangements, funding and mandates are key for adaptation to climate-related health risks (high confidence). Without integration and collaboration across sectors, health adaptation can become siloed, leading to less effective adaptation or even maladaptation (Magnan et al., 2016; Fox et al., 2019). Integration and collaboration include working laterally across national government departments and agencies, as well as vertically from national agencies to local governments and with the private sector, academia, NGOs and civil society. In this context, top-down policy design and implementation are complemented by bottom-up approaches that engage community actors in programme design and draw upon their local practices, perspectives, opinions and experiences. Opportunities exist to better integrate public health into climate change discourse and policymaking processes, and to strengthen public health partnerships and collaborations (Awuor et al., 2020). Creating networks, integration across organisations and jointly developed policies can facilitate cross-sectoral collaboration (Bowen and Ebi, 2017).
7.4.3.2 Multi-sectoral Collaborations
Multi-sectoral collaborations aimed at strengthening the health sector can generate multiple co-benefits in other sectors (high agreement, medium evidence). Solutions for the health and well-being risks described in 7.2 and 7.3 often have their origins in sectors that include water, sanitation, agriculture, food systems, social protection systems, energy and key components of urban systems such as housing and employment (WHO, 2015a; Bowen et al., 2014b; Machalaba et al., 2015; Confalonieri et al., 2015; Bowen et al., 2014a; Semenza, 2021). Climate resilient development pursued in these other sectors, and in cooperation with the health sector, simultaneously increases the potential for adaptation and climate resilience in terms of health and well-being (high confidence) (Ahmad et al., 2017; Watts et al., 2018b; Levy and Patz, 2015; WHO, 2018a; Chiabai et al., 2018a; Dudley et al., 2015; Zinsstag et al., 2018; Sherpa et al., 2014).
7.4.3.3 Financial Constraints
Financial constraints are the most referenced barrier to health adaptation and so scaling up financial investments remains a key international priority (very high confidence) (Wheeler and Watts, 2018; UNFCCC, 2017a). AR5 estimated the costs of adaptation in developing countries at between USD 70 billion and USD 100 billion annually in the year 2050, but these are likely to be a significant underestimate, particularly in the years 2030 and beyond (UNEP, 2014). National surveys conducted by WHO identified financial constraints as a major barrier to the implementation of health adaptation priorities (WHO, 2019b; Watts et al., 2021). Novel research drawing on global financial transaction data suggests that in 2019, global financial transactions with the potential to deliver adaptation in the health and healthcare sector reached USD 18.4 billion, driven by transactions in high- and upper middle-income countries, with investment in Africa, Southeast Asia and the eastern Mediterranean mostly stagnant (Watts et al., 2021).
There has been limited participation of the health sector in international climate financing mechanisms (Martinez and Berry, 2018). Of 149 projects listed in the Adaptation Fund database in October 2020, a large number were broad-based initiatives that may have considerable indirect benefits for health systems, such as enhanced disaster preparedness and food security, but none were explicitly aimed at strengthening health systems or had directed funds through ministries of health. A review of projects funded by the major multi-lateral climate funds showed that less than 1.5% of dispersed adaptation funding and less than 0.5% of overall funding have been allocated to projects aimed at protecting health (WHO, 2015a). A survey of national public health organisation representatives from a mix of low-, middle- and high-income countries found that a lack of political commitment, insufficient coordination across sectors and inadequate funding for public health-specific adaptation initiatives were common barriers to building climate resilience (Marcus and Hanna, 2020). Under-investment in climate-specific initiatives in health systems coincides with persistent under-investment in healthcare more generally, especially in low- and middle-income countries (Schaferhoff et al., 2019).
Adaptation financing does not often reach places where the climate-sensitivity of the health sector is greatest (Weiler, 2019). Financial constraints in Africa are one of the key reasons for slow implementation of health adaptation measures (Nhamo and Muchuru, 2019). Strengthening health systems in vulnerable countries has the potential to reduce current and future economic costs related to environmental health risks, thus enabling reinvestment in the health system and sustainable development (WHO, 2020a; WHO, 2015a). Robust and comprehensive climate and health financing builds first on core health sector investments (WHO, 2015a). Other potential opportunities for resource mobilisation include health-specific funding mechanisms, climate change funding streams and investments from multi-sectoral actions and actions in health-determining sectors (WHO, 2015a). Incorporating climate change and health considerations into disaster reduction and management strategies could improve funding opportunities and increase potential funding streams (Aitsi-Selmi et al., 2015). Reinforcing cross-sectoral governance mechanisms maximises health co-benefits and economic savings by allowing for multi-sectoral costs and benefits to be comprehensively considered in decision-making (Belesova et al., 2016; WHO, 2020a; WHO, 2015b). An additional financial need concerns health research, the existing funding for which does not match what is needed to support the implementation of the combined objectives of the UN 2030 Agenda for Sustainable Development, the Sendai Framework for Disaster Risk Reduction and the Paris Agreement (Green and Minchin, 2014; Ebi, 2016; Green et al., 2017).
7.4.3.4 Perceptions of Climate Change Risks and Links to Adaptation
Adaptation decisions and responses to climate change can be influenced by perceptions of risks, which are shaped by individuals’ characteristics, knowledge and experience (medium agreement, medium evidence). Institutional and governmental responses are critical for adapting to climate-related risks in health and other sectors, but individual responses also are relevant, such as choosing to implement adaptation measures. Individual responses are in turn affected not only by capabilities but also by perceptions that climate change is real and requires a response (Ogunbode et al., 2019). Perceptions of climate risks are formed by experiences of changes in local weather and extreme weather events (Sattler et al., 2018; Sattler et al., 2020; van der Linden, 2015), observations of environmental changes (Hornsey et al., 2016), experiences of and knowledge about climate change impacts (Ngo et al., 2020; van der Linden, 2015) and individual characteristics such as values and worldviews (Poortinga et al., 2019) (high agreement, medium evidence). Risk perceptions include both logical assessments about the likelihood and severity of climate change impacts and affective feelings about those impacts. On average, affective measures of risk perception are more strongly associated with disaster preparation than cognitive measures (Bamberg et al., 2017; van Valkengoed and Steg, 2019).
In addition to perceptions of risk, the likelihood that an individual will implement behavioural adaptations or support relevant public policy is affected by subjective assessments of the response options (Bamberg et al., 2017; van Valkengoed and Steg, 2019; Akompab et al., 2013; Carman and Zint, 2020; Hornsey et al., 2016; Brenkert-Smith et al., 2015).
Efficacy beliefs, social norms and subjective resilience also affect adaptation behaviour (medium confidence), which has implications for communication about the need for climate adaptation. Efficacy beliefs represent the belief in one’s ability to carry out particular action(s) and the belief that the action(s) will have the desired outcome. Belief that one is personally able to complete a behaviour is moderately associated with engaging in disaster preparations (Navarro et al., 2021; van Valkengoed and Steg, 2019) and with adaptation intentions (Burnham and Ma, 2017). Collective efficacy, the belief that a group of people working together can achieve a desired outcome, is important for participating in community adaptation behaviours (Bandura, 1982; Chen, 2015; Thaker et al., 2015). Related to this is response efficacy, a belief that a behaviour will achieve its desired outcome, which is also moderately associated with engaging in disaster preparations (van Valkengoed and Steg, 2019). Collective efficacy can potentially be developed by strengthening communication networks and social ties within a community (Haas et al., 2021; Jugert et al., 2016). Norms describing the adaptation strategies of others in a community, particularly those with high social status, can either facilitate or inhibit individual adaptation decisions (Neef et al., 2018; Smith et al., 2021).
Distinct from efficacy beliefs, subjective resilience is a more general optimism or belief about one’s ability (Jones, 2019; Khanian et al., 2019). Subjective resilience (Clare et al., 2017) can influence preferred responses to climate change via assessment of one’s ability to engage in specific response options. Identities can influence assessment of subjective resilience. Place attachment, having a strong emotional connection to a particular location, is weakly associated with disaster preparation (Brügger et al., 2015). In some cases, place attachment may inhibit adaptive responses, either by reducing perceptions of risk or by making people reluctant to leave an area that is threatened (De Dominicis et al., 2015; van Valkengoed and Steg, 2019). Place attachment can also contribute to enhanced community resilience (Khanian et al., 2019; Jones, 2019; Wang et al., 2021).
7.4.4 Migration and Adaptation in the Context of Climate Change
7.4.4.1 Linkages between Migration, Adaptation and Household Resilience
AR5 (Chapter 17) concluded that migration is often, though not in all situations, a potential form of adaptation initiated by households. Subsequent research indicates that the circumstances under which migration occurs and the degree of agency under which household migration decisions are made are important determinants of whether migration outcomes are successful in terms of advancing the well-being of the household and providing benefits to sending and receiving communities (high confidence) (Adger et al., 2015; Cattaneo et al., 2019; Cross-Chapter Box MIGRATE in Chapter 7). Evidence from refugee studies and general migration research indicates that higher agency migration, in which migrants have mobility options, allows migrants greater opportunities for integrating into labour markets at the destination, makes it easier to remit money home and generally creates conditions for potential benefits for migrant households and for sending and receiving communities (International Organization for Migration, 2019). Bilateral agreements that facilitate labour migration have been identified as being especially urgently needed for Pacific small island states (Weber, 2017).
Adaptive migration and the implied assumption that people can or should simply move out of harm’s way is not a substitute for investment in adaptive capacity-building (high agreement ) (Bettini and Gioli, 2016). Climate-related migration, and especially involuntary displacement, often occurs only after in situ adaptation options have been exhausted and/or where government actions are inadequate (Adger et al., 2015; Ocello et al., 2015; Cross-Chapter Box MIGRATE in Chapter 7). The threshold at which household adaptation transitions from in situ measures to migration is highly context specific and reflects the degree of exposure to specific climate risks, mobility options and the socioeconomic circumstances of the household and local community (McLeman, 2017; Adams and Kay, 2019; Semenza and Ebi, 2019; Cross-Chapter Box MIGRATE in Chapter 7). A consistent theme in the research literature reviewed for all sections of this chapter is that proactive investments in health, social and physical infrastructure, including those not aimed specifically at climate risks, build societal adaptive capacity and household resilience. In turn, expanding the range of adaptation options available to households increases the likelihood that, when migration does occur, it does so under conditions of high agency that lead to greater chances of success. In communities where climate-related migration and/or relocation is occurring or may occur, policymaking and planning benefits from understanding the cultural, social and economic needs of exposed populations and helps in the identification of responses and policies that build resilience (Hino et al. 2017)
7.4.4.2 Climate, Migration and Linkages to Labour Markets and Social Networks
Adaptive climate-related migration is often closely related to wage-seeking labour migration (medium confidence). Due to the circumstances under which they move, climate-related migrants’ destinations, labour market choices and returns from migration may be more heavily constrained than those of other labour migrants (Jessoe et al., 2018; Wrathall and Suckall, 2016).Within low- and middle-income countries, rural–urban migrant networks are important channels for remittances that may help build socioeconomic resilience to climate hazards in sending areas (Porst and Sakdapolrak, 2020), with higher levels of wage-seeking labour participation observed in climate-sensitive locales in south Asia (Maharjan et al., 2020). Local-level research in China and south Asia shows, however, that the potential for remittances to generate improvements in household level adaptive capacity is highly context specific, has significant gender dimensions and depends on such factors as the nature of the hazard, the distance migrated and the length of time over which remittances are received (Banerjee et al., 2019a; Banerjee et al., 2019b). Social networks are a key asset in helping climate migrants overcome financial and structural impediments to their mobility, but these have their limits, particularly with respect to international migration (Semenza and Ebi, 2019). Since AR5, greater restrictions have emerged on movement between many low- and high-income countries (not including those necessitated by public health measures during the COVID-19 pandemic), a trend that, if it continues, would generate additional constraints on destination choices for future climate migrants (McLeman, 2019). Transnational diasporic connections are a potential asset for building resilience in migrant-sending communities highly exposed to climatic risks, with migrants’ remittances potentially providing resources for long-term resilience building, recovery from extreme events and reducing income inequality (Bragg et al., 2018; Mosuela et al., 2015; Obokata and Veronis, 2018; Shayegh, 2017; Semenza and Ebi, 2019). Safe and orderly labour migration is consequently a potentially beneficial component of wider cross-sectoral approaches to building adaptive capacity and supporting sustainable development in regions highly exposed to climate risks (McLeman, 2019).
7.4.4.3 Attitudes Towards Climate Migration
The success of climate-related migration as an adaptive response is shaped by how migrants are perceived and how policy discussions are framed (high agreement, medium evidence). The possibility that climate change may enlarge international migrant flows has in some policy discussions been interpreted as a potential threat to the security of destination countries (Sow et al., 2016; Telford, 2018), but there is little empirical evidence in peer-reviewed literature assessed for this chapter of climate migrants posing significant threats to security at state or international levels. There is also an inconsistency between framing in some policy discussions of undocumented migration (climate-related and other forms) as being ‘illegal’ and the objectives of the Global Compact on Safe, Orderly and Regular Migration and the Global Compact on Refugees (McLeman, 2019). Although climate-related migrants are not officially recognised as refugees under the 1951 Convention relating to the Status of Refugees, terms such as ‘climate refugees’ are common in popular media and some policy discussions (Høeg and Tulloch, 2018; Wiegel et al., 2019). The framing of migration policy discussions is relevant, for example, in discussing climate adaptation options for Pacific Island Countries, where there is considerable disagreement over policies that range from a ‘migration with dignity’ approach that would liberalise labour migration in the Pacific region to those that see migration as a last resort option to be avoided as much as possible (McNamara, 2015; Farbotko and McMichael, 2019; Oakes, 2019; Remling, 2020). A more beneficial policy framing in terms of ensuring that future migration contributes to climate resilience and sustainable development has been established since AR5 within the framework of the Global Compact for Safe, Orderly and Regular Migration (see Section 7.4.7.7).
Attitudes of residents in migrant-receiving areas with respect to climate-related migration warrant consideration when formulating adaptation policy (medium confidence). Existing research is modest and difficult to generalise with respect to the impacts of climate-related migration and displacement on social dynamics and stability in receiving destinations, with outcomes being tied to the attitudes and social acceptance of receiving communities and efforts to integrate migrant arrivals into the community (Koubi and Nguyen, 2020). Research from Kenya and Vietnam shows that residents of receiving communities view environmental drivers as being legitimate reasons for people to move and consequently tend not to stigmatise such migrants (Spilker et al., 2020). In these examples, urban residents viewed environmental motivations as being comparable to economic reasons for migrating and did not see climate-related migrants as posing any particular risks for receiving communities. However, case studies from India suggest that a lack of recognition by local authorities of climatic factors being legitimate drivers of rural–urban migration may lead to discrimination against migrants in terms of access to housing and other social protections, thereby undermining household resilience (Chu and Michael, 2018).
7.4.4.4 Planned Relocation and Managed Retreats
There is high agreement among existing studies that immobile populations often have high vulnerability and/or high long-term exposure to climate hazards, and that non-climatic political, economic and social factors within countries may strongly constrain mobility (Zickgraf, 2019; Ayeb-Karlsson et al., 2020; Cundill et al., 2021). Section 7.2.6.2 highlighted the particular vulnerability of immobile populations in the face of growing climatic risks. However, research suggests governments should be slow to label such populations as being ‘trapped’ or to actively promote relocations in the absence of local agreement that in situ adaptation options have been exhausted (Adams, 2016; Farbotko and McMichael, 2019). In the case of indigenous settlements, efforts made to incorporate traditional knowledge in decision-making and planning increase the potential for longer-term success (Manrique, 2018). Considerable health implications can emerge within populations that are relocated as part of a planned retreat, and represent an important consideration for planners that requires greater research (Dannenberg et al., 2019). Organised relocations are not inherently transformative in their outcomes but, depending on the circumstances under which they occur and on how issues of equity and respect for the rights of those affected are implemented, relocation could potentially represent a positive transformation (Siders et al., 2021).
Disruptive and expensive relocations of low-lying coastal settlements in many regions would become increasingly necessary in coming decades under high levels of warming (high confidence). Organised relocations require long-term innovation, planning and cooperation on the part of governments, institutions, affected populations and civil society (Hauer, 2017; Hino et al., 2017; Haasnoot et al., 2021; Moss et al., 2021). Recent examples illustrate the substantial financial costs of organised relocations, ranging from USD 10,000 per person in examples from Fiji to USD 100,000 per person in coastal Louisiana, USA (Hino et al., 2017). Organised relocations are politically and emotionally charged, may not necessarily be seen as desirable by exposed populations and are most successful when approached proactive and strategically to avoid increasing the socioeconomic vulnerability of those who are relocated (Jamero et al., 2017; Wilmsen and Webber, 2015; Chapin et al., 2016; McNamara et al., 2018; Hauer et al., 2019; Bertana, 2020). Key considerations for protecting the rights and well-being of people who might need to be resettled include proactive communication with and participation of the affected communities, availability of compensation, livelihood protection and ensuring there is permanence and security of tenure at the relocation destination (Tadgell et al., 2018). Availability of funds for resettlement, how to manage relocation from communally owned lands, how to value privately owned land to be abandoned and the potential for loss and damage claims are just some of the many potential complications (Marino, 2018; McNamara et al., 2018). As a proactive option, researchers in Bangladesh have suggested the creation of ‘migrant-friendly towns’ to provide options for autonomous relocation from hazardous areas (Khan and Huq, 2021).
7.4.5 Adaptation Solutions for Reducing Conflict Risks
There has been increased activity within the international community to understand and address climate–conflict linkages since AR5, with high level actions including the UN Climate Security Mechanism, launched in 2018 and tasked with providing integrated climate risk assessments to the United Nations Security Council and other UN bodies in partnership with UN and external actors (DPPA et al., 2020). G7 governments initiated an integrated agenda for resilience (Rüttinger et al., 2015) and the Berlin Call for Action in 2019 sought a foreign policy platform to address climate security concerns, focusing on risk-informed planning, enhanced capacity for action within the UN and improvements to operational response to climate security risks (Federal Foreign Office, 2019). The non-peer-reviewed literature that currently addresses these policy dimensions is often generated by a small number of consultancies funded by governments from the Global North and can lack diverse perspectives and priorities.
7.4.5.1 Environmental Cooperation and Peacebuilding
The environment can form the basis for active peacebuilding, and a sustainable natural environment is important for ongoing peace (high agreement, medium evidence). EP is a framework increasingly utilised to understand the diverse ways in which the natural environment supports peace and can be utilised in peacebuilding; key tenets include preserving the natural environment such that degradation does not contribute to violence, protecting natural resources during conflict and using natural resources to support post-conflict economic recovery (Kron, 2019). EP frames natural resources as facilitating peace rather than driving conflict (Dresse et al., 2019) with emerging literature analysing what this means in practice (Kovach and Conca, 2016; Krampe, 2017; Ide, 2019; Ide et al., 2021; Johnson, 2021; Kalilou, 2021). There is emergent evidence for the success of EP pathways. For example, a natural resource sharing agreement on the Kenya–Uganda border was able to reconcile spatial, logistical and conceptual barriers to addressing climate risks in development contexts (Abrahams, 2020). However, the long-term impacts of EP approaches on sustaining peace are yet to be monitored and evaluated (Ide and Tubi, 2020). EP may be successful depending on the context and the element of peace being built (Johnson, 2021) or undermine processes when environmental arguments are co-opted for geopolitical purposes (Barquet, 2015) or to depoliticise conflict (Ide, 2020).
Formal institutional arrangements for natural resource management can contribute to transnational cooperation (high confidence) (see also Chapter 4). Evidence from transboundary water sharing agreements provides evidence for cooperation rather than conflict over resources (Timmerman et al., 2017; Timmerman, 2020; Dinar et al., 2015). Transboundary water agreements and river basin organisations help build robust institutions that facilitate trust and relationship building that have benefits in other domains (strong agreement, medium evidence) (Dombrowsky, 2010; Krampe and Gignoux, 2018; Barquet et al., 2014; Ide and Detges 2018). However, outcomes can be mixed, and the international and top down nature of these approaches may limit their transferability to intra-state conflicts at local levels (Rigi and Warner, 2020; Ide et al., 2021; Krampe et al., 2021).
7.4.5.2 Adaptation in Fragile Settings
Climate-resilient peacebuilding has the potential to limit the impact of future climate change on peace efforts (medium confidence). Practical guidance has been developed, driven by policy concerns on climate–conflict links. The United Nations Environment Programme (UNEP), the European Union and Adelphi have developed a toolkit for addressing climate fragility risks in peacebuilding, adaptation and livelihoods support (UNEP et al., 2019). Crawford et al. (2015) provide recommendations for climate-resilient peacebuilding consistent with the UN Secretary General’s five peacebuilding principles, including integrating ex-combatants through the construction of climate-resilient infrastructure, using climate impacts as a platform to engage previously conflicting groups, developing national DRR and management strategies, and climate-proofing economic development activities. The USAID, in a report prepared for the Adaptation Thought Leadership and Assessments (ATLAS) programme (Adelphi & Chemonics International, 2020) that drew upon resilience and peacebuilding programmes in the Horn of Africa, recommend two critical conditions to ensure activities address compound climate fragility risks. Firstly, conducting local analyses of the links between climate, conflict and fragility to identify specific risks to target and, secondly, ensuring long-term commitment with a focus on participation and flexibility.
Conflict-sensitive adaptation that focuses on institutional frameworks, conflict management and governance mechanisms has the potential to address complex interacting risks and emergencies over the long term (medium agreement, limited evidence) (Scheffran et al., 2012; Matthew, 2018; Okpara et al., 2018). However, most adaptation activities are planned and implemented under development or climate finance funds without systematic integration of conflict sensitivity, and National Adaptation strategies rarely and only implicitly address conflict and potential changes to power relations (Tänzler et al., 2019). Practitioners and policy researchers have attempted to address this gap by developing guidance and delivering training (e.g., Tänzler et al. (2019); Bob and Bronkhorst (2014)). However, there are real challenges relating to discounting indirect impacts on conflict and maladaptation (Asplund and Hjerpe, 2020) and risks of unintended outcomes (Mirumachi et al., 2020). Crawford and Church (2020) highlight the synergies between adaptation planning under the UNFCCC’s National Adaptation Plan process and conflict reduction. Discussing development more broadly, Abrahams (2020) suggests three barriers to development that incorporate conflict–climate risks: geographically disconnected impacts and outcomes, the discourse of climate as a threat multiplier (rather than underlying peace) and teleconnected risks occurring at different scales. Effective approaches rely on understanding local power dynamics and social relations (Sovacool 2018; Roth et al. 2019; Sapiains et al. 2021) (high agreement, medium evidence).
7.4.5.3 Gender-Based Approaches to Peacebuilding
Gender-based approaches provide novel under-utilised pathways to achieving sustainable peace (high confidence). Security council resolutions have encouraged the incorporation of gender analysis into peacebuilding and research has shown that taking into account the gendered nature of networks and dialogues opens new avenues for cooperation that are conflict sensitive (Dunn and Matthew, 2015), creating potential for women’s rights and advocacy groups to be drivers of peace (Céspedes-Báez, 2018). For example, women are working to reduce climate vulnerability security risks in urban settings by entering local politics and joining community-based organised and civil society networks (Kellog, 2020). The gendered nature of vulnerability and access to natural resources (Sections 4.6.4, 4.7.5.3, 5.4.2.3, 5.5.2.6, 5.8.2.2; Cross-Chapter Box GENDER in Chapter 18) will influence the efficacy of interventions to prevent conflict or to build durable peace (Pearse, 2017; Chandra et al., 2017; Fröhlich et al., 2018). However, this understanding has not so far resulted in widespread employment of gender-led analyses (Fröhlich and Gioli, 2015). This represents a key opportunity for expansion of the solution space for climate-related conflict. Analysis of peace processes more generally demonstrates the benefits of women’s participation in peace processes for devising strategies for building peace (Paffenholz, 2018; Cárdenas and Olivius, 2021) and for the durability of that peace (Shair-Rosenfield and Wood, 2017; Krause et al., 2018).
7.4.6 Climate Resilient Development Pathways
Climate resilient development is a set of trajectories that strengthens sustainable development and efforts to eradicate poverty and reduce inequalities while promoting fair and equitable reductions of GHG emissions. Climate resilient development also serves to steer societies towards low-carbon, prosperous and ecologically safer futures (Chapter 1). All pathways to pursue climate resilient development will involve balancing complex synergies and trade-offs (very high confidence; Chapter 18). Pathways to climate resilient development can be pursued simultaneously with recovering from the COVID-19 pandemic (Cross-Chapter Box COVID in Chapter 7; Ebi et al., 2021).
Meeting commitments against the following seven existing global priorities would facilitate CRDPs and transformational futures for health, well-being, conflict and migration (high agreement, medium evidence):
- Fully implementing the WHO Operational Framework for building climate-resilient health systems (WHO, 2015b)
- Achieving Universal Health Coverage (UHC) under SDG 3 (good health and well-being)
- Achieving net zero GHG emissions from healthcare systems and services
- Achieving the SDGs more generally
- Adopting mitigation policies and technologies that have significant health co-benefits (see Cross-Chapter Box HEALTH)
- Meeting the objectives of the Global Compact for Safe, Orderly and Regular Migration
- Inclusive and integrative approaches to climate-resilient peace
These transformations map across all five of the system transitions identified in Chapter 18: energy systems; land, ocean, and ecosystems; urban and infrastructural systems; industrial systems; and societal systems.
7.4.7.1 Fully Implementing the World Health Organization Operational Framework
The WHO Operational Framework for building climate-resilient health systems was designed to increase the capacity of health systems and public health programming to protect health in an unstable and changing climate (WHO, 2015b). The guidance defines a climate-resilient health system as one that is capable to anticipate, respond to, cope with, recover from and adapt to climate-related shocks and stress, so as to bring sustained improvements in population health despite an unstable climate. Full implementation of this framework has the potential to achieve transformational adaptation; the fundamental attributes of health systems would change to anticipate and effectively manage the population health and healthcare risks of climate change. This includes having the knowledge, capacity, tools and human and financial resources for health systems to extend beyond soft limits to adaptation.
The WHO framework outlines 10 key components (Figure 7.15) that, when achieved, will:
- Guide professionals working in health systems and in health determining sectors (e.g., water and sanitation, food and agriculture, energy, and urban planning) to understand and effectively prepare for the additional health risks posed by climate variability and change
- Identify the main health functions that need to be strengthened to build climate resilience, and to use these to develop comprehensive and practical plans (e.g., the health component of National Adaptation Plans (H-NAP))
- Support health decision makers to identify roles and responsibilities to implement this plan for actors within and outside the formal health sector
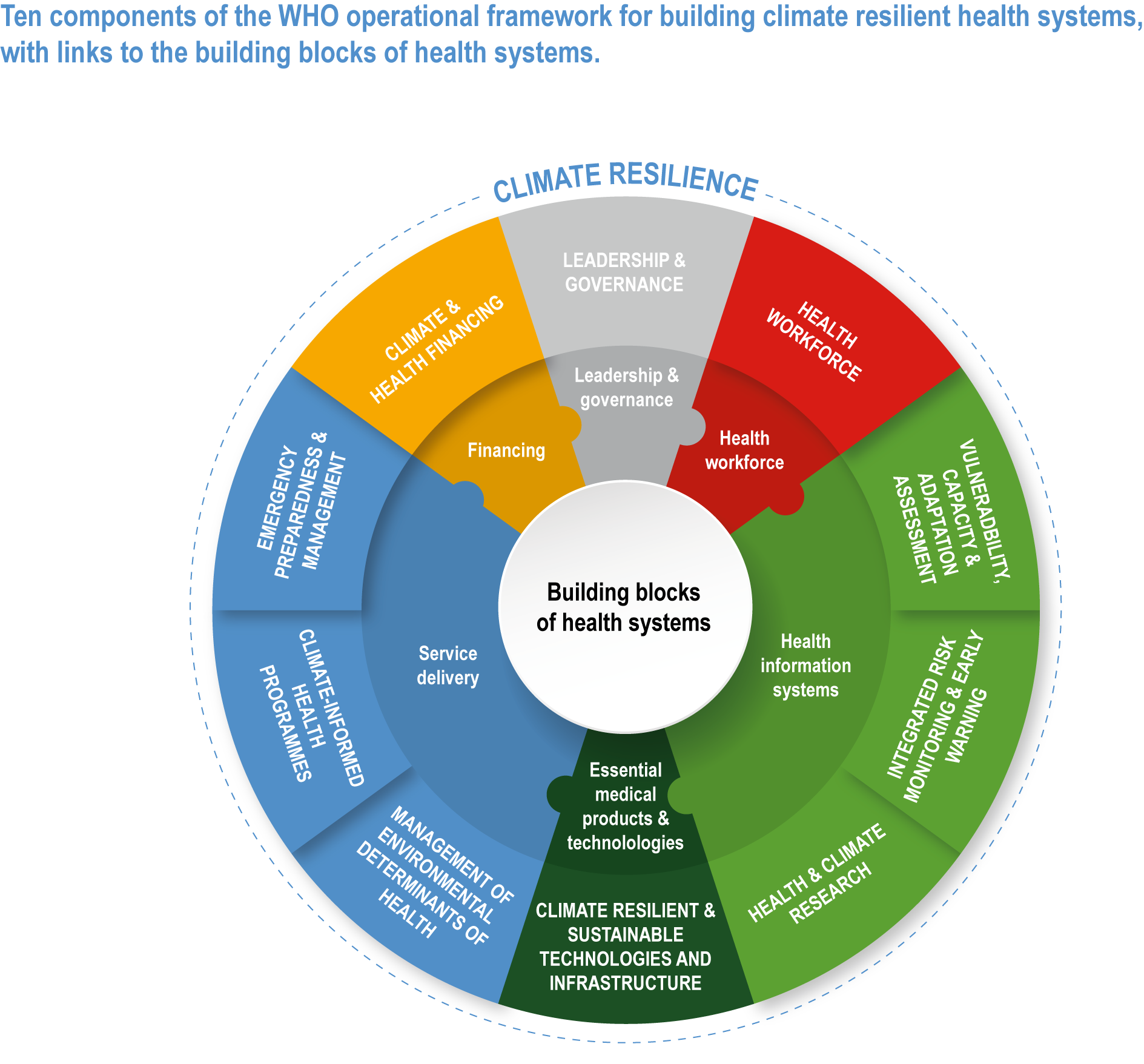
Figure 7.15 | Ten components of the WHO operational framework for building climate-resilient health systems with links to the building blocks of health systems. Source: WHO (2015b).
Achieving full implementation of the WHO Operational Framework requires determination and commitment—with associated funding—from the health community specifically and health-determining sectors more generally. Identifying priority areas is an immediate step required to commence this implementation process, which will vary across different contexts. Active engagement with Communities of Practice to share lessons and experiences would be a useful approach to support national and sub-national efforts; examples of this already exist (e.g., the Climate Change Community of Practice in Canada and the ‘weADAPT’ initiative under the auspices of the Stockholm Environment Institute).
Table 7.9 summarises selected characteristics of health systems as they might be under SSP1 (a world aiming to sustainable development), SSP2 (a world continuing current trends) and SSP3 (a world with high challenges to adaptation and mitigation), with systems under SSP1 being most consistent with climate resilient development. The table highlights the importance of investments that promote sustainable and resilient development to decrease vulnerability, no matter the magnitude and pattern of climate change. Adapting under SSP3 would be challenging even under pathways of limited additional climate change.
Table 7.9 | Characteristics of future health systems under three SSPs; modified from Sellers and Ebi (2017).
SSP3 | SSP2 | SSP1 | |
Basic characteristics | Reactive; failure to adapt; siloed information channels and national governance; limited partnerships | Incomplete planning; new information incorporated as convenient; occasional partnerships | Proactive; adaptively managed; frequent partnerships; inter-disciplinary |
Leadership and governance | Little focus at national and international levels on climate change and health; minimal planning conducted | Planning for climate change and health, but not comprehensive and often side-tracked by other issues | Strong climate change and health planning apparatus, including health components of national adaptation plans; regional/international partnerships |
Health workforce | Climate change and health not often incorporated into training; few provisions for new training programmes or funding for increase health worker positions in climate change-relevant specialties; health disparities not addressed | Climate change and health not systematically incorporated into training; new training programmes insufficient to fill gaps in demand; limited attention to addressing health disparities | Systematic inclusion of climate change and health in worker training; expansion of funding and training; financing and incentive mechanisms to address health disparities |
Health information systems | Assessments of vulnerability and adaptation rarely conducted, if ever; information not useful for planning; minimal risk monitoring or research | Vulnerability and adaptation assessments occasionally conducted, but generally of poor quality; early warnings incomplete; fiscal and political constraints on research | Vulnerability and adaptation assessments regularly conducted and used in planning; robust early warning networks; research agenda focused on vulnerable communities |
Climate-resilient and sustainable technologies and infrastructure | Facilities sited and constructed without climate consideration incorporated; medical supply chains not modified | Capital cost serves as a key factor in siting and construction; increasing vulnerability of facilities to shocks | Health infrastructure designed to be robust to storms/floods, with redundant systems added to ensure continuity of care |
Service delivery | Policies to manage environmental health hazards generally not followed; care practices not modified to accommodate climate information; few changes to emergency management procedures; health inequities worsen | Environmental health policies are not robust; marginal improvements in care practices; risk assessments and communication inadequate; no shift in health inequities | Policies to manage environmental health hazards regularly reviewed; practitioners review care practices and adjust as appropriate based on local climate and health conditions; robust communication tools developed; health service improvements reduce health inequities |
Climate and health financing | Few funds devoted to climate change and health activities, particularly in low- and middle-income countries; few if any financing partnerships between high-, low- and middle-income countries; very weak regional and international coordinating bodies due to funding constraints | High-income countries generally form robust financing mechanisms; fiscal pressures in low- and middle-income countries constrain their financing abilities; financial partnerships formed across countries, but financing often not robust; regional and international coordinating bodies receive inadequate funds | Robust funding streams for climate change and health; climate change and health activities receive continuing financial support; effective financing partnerships; regional and international coordinating bodies effectively funded |
Stress testing is an approach for evaluating the extent to which health systems are prepared for a future different from today (Ebi et al., 2018a). These desk-based exercises identify a desirable future outcome, such as successfully managing an extreme heatwave, flood or storm with characteristics outside the range of recent experiences. The exercises move beyond identifying likely challenges from hazardous exposures to specifying policies and measures that could be successful under a different climate and development pathway. The exercises consider socioeconomic and political factors that can influence the extent of health system vulnerability and other factors that can affect health system demands by impacting population health. Stress testing is designed to identify conditions under which it would be difficult for the health system to maintain its essential functions and to identify interventions that could maintain essential system functions despite climate-related shocks and stresses.
7.4.6.2 Achieving Universal Health Coverage Under SDG 3 (good health and well-being)
UHC is when all people have access to the health services they need, when and where they need them, without financial hardship (WHO, 2021b). Achieving UHC is one of the targets in the SDGs. However, climate change is threatening to undermine the achievement of UHC through negative health outcomes and healthcare system disruptions (Salas and Jha, 2019; Phillips et al., 2020; Kadandale et al., 2020; Roa et al., 2020). Climate change adaptation and UHC progress are closely linked to one another, as both may improve health and achieve health equity (Salas and Jha, 2019). Supporting UHC is key to securing population health under a changing climate as well as addressing structural inequalities (Roos et al., 2021; Aleksandrova, 2020; Phillips et al., 2020). Many regions of the world with the highest levels of vulnerability to the health impacts of climate change also have low levels of UHC; an integrated approach to UHC planning that incorporates climate change will have great benefits particularly in improving health equity (Salas and Jha, 2019).
The COVID-19 pandemic has shown some countries taking positive steps to achieving UHC. For example, Ireland nationalised healthcare for the duration of the pandemic and many countries, including Australia, have enhanced their telehealth services, which has enabled specific groups to access health services, particularly those in rural and remote settings, and has allowed continuous care to the community (Monaghesh and Hajizadeh, 2020; Cross-Chapter Box COVID in Chapter 7).
7.4.6.3 Achieving Net Zero GHG Emissions from Healthcare Systems and Services
The healthcare system is a core component of UHC, supporting climate-resilient and environmentally sustainable healthcare facilities (Corvalan et al., 2020). Health systems are large carbon polluters and have the potential to look beyond traditional ‘green’ initiatives towards a more fundamental, longer-term redesign of current service models, with health practitioners participating actively in this process (Charlesworth and Jamieson, 2018). In the largest and most comprehensive accounting of national healthcare service emissions, the UK’s National Health Service (NHS) quantified its health services’ emissions and identified that 62% came from the supply chain, 24% from the direct delivery of care, 10% from staff commute and patient and visitor travel, and 4% from private health and care services commissioned by the NHS (Tennison et al., 2021).
The health sector has considerable opportunity to reduce its own carbon footprint and by doing so would contribute to mitigation efforts and help reduce health burdens associated with GHG emissions (Vidal et al., 2014; Duane et al., 2019; Charlesworth and Jamieson, 2019; Charlesworth et al., 2018; Guetter et al., 2018; Bharara et al., 2018; Frumkin, 2018) (high confidence). The UK’s NHS has committed to becoming the world’s first net zero national healthcare system. Other examples of recent and ongoing initiatives include those undertaken by the Kaiser Permanente and the Gundersen Clinics in the USA, Health Care without Harm in the Asia Pacific region, and the Green Hospital Initiative in New Delhi (Frumkin, 2018; Bharara et al., 2018).
7.4.6.4 Achieving the SDGs Would Increase Resilience in Health-Determining Sectors and Contribute to Reducing the Risks of Involuntary Displacement and Conflict
The SDGs are globally agreed objectives that integrate the economic, environmental and social aspects of sustainable development to end poverty, protect nature and ensure that all people enjoy peace and prosperity. The SDGs were developed under the principle that the goals are integrated and indivisible, such that progress in one goal depends on progress in others (WHO, 2016b). Promoting health and well-being is not the sole responsibility of the health sector; it is also partially determined by strategies, policies and options such as poverty reduction, promoting gender equality, ensuring all people enjoy peace and prosperity, eliminating nutritional insecurity and ensuring availability and sustainable management of water and sanitation (Morton et al., 2019; Bennett et al., 2020). Unique themes in the SDGs for health policy and systems research include social protection, access to health services, stronger and more effective multi-sectoral collaborations beyond the health sector to address the upstream drivers of health and well-being, and participatory and accountable institutions to strengthen civic engagement and local accountability within health systems (Bennett et al., 2020).
For example, clean water, sanitation and hygiene are essential to human health and well-being. Unsafe water and sanitation and a lack of hygiene caused an estimated 870,000 associated deaths in 2016 (WHO, 2021c). Only 71% of the global population has access to safely managed drinking water services; only 45% of the global population has access to safely managed sanitation services; and 60% has basic handwashing facilities in their home. About 25% of healthcare facilities lack basic water services, exposing workers and patients to higher infection risks. More than 80% of countries reported in 2018 that they lacked sufficient funding to meet national WASH targets. As detailed in Section 7.2.2.2, Box 7.3, Section 7.3.1.4 and Section 7.4.2.3, the burden of climate-sensitive WBDs would be reduced if WASH targets were met.
WHO developed a Global Action Plan for Healthy Lives and Well-Being for All that brings together multi-lateral health, development and humanitarian agencies to support countries in accelerating progress towards the health-related SDGs (WHO, 2021c). Themes include sustainable financing to reduce unmet needs for services, community and civil society engagement to generate knowledge to inform policymaking and health responses, addressing the socioenvironmental determinants of health, ensuring health and humanitarian services are available in fragile and vulnerable settings, research and development, and greater implementation of digital health delivery. In 2020, enhanced collaboration through the Global Action Plan provided support for an equitable recovery from the COVID-19 pandemic in, for example, Lao People’s Democratic Republic, Pakistan, Tajikistan, Somalia, South Sudan, Malawi, Nepal and Columbia, highlighting the potential for multi-sectoral integration of economic, environmental and social aspects of sustainable development to maintain essential health services and core public health functions during shocks and stresses (WHO, 2021a).
Meeting the SDGs also contributes towards reducing involuntary displacement and conflict, as assessed in Sections 7.4.6.6 and 7.4.6.7.
7.4.6.5 Adopting Mitigation Policies and Technologies that Have Significant Health Co-benefits
Substantial co-benefits from climate action can result from investing in health systems, infrastructure, water and sanitation, clean energy, affordable healthy diets, low-carbon housing, public transport, improved air quality, and social protection. These benefits are in addition to the avoided health impacts associated with climate change (see Cross-Chapter Box HEALTH in Chapter 7).
7.4.6.6 International Policy Frameworks for Migration that Contribute to Climate Resilient Development
Climate-related migration, displacement and immobility in coming decades will coincide with global and regional demographic changes that will produce a widening distinction between high-income countries that have aging, slow-growing (or in some countries, shrinking) population numbers and low-income countries that have rapidly growing, youthful populations. Given this dynamic, coordinated national and international strategies that integrate migration and displacement considerations with wider adaptation and sustainable development policies may contribute to climate resilient development. Since AR5, the international community has established a number of agreements and initiatives that, with continued pursuit and implementation, would create potential for climate-related migration to be a positive contribution towards adaptive capacity-building and sustainable development more broadly (Warner, 2018).
The 2018 Global Compact for Safe, Orderly and Regular Migration provides an important opportunity for planning for and responding to future climate-related migration and displacement (Kälin, 2018). Among its 23 objectives, the Compact explicitly encourages the international community to implement migration policies that facilitate voluntary migration and actively prepare for involuntary displacements due to climate change, especially in low- and middle-income countries. The Compact’s objectives include reducing barriers to legal and safe migration, and facilitating the freer flow of remittances between sending and receiving communities. By doing so the Compact aims to increase the potential for migration to make positive contributions to sustainable development and to adaptive capacity-building. It also contains specific provisions pertaining to climate- and disaster-related migration and displacement. Objective 2 of the Compact aims at reducing drivers of involuntary or low-agency migration and recommends that states establish systems for sharing information on environmental migration, develop climate adaptation and resilience strategies harmonised at sub-regional and regional levels, and cooperate on disaster risk prevention and response. Other objectives in the Compact relevant to climate-related migration include Objective 5 (increasing pathways for regular migration) and Objective 19 (facilitating migrants’ ability to contribute to sustainable development). Objective 18, which links migration with skills development, is consistent with the ‘migration with dignity’ approach to displacement risks (McNamara, 2015; Kupferberg, 2021). The 2018 Global Compact on Refugees observes that climate hazards increasingly interact with the drivers of refugee movements. The guidelines this Compact provides to governments regarding actions for addressing the causes of refugee movements and considerations for assisting and supporting refugees are useful for governments seeking guidance for all forms of displacement more generally, including displacement linked to climate change.
Pursuant to the Paris Agreement, a task force was struck by the Warsaw International Mechanism to make recommendations to the Conference of the Parties to the UNFCCC on how to reduce the risks of climate-related displacement. Its 2018 report recommended that parties work towards development of national legislation, cooperate on research, strengthen preparedness, integrate mobility into wider adaptation plans, work towards safe and orderly migration, and provide assistance to people internally displaced for climate-related reasons. Such recommendations dovetail strongly with the objectives of the Compacts on Migration and Refugees as well as the Sendai Framework for DRR and the 2030 SDGs. The SDGs, which include multiple goals and targets in which migration plays an explicit role in fostering development (Nurse, 2019), may be seen as completing the international policy arrangements necessary for addressing future climate-related migration and displacement.
7.4.6.7 Inclusive and Integrative Approaches to Climate-Resilient Peace
CRDPs to reduce conflict risk rely on a shift in perspective from framings around resource scarcity and security to sustainable natural resource governance and peace (Brauch et al., 2016; Barnett, 2018; Dresse et al., 2018; Day and Caus, 2020). Recognising that conflict results from underlying vulnerabilities, development that reduces vulnerability offers the best win-win option for building sustainable, climate-resilient peace rather than specific security-focused interventions (high confidence). To this end, meeting the SDGs represents an unambiguous path to reducing conflict risk in a climate-changed world (Singh and Chudasama, 2021). There is growing acceptance in the development community, despite reservations about the securitisation of climate, that instability and conflict exacerbated by climate change has the potential to undermine development gains (Casado-Asensio et al., 2020; Day and Caus, 2020).
Core to achieving climate-resilient peace are new ways of working that involve cross-issue and cross-sectoral collaboration and integration as a default to policy and programming. The Security Council Resolution 1325 Women and peace and security (S/RES/1325 (2000)) and the Sustaining Peace Agenda (A/RES/70/262 (2016)) are notable examples of this. The 2020 UNEP report on gender and security recommends integrated policy frameworks, better financing to strengthen women’s roles in peacebuilding, integrated programme design, and further research on gender, climate and security linkages. Inclusive approaches recognise that much of the vulnerability that drives conflict risk is generated by existing inequality and marginalisation of large proportions of the population—for example women and youth—and that peace cannot be achieved without their needs being taken into account and without their participation in peace processes (Mosello et al., 2021). Diverse and inclusive partnerships also require ways to better engage local-level participation, and improve understanding of how to build consensus through human rights-based approaches that recognize non-violent conflict and protest to be potentially positive and constructive elements of transformational approaches to building resilience (Nursey-Bray, 2017; Ensor et al., 2018; Schipper et al., 2021). Addressing the lack of participation of researchers and experts from countries most at risk of conflict in many climate-related conflict and peacebuilding assessments and initiatives could also support this objective. There is an increasing focus on the role of environmental defenders in highlighting violations and gaps in state obligations through non-violent protest (Butt et al., 2019; Scheidel et al., 2020).
CRDPs for sustainable peace also require different ways of gathering intelligence and informing conflict risk. Dynamics that affect such risks exist across scales from the local to the regional, and require response in a transboundary manner. There is increasing emphasis on engaging local stakeholders and diverse partnerships to inform context appropriate measures and better policy coordination (Bremberg et al., 2019; Tshimanga et al., 2021; Abrahams, 2020). The UN’s Climate Security Mechanism, working across three UN departments, takes an integrated approach to analyse and support timely and appropriate responses to conflict risk, focusing on risk assessments and early warning systems to aid conflict prevention, climate-informed peace and security activities and conflict-sensitive development, and to promote inter-sectoral cooperation, partnership and information sharing (DPPA et al., 2020). There is already acknowledgement that adaptation needs to be effectively monitored so that maladaptation can be avoided (Eriksen et al., 2021). Here, academic research, which until now has predominantly focused on understanding the causal relationship between conflict and climate, could contribute to advancing the monitoring and evaluation of climate-resilient peacebuilding initiatives (Mach et al., 2020; Gilmore et al., 2018).
Cross-Chapter Box HEALTH | Co-benefits of Climate Actions for Human Health, Well-Being and Equity
Authors: Cristina Tirado (USA/Spain, Chapter 7); Robbert Biesbroek (Netherlands, Chapter 13); Mark Pelling (United Kingdom, Chapter 6); Jeremy Hess (USA, Chapter 7); Felix Creutzig (Germany, WGIII); Rachel Bezner Kerr (Canada/USA, Chapter 5); Siri Eriksen (Norway, Chapter 18); Diarmid Campbell-Lendrum (United Kingdom, Chapter 7); Elisabeth Gilmore (USA/Canada, Chapter 14); Maria Figueroa (Denmark/Venezuela, WGIII); Nathalie Hilmi (Monaco, Chapter 18); Peter Newman (Australia, WGIII); Sebastian Mirasgedis (Greece, WGIII); Sharma Rohit (India); Yamina Saheb (France/Algeria, WGIII); Gerardo Sanchez Martinez (Spain); Peter Smith (United Kingdom, WGIII); Adrian Leip (Italy, WGIII); Dhar Subash (Denmark/India, WGIII); Chris Trisos (South Africa, Chapter 9); Mercedes Bustamante (Brazil, WGIII); Luisa Cabeza (Spain, WGIII); Diana Urge-Vorsatz (Hungary, WGIII)
Achieving the Paris Agreement and SDGs can result in low-carbon, healthy, resilient and equitable societies with high well-being for all (very high confidence) (Alfredsson et al., 2018; O’Neill et al., 2018). Given the overlap in sources of greenhouse gases (GHGs) and co-pollutants in energy systems, strategies that pursue GHG emission reductions and improvements in energy efficiency hold significant potential health co-benefits through air pollution emission reductions (high confidence) (Gao et al., 2018). Air quality improvements alone can substantially offset, or most likely exceed, mitigation costs at the societal level (Schucht et al., 2015; Chang et al., 2017; Markandya et al., 2018; Vandyck et al., 2018; Peng et al., 2017; Woodward et al., 2019; Sampedro et al., 2020; Xie et al., 2018). Pursuit of a mitigation pathway compatible with warming of +1.5°C with associated cleaner air, avoided extreme events and improved food security and nutrition could result in 152 ± 43 million fewer premature deaths worldwide between 2020 and 2100 compared with a business-as-usual scenario (Shindell et al., 2018). Reaching the Paris Agreement could result in an annual reduction of 1.18 million air pollution-related deaths, 5.86 million diet-related deaths and 1.15 million deaths due to physical inactivity across nine major economies by 2040 (Hamilton et al., 2021). In Europe, a mitigation scenario compatible with RCP2.6 could reduce total pollution costs, mostly from PM2.5, by 84%, with human health benefits equal to more than Euro 1 trillion over five years (Scasny et al., 2015). In the EU, ambitious climate mitigation policies could reduce years of lost life due to fine particulate matter (PM) from over 4.6 million in 2005 to 1 million in 2050, reduce ozone-related premature deaths from 48,000 to 7,000 and generate health benefits of Euro 62 billion yr –1 in 2050 (Schucht et al., 2015).
However, there may be significant trade-offs between mitigation and other societal goals (Dong et al., 2019; Gao et al., 2018). In some scenarios, mitigation policies consistent with the NDCs may slow poverty reduction efforts (Campagnolo and Davide, 2019) with implications for health. A framework of ‘co-impacts’ that assumes neither a general beneficial nature of all implications from mitigation policy nor a hierarchy between climate and other types of benefits, may be more appropriate (Ürge-Vorsatz et al., 2014; Cohen et al., 2017).
Transitioning to affordable clean energy sources for all presents opportunities for substantial well-being, health, and equity co-benefits (high confidence) (Gibon et al., 2017; Lacey et al., 2017; Peng et al., 2018; Vandyck et al., 2018; Williams et al., 2018). Residential solid fuel use affects health and degrades indoor air quality for up to 3.1 billion people in low- and middle-income countries (WHO, 2016b; Wang et al., 2017 a). Adherence to planned emission reductions from the Paris Agreement related to renewables could subsequently improve air quality and prevent 71,000–99,000 premature deaths annually by 2030 (Vandyck et al., 2018). This effect increases with a 2°C pathway, with 0.7–1.5 million premature deaths avoided annually by 2050 (Vandyck et al., 2018). Co-benefits are also observed at national and regional levels. For instance, China could expect 55,000–69,000 averted deaths in 2030 if it transitioned to a half-decarbonised power supply for its residential and vehicle sectors (Peng et al., 2018).
Investing in universal basic infrastructure, including sanitation, clean drinking water, drainage, electricity, and land-rights, can transform development opportunities, increase adaptive capacity, and reduce vulnerability to climate-related risks (high agreement, high evidence).Transformative approaches that reduce climate-related risks and deliver enhanced social inclusion and development opportunities for the urban poor are most likely where local governments act in partnership with local communities and other civil society actors (high confidence) (Chapter 6, sections 6.1, 6.3, 6.4).
Rapid urbanisation offers a time-limited opportunity to work at scale towards transformational adaptation and climate resilient development (medium evidence, high agreement). Multi-level leadership, institutional capacity and financial resources to support inclusive adaptation in the context of multiple pressures and inter-connected risks can help ensure that the additional 2.5 billion people projected to live in urban areas by 2050 are less exposed to climate-related hazards and contribute less to global warming (high confidence) (Chapter 6, sections 6.1, 6.3, 6.4). Integrating low-carbon, inclusive adaptation into infrastructure investment driven by rapid urban population growth and COVID-19 recovery can accelerate co-benefits (Chapter 6).
Urban planning that combines clean, affordable public transportation, shared clean vehicles and accessible active transportation modes can improve air quality and contribute to healthy, equitable societies and higher well-being for all. Stimulating active mobility (walking and bicycling) can bring physical and mental health benefits (high confidence) (Chapter 6; Rojas-Rueda et al., 2016; Avila-Palencia et al., 2018; Gascon et al., 2019; Hamilton et al., 2021). The health gains from active mobility outweigh traffic-related injuries due to a decreased incidence of chronic diseases (Ahmad et al., 2017; Maizlish et al., 2017; Tainio et al., 2017; Woodcock et al., 2018).
Urban green and blue spaces contribute to climate change adaptation and mitigation and improve physical and mental health and well-being (high confidence) (Hansen 2017; EC, 2018; WHO, 2018a; Rojas-Rueda et al. 2019; 13.7.3, WGII; 6. WGII; 8.4 WGIII). Urban green infrastructure including urban gardens, can bring benefits to social cohesion, mental health and well-being and reduce the health impacts of heatwaves by decreasing temperatures, thus reducing inequities in exposure to heat stress for low income, marginalised groups (Hoffman et al., 2020; Hoffmann et al., 2020; Chapter 5 section 5.12.5; Chapter 6; Chapter 7 section 7.4; Chapter 13 section 13.7). The trade-offs of increasing urban green and blue spaces include potential public health risks related to increased vectors or hosts for infectious diseases, toxic algal blooms, drowning and aeroallergens (Choi et al., 2021; Stewart-Sinclair et al., 2020; Chapter 6).
Climate adaptation and mitigation policies in the building sector offer multiple well-being and health co-benefits (high confidence) (Diaz-Mendez et al., 2018; Macnaughton et al., 2018; Chpater 3 section 3.6.2). Leadership in Energy and Environmental Design (LEED) certified buildings in the USA, Brazil, China, India, Germany and Turkey saved an estimated USD 7.5 billion in energy costs and averted 33 Mt of CO2 from 2000–2016 (Macnaughton et al., 2018). These measures can increase health benefits through better indoor air quality, reduction of the heat island effect, improved social well-being through energy poverty alleviation, creation of new jobs, increased productive time and income, increased thermal comfort and lighting indoors and reduced noise impact (Smith et al., 2016; McCollum et al., 2018; Thema et al., 2017; Mirasgedis et al., 2014; Alawneh et al., 2019; Diaz-Mendez et al., 2018). The value of these multiple co-benefits associated with climate actions in buildings is equal to or greater than the costs of energy savings (Ürge-Vorsatz et al., 2016; Payne et al., 2015; Chapter 14 section 14.4.5).
Shifting to sustainable food systems that provide affordable, diverse and plant-rich diets with moderate quantities of GHG-intensive animal protein can bring health co-benefits and substantially reduce GHG emissions, especially in high income countries and where ill health related to overconsumption of animal-based products is prevalent (very high confidence) (Chapter 5 section 5.12.6; Chapter 7 section 7.4, Chapter 13 section 13.5; Springmann et al., 2018c; IPCC, 2019b; Clark and Tilman, 2017; Poore and Nemecek, 2018; Hayek et al., 2021). Transforming the food system by limiting the demand for GHG-intensive animal foods, reducing food over-consumption and transitioning to nutritious, plant-rich diets can have significant co-benefits to health (high confidence) (Hedenus et al., 2014; Ripple et al., 2014; Tirado, 2017; Springmann et al., 2018c; IPCC, 2018; IPCC, 2019a; IPCC, 2019b; Nelson et al., 2016; Willett et al., 2019; Tilman and Clark, 2014; Green et al., 2015; Springmann et al., 2016b; Springmann et al., 2018b; Springmann et al., 2018a; Springmann et al., 2018c; Milner et al., 2015; Milner et al., 2017; Farchi et al., 2017; Song et al., 2017; Willett et al., 2019). Reduction of red meat consumption reduces the risk of cardiovascular disease (CVD) and colorectal cancer; the consumption of more fruits and vegetables can reduce the risk of CVD, type II diabetes, cancer and all causes of mortality (Tilman and Clark, 2014; Sabate and Soret, 2014; Willett et al., 2019; Chapter 7 section 7.4; Chapter 5 section 5.12.5). Globally, it is estimated that transitioning to more plant-based diets—in line with World Health Organization (WHO) recommendations on healthy eating—could reduce global mortality by 6‒10% and food-related GHG emissions by 29‒70% by 2050 (Springmann et al., 2016b). There are limitations in accessibility of affordable of healthy and diverse diets for all (Springmann et al., 2020) and trade-offs such as the potential increase of GHG emissions from producing healthy and diverse diets in low- and medium-income countries (Semba et al., 2020). Agroecological approaches have mitigation and adaptation potential and deliver ecosystem services, biodiversity, livelihoods and benefits to nutrition, health and equity (Rosenstock et al., 2019; Bezner Kerr et al., 2021; Chapter 5 sections 5.4.4, 5.14.1; Chapter 13 section 13.5; Chapter 14 section 14.4.4).
Frequently Asked Questions
FAQ 7.1 | How will climate change affect physical and mental health and well-being?
Climate change will affect human health and well-being in a variety of direct and indirect ways that depend on exposure to hazards and vulnerabilities that are heterogeneous and vary within societies, and that are influenced by social, economic and geographical factors and individual differences (see Figure FAQ7.1.1). Changes in the magnitude, frequency and intensity of extreme climate events (e.g., storms, floods, wildfires, heatwaves and dust storms) will expose people to increased risks of climate-sensitive illnesses and injuries and, in the worst cases, higher mortality rates. Increased risks for mental health and well-being are associated with changes caused by the impacts of climate change on climate-sensitive health outcomes and systems (see Figure FAQ7.1.2). Higher temperatures and changing geographical and seasonal precipitation patterns will facilitate the spread of mosquito- and tick-borne diseases, such as Lyme disease and dengue fever, and water- and food-borne diseases. An increase in the frequency of extreme heat events will exacerbate health risks associated with cardiovascular disease and affect access to freshwater in multiple regions, impairing agricultural productivity and increasing food insecurity, undernutrition and poverty in low-income areas.
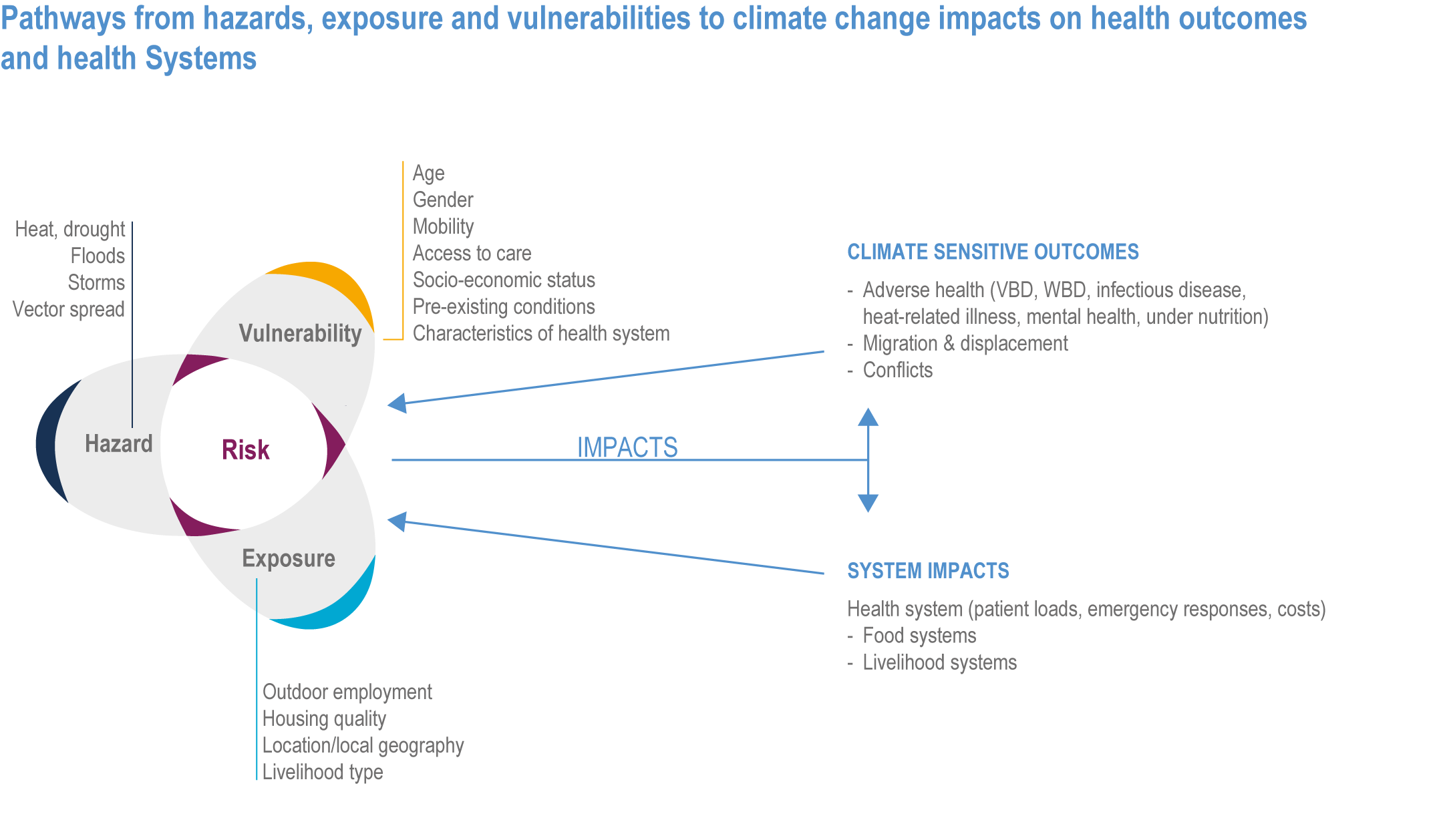
Figure FAQ7.1.1 | Pathways from hazards, exposure and vulnerabilities to climate change impacts on health outcomes and health systems.
WBD: waterborne disease, VBD: Vector-borne disease, and FBD: Food-borne disease.
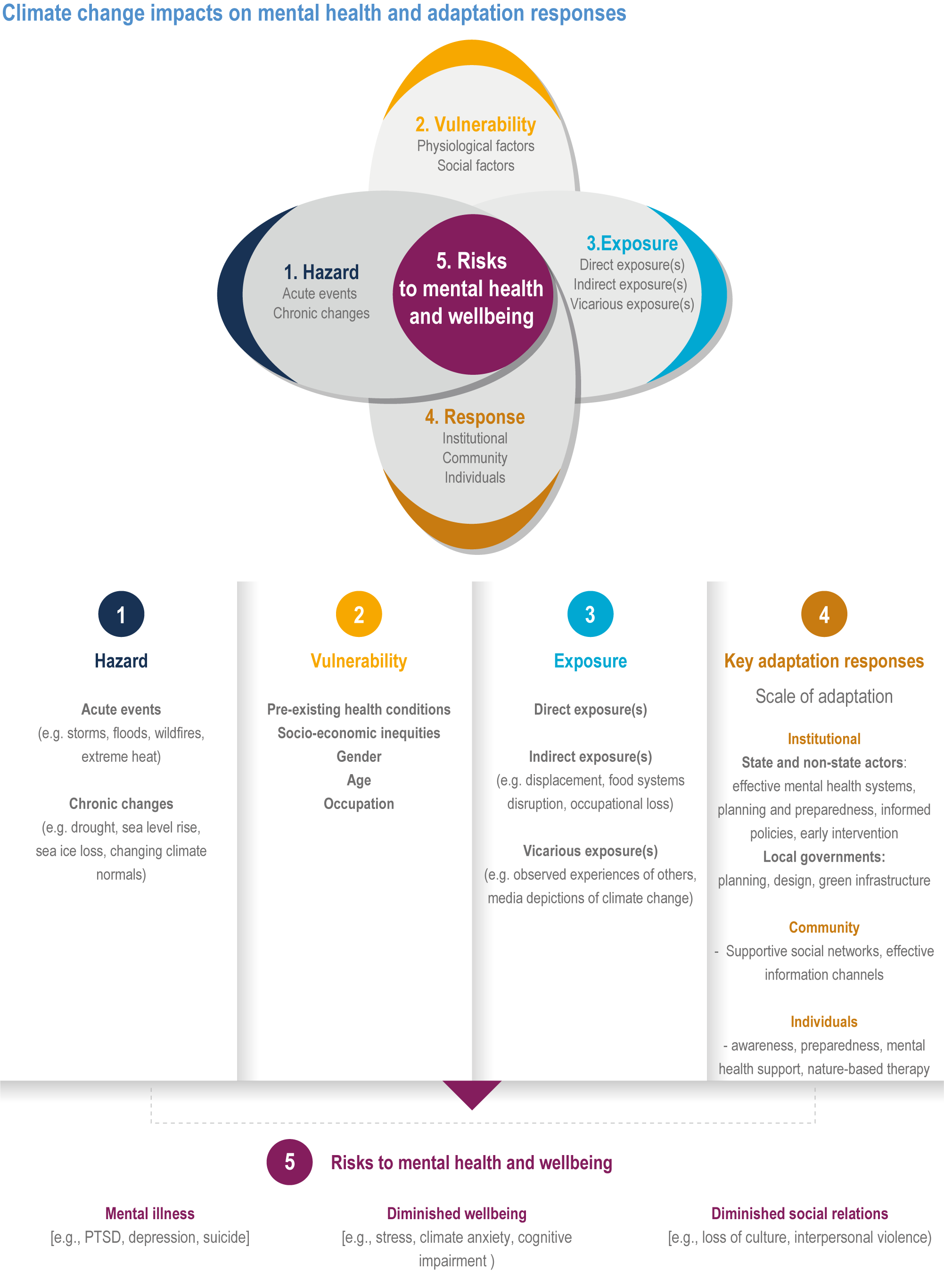
Figure FAQ7.1.2 | Climate change impacts on mental health and key adaptation responses. PTSD: Post traumatic stress disorder.
FAQ 7.2 | Will climate change lead to wide-scale forced migration and involuntary displacement?
Climate change will have impacts on future migration patterns that will vary by region and over time, depending on the types of climate risks people are exposed to, their vulnerability to those risks and their capacity—and the capacity of their governments—to adapt and respond. Depending on the range of adaptation options available, households may use migration as a strategy to adapt to climate risks, often through labour migration. The most common drivers of climate-related displacement are extreme weather events, floods and droughts, especially when these events cause severe damage to homes, livelihoods and food systems. Rising sea levels will present a new risk for communities situated in low-lying coastal areas and small island states. The greater the scale of future warming and extreme events, the greater the potential scale of future, involuntary climate-related migration and displacement.Progress towards achieving the Sustainable Development Goals (SDGs) has strong potential to reduce future involuntary climate-related migration and displacement.
FAQ 7.3 | Will climate change increase the potential for violent conflict?
Climate hazards have affected armed conflict within countries but the observed influence of climate is small relative to socioeconomic, political and cultural factors. Adverse impacts of climate change threaten to increase poverty and inequality, undermine progress in meetings Sustainable Development Goals (SDGs) and place strain on civil institutions—all of which are factors that contribute to the emergence or worsening of civil unrest and conflict. Climate change impacts on crop productivity and water availability can function as a ‘risk multiplier’ for conflict in areas that are already politically and/or socially fragile and, depending on circumstances, could increase the length or the nature of an existing conflict. Institutional initiatives within or between states to protect the environment and manage natural resources can serve simultaneously as mechanisms for engaging rival groups and adversaries to cooperate in policymaking and peacebuilding.
FAQ 7.4 | What solutions can effectively reduce climate change risks to health, well-being, forced migration and conflict?
The solution space includes policies, strategies and programmes that consider why, how, when and who should be involved to sustainably adapt to climate change. Effectively preparing for and managing the health risks of climate change requires considering the multiple interacting sectors that affect population health and effective functioning of health systems. Considering the close inter-connections between health, migration and conflict, interventions that address climate risks in one area often have synergistic benefits in others. For example, conflicts often result in large numbers of people being involuntarily displaced and facilitate the spread of climate-sensitive diseases; tackling the underlying causes of vulnerability and exposure that generate conflict reduces risks across all areas. A key starting point for health and well-being is strengthening public health systems so that they become more climate resilient, which also requires cooperation with other sectors (water, food, sanitation, transportation, etc.) to ensure appropriate funding and progress on sustainable development goals. Interventions to enhance protection against specific climate-sensitive health risks could reduce morbidity and mortality and prevent many losses and damages (Figure FAQ7.4.1). These range from malaria net initiatives, vector control programmes, health hazard (syndromic) surveillance and early warning systems, improving access to water, sanitation and hygiene (WASH), heat action plans (HAPs), behavioural changes and integration with disaster risk reduction (DRR) and response strategies. More importantly, climate resilient development pathways (CRDPs) are essential to improve overall health and well-being, reduce underlying causes of vulnerability and provide a framework for prioritising mitigation and adaptation options that support sustainable development. Transformative changes in key sectors including water, food, energy, transportation and built environments offer significant co-benefits for health.
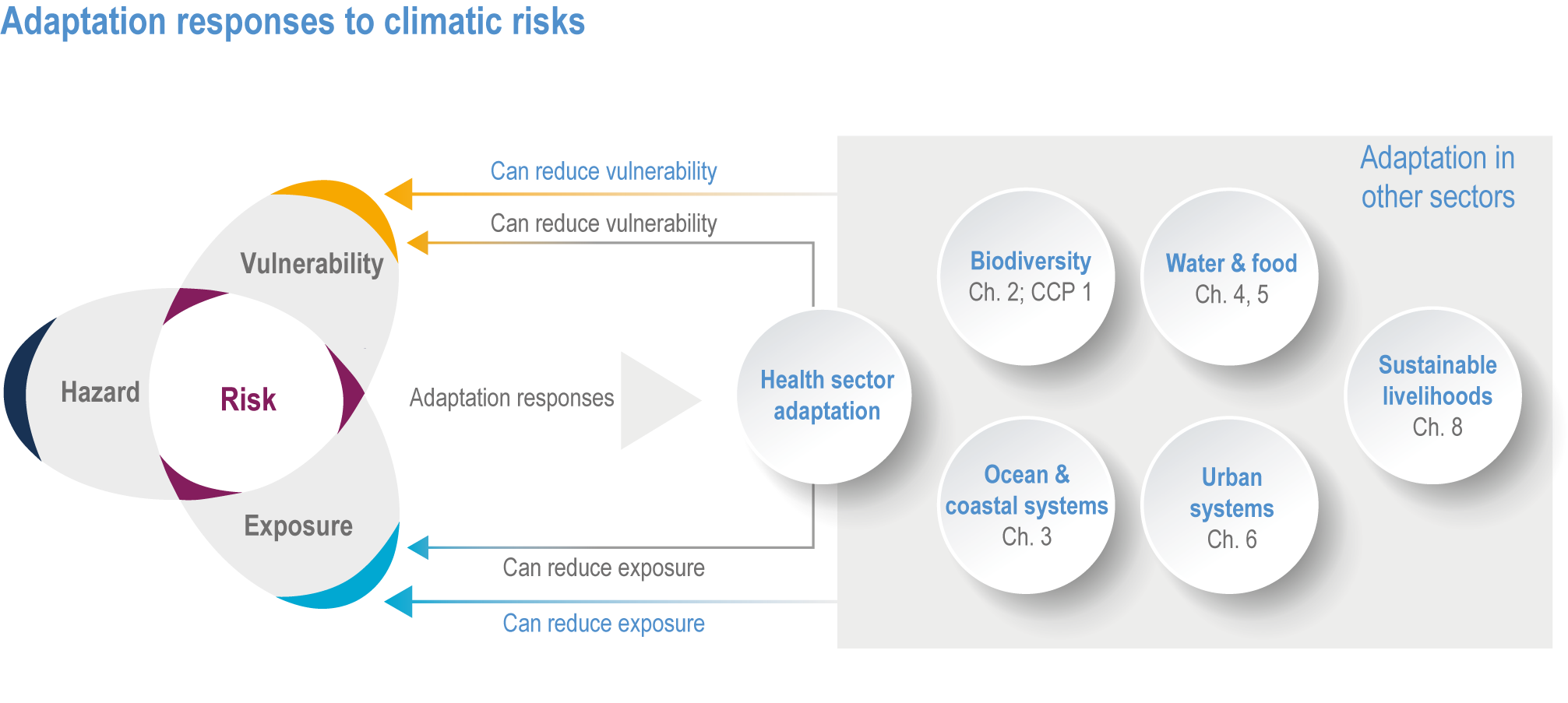
Figure FAQ7.4.1 | Solution space for adaptation to climate change in health and other sectors.
FAQ 7.5 | What are some specific examples of actions taken in other sectors that reduce climate change risks in the health sector?
Many actions taken in other sectors to address the risks of climate change can lead to benefits for health and well-being. Adaptive urban design that provides greater access to green and natural spaces simultaneously enhances biodiversity, improves air quality and moderates the hydrological cycle; it also helps reduce health risks associated with heat stress and respiratory illnesses, and mitigates mental health challenges associated with congested urban living. Transitioning away from internal-combustion vehicles and fossil fuel-powered generating stations to renewable energy mitigates greenhouse gas emissions, improves air quality and lowers the risks of respiratory illnesses. Policies and designs that facilitate active urban transport (walking and bicycling) increase efficiency in that sector, reduce emissions, improve air quality and generate physical and mental health benefits for residents. Improved building and urban design that foster energy efficiency improve indoor air quality and reduce risks of heat stress and respiratory illness. Food systems that emphasise healthy, plant-centred diets reduce emissions in the agricultural sector while helping in the fight against malnutrition.
Acknowledgements
The Lead Autors wish to recognize with thanks the research assistance and editorial assistance provided by Alyssa Gatt and Edi Cadham of Wilfrid Laurier University (Canada).
References
Alava, J. J., W. W. Cheung, P. S. Ross and , U. R. Sumaila, 2017: Climate change–contaminant interactions in marine food webs: toward a conceptual framework. Glob. Change Biol. , 23, 3984–4001, doi:10.1111/gcb.13667.Call, M. A., C. Gray, M. Yunus and M. Emch, 2017: Disruption, not displacement: environmental variability and temporary migration in Bangladesh. Glob. Environ. Change, 46, 157–165.
Abbott, M., M. Bazilian, D. Egel and H.H. Willis, 2017: Examining the food–energy–water and conflict nexus. Curr. Opin. Chem. Eng. , 18, 55–60.
Abdullah, A.S.M., et al., 2019: Effects of climate change and maternal morality: perspective from case studies in rural Bangladesh. Int. J. Environ. Res. Public Health, 16(23), 4594;https://doi.org/10.3390/ijerph16234594
Abel, D.W., et al., 2018: Air-quality-related health impacts from climate change and from adaptation of cooling demand for buildings in the eastern United States: an interdisciplinary modeling study. PLoS Med, 15 (7), doi:10.1371/journal.pmed.1002599.
Abel, G. and N. Sander, 2014: Quantifying global international migration flows. Science, 343 (6178), 1520–1522, doi:10.1126/science.1248676.
Abel, G.J., B. Barakat, K.C. Samir and W. Lutz, 2016: Meeting the sustainable development goals leads to lower world population growth. Proc. Natl. Acad. Sci. , 113 (50), 14294–14299.
Abel, G.J., M. Brottrager, J.C. Cuaresma and R. Muttarak, 2019: Climate, conflict and forced migration. Glob. Environ. Change, 54, 239–249.
Abhijith, K.V., et al., 2017: Air pollution abatement performances of green infrastructure in open road and built-up street canyon environments – a review. Atmos. Environ. , 162, 71–86, doi:10.1016/j.atmosenv.2017.05.014.
Abiona, O., 2017: Adverse effects of early life extreme precipitation shocks on short-term health and adulthood welfare outcomes. Rev. Dev. Econ. , 21 (4), 1229–1254.
Aboubakri, O., et al., 2020: Projection of mortality attributed to heat and cold; the impact of climate change in a dry region of Iran, Kerman. Sci. Total Environ. , 728, 138700, doi:10.1016/j.scitotenv.2020.138700.
Abrahams, D., 2020: Conflict in abundance and peacebuilding in scarcity: challenges and opportunities in addressing climate change and conflict. World Dev. , 132, 104998.
Abramson, M., et al., 2015: The resilience activation framework: a conceptual model of how access to social resources promotes adaptation and rapid recovery in post-disaster settings. J. Behav. Health Serv. Res. , 42 (1), 42–57.
Achakulwisut, P., et al., 2019: Effects of increasing aridity on ambient dust and public health in the U.S. southwest under climate change. Geohealth, 3 (5), 127–144, doi:10.1029/2019gh000187.
Achakulwisut, P., L.J. Mickley and S.C. Anenberg, 2018: Drought-sensitivity of fine dust in the US southwest: implications for air quality and public health under future climate change. Environ. Res. Lett. , 13 (5), 54025, doi:10.1088/1748-9326/aabf20.
Acharya, B.K., et al., 2018: Present and future of dengue fever in Nepal: mapping climatic suitability by ecological niche model. Int. J. Environ. Res. Public Health, 15 (2), doi:10.3390/ijerph15020187.
Acharya, Y., et al., 2019: Nutritional status, cognitive achievement, and educational attainment of children aged 8–11 in rural South India. PLoS ONE, 14 (10), doi:10.1371/journal.pone.0223001.
Achebak, H., D. Devolder, V. Ingole and J. Ballester, 2020: Reversal of the seasonality of temperature-attributable mortality from respiratory diseases in Spain. Nat. Commun. , 11 (1), doi:10.1038/s41467-020-16273-x.
Adams, C., T. Ide, J. Barnett and A. Detges, 2018: Sampling bias in climate-conflict research. Nat. Clim. Change, 8 (3), 200–203, doi:10.1038/s41558-018-0068-2.
Adams, H., 2016: Why populations persist: mobility, place attachment and climate change. Popul. Environ. , 37 (4), 429–448.
Adams, H. and S. Kay, 2019: Migration as a human affair: Integrating individual stress thresholds into quantitative models of climate migration. Environ. Sci. Policy, 93, 129–138, doi:10.1016/j.envsci.2018.10.015.
Adams, W.M. and J.F. Jardine, 2020: Overview of exertional heat illness. In: Exertional Heat Illness: a Clinical and Evidence-Based Guide, pp. 1–16. doi:10.1007/978-3-030-27805-2_1.
Adelodun, B., et al., 2020: Snowballing transmission of COVID-19 (SARS-CoV-2) through wastewater: any sustainable preventive measures to curtail the scourge in low-income countries?Sci. Total Environ. , 742, doi:10.1016/j.scitotenv.2020.140680.
Adelphi & Chemonics International 2020: Pathways to Peace: Addressing Conflict and Strengthening Stability in a Changing Climate. Lessons Learned from Resilience and Peacebuilding Programs in the Horn of Africa. Adaptation Thought Leadership and Assessments (ATLAS), United States Agency for International Development.
Adger, W., et al., 2015: Focus on environmental risks and migration: causes and consequence. Environ. Res. Lett. , 10, 60201, doi:10.1088/1748-9326/10/6/060201.
Adhvaryu, A., J. Fenske and A. Nyshadham, 2019: Early life circumstance and adult mental health. J. Polit. Econ. , 127 (4), 1516-1549.
Afifi, T., et al., 2016: Human mobility in response to rainfall variability: opportunities for migration as a successful adaptation strategy in eight case studies. Migr. Dev. , 5, 254–274.
Afriyie, K., J. Ganle and E. Santos, 2018: ‘The floods came and we lost everything’: weather extremes and households’ asset vulnerability and adaptation in rural Ghana. Clim. Dev. , 10 (3), 259–274, doi:10.1080/17565529.2017.1291403.
Afshin, A., et al., 2019: Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet , 393 (10184), 1958–1972, doi:10.1016/S0140-6736(19)30041-8.
Ahmad, S., S. Pachauri and F. Creutzig, 2017: Synergies and trade-offs between energy-efficient urbanization and health. Env. Res. Lett., 12 (11), doi:10.1088/1748-9326/aa9281.
Ahmadalipour, A. and H. Moradkhani, 2018: Escalating heat-stress mortality risk due to global warming in the Middle East and North Africa (MENA). Environ. Int. , 117, 215–225, doi:10.1016/j.envint.2018.05.014.
Ahmed, K.J., S.M. A. Haq and F. Bartiaux, 2019: The nexus between extreme weather events, sexual violence, and early marriage: a study of vulnerable populations in Bangladesh. Popul. Environ. , 40 (3), 303–324.
Ahmed, S., et al., 2020: Effect of extreme weather events on injury, disability, and death in Bangladesh. Clim Dev, 13 (4), 306-317.
Ahmed, S.A., M. Guerrero Flórez and P. Karanis, 2018: The impact of water crises and climate changes on the transmission of protozoan parasites in Africa. Pathog. Glob. Health, 112 (6), 281–293.
Ahmed, S.A., A. Saad-Hussein, A. El Feel and M. A. Hamed, 2014: Time series trend of bilharzial bladder cancer in Egypt and its relation to climate change: a study from 1995–2005. Int. J. Pharm. Clin. Res. , 6 (1), 46–53.
Aik, J., et al., 2018: Climate variability and salmonellosis in Singapore – a time series analysis. Sci. Total Environ. , 639, 1261–1267, doi:10.1016/j.scitotenv.2018.05.254.
Aitsi-Selmi, A. and V. Murray, 2016: Protecting the health and well-being of populations from disasters: health and health care in the Sendai framework for disaster risk reduction 2015–2030. Prehosp. Disaster Med. , 31 (1), 74–78, doi:10.1017/S1049023X15005531.
Aitsi-Selmi, A., et al., 2015: The Sendai Framework for disaster risk reduction: renewing the global commitment to people’s resilience, health, and well-being. Int. J. Disaster Risk Sci. , 6 (2), 164–176, doi:10.1007/s13753-015-0050-9.
Ajibade, I., M. Sullivan and M. Haeffner, 2020: Why climate migration is not managed retreat: six justifications. Glob. Environ. Change, 65, 102187.
Akande, V., T. Fawehinmi, R. Ruiter and S. Kremers, 2021: Healthy dietary choices and physical activity participation in the Canadian arctic: understanding Nunavut Inuit perspectives on the barriers and enablers. Int. J. Environ. Res. Public Health, 18 (3), doi:10.3390/ijerph18030940.
Akil, L., H.A. Ahmad and R.S. Reddy, 2014: Effects of climate change on Salmonella infections. Foodborne Pathog. Dis. , 11 (12), 974–980, doi:10.1089/fpd.2014.1802.
Akompab, D., et al., 2013: Heat waves and climate change: applying the health belief model to identify predictors of risk perception and adaptive behaviours in Adelaide, Australia. Int. J. Environ. Res. Public Health, 10 (6), 2164–2184, doi:10.3390/ijerph10062164.
Akpan, G., K. Adepoju, O. Oladosu and S. Adelabu, 2018: Dominant malaria vector species in Nigeria: modelling potential distribution of Anopheles gambiae sensu lato and its siblings with MaxEnt. PLoS ONE, 13 (10), doi:10.1371/journal.pone.0204233.
Akter, R., et al., 2017: Joint effects of climate variability and socioecological factors on dengue transmission: epidemiological evidence. Trop. Med. Int. Health, 22 (6), 656–669, doi:10.1111/tmi.12868.
Al-Bouwarthan, M., M.M. Quinn, D. Kriebel and D.H. Wegman, 2020: Risk of kidney injury among construction workers exposed to heat stress: a longitudinal study from Saudi Arabia. Int. J. Environ. Res. Public Health, 17 (11), doi:10.3390/ijerph17113775.
Alawneh, R., F. Ghazali, H. Ali and M. Asif, 2019: A new index for assessing the contribution of energy efficiency in LEED 2009 certified green buildings to achieving UN sustainable development goals in Jordan. Int. J. Green Energy, 16 (6), 490–499, doi:10.1080/15435075.2019.1584104.
Albert, S., et al., 2018: Heading for the hills: climate-driven community relocations in the Solomon Islands and Alaska provide insight for a 1.5°C future. Reg. Environ. Change, 2261–2272, doi:10.1007/s10113-017-1256-8.
Albrecht, G., et al., 2007: Solastalgia: the distress caused by environmental change. Australas. Psychiatry, 15, S95–S98, doi:10.1080/10398560701701288.
Alderman, H., 2016: Leveraging Social Protection Programs for Improved Nutrition: Summary of Evidence Prepared for the Global Forum on Nutrition-Sensitive Social Protection Programs, 2015. World Bank, Washington, DC.
Aleksandrova, M., 2020: Principles and considerations for mainstreaming climate change risk into national social protection frameworks in developing countries. Clim. Dev. , 12 (6), 511–520, doi:10.1080/17565529.2019.1642180.
Alele, F., B. Malau-Aduli, A. Malau-Aduli and M. Crowe, 2020: Systematic review of gender differences in the epidemiology and risk factors of exertional heat illness and heat tolerance in the armed forces. BMJ Open, 10 (4), doi:10.1136/bmjopen-2019-031825.
Alexander, P.J., R. Fealy and G.M. Mills, 2016: Simulating the impact of urban development pathways on the local climate: a scenario-based analysis in the greater Dublin region, Ireland. Landsc. Urban Plan. , 152, 72–89, doi:10.1016/j.landurbplan.2016.02.006.
Alfredsson, E., et al., 2018: Why achieving the Paris Agreement requires reduced overall consumption and production. Sustain. Sci. Pract. Policy, 14 (1), 1–5.
Ali, S., et al., 2020: Mental health in the Pacific: urgency and opportunity. Asia Pac. Viewp. , doi:10.1111/apv.12286.
Almendra, R., et al., 2019: Short-term impacts of air temperature on hospitalizations for mental disorders in Lisbon. Sci. Total Environ. , 647, 127–133, doi:10.1016/j.scitotenv.2018.07.337.
Alpino, T.A., A.R.M. d. Sena and C.M. d. Freitas, 2016: Desastres relacionados à seca e saúde coletiva – uma revisão da literatura científica. Ciên. Saúde Colet. , 21 (3), 809–820, doi:10.1590/1413-81232015213.21392015.
Alston, M. and B. Akhter, 2016: Gender and food security in Bangladesh: the impact of climate change. Gend. Place Cult. , 23 (10), 1450–1464, doi:10.1080/0966369x.2016.1204997.
Altieri, M., C. Nicholls, A. Henao and M. Lana, 2015: Agroecology and the design of climate change-resilient farming systems. Agron. Sustain. Dev. , 35 (3), 869–890, doi:10.1007/s13593-015-0285-2.
Amaratunga, D., et al., 2018: Sound practices of disaster risk reduction at local level. Procedia Eng. , 212, 1163–1170, doi:10.1016/j.proeng.2018.01.150.
Amat, F., et al., 2020: Pandemics meet democracy: experimental evidence from the COVID-19 crisis in Spain. SOC Arxiv Pap. , doi:10.31235/osf.io/dkusw.
Amegah, A.K., G. Rezza and J.J. Jaakkola, 2016: Temperature-related morbidity and mortality in Sub-Saharan Africa: a systematic review of the empirical evidence. Environ. Int. , 91, 133–149, doi:10.1016/j.envint.2016.02.027.
Amstislavski, P., et al., 2013: Effects of increase in temperature and open water on transmigration and access to health care by the Nenets reindeer herders in northern Russia. Int. J. Circumpolar Health, 72, 447–455, doi:10.3402/ijch.v72i0.21183.
An, R., M. Ji and S. Zhang, 2018: Global warming and obesity: a systematic review. Obes. Rev. , 19 (2), 150–163, doi:10.1111/obr.12624.
Analitis, A., et al., 2014: Effects of heat waves on mortality effect modification and confounding by air pollutants. Epidemiology, 25 (1), 15–22, doi:10.1097/EDE.0b013e31828ac01b.
Andersen, L.K. and M.D.P. Davis, 2017: A wake-up call to dermatologists – climate change affects the skin. Int. J. Dermatol. , 56 (10), e198–e199, doi:10.1111/ijd.13617.
Anderson, G.B., K.W. Oleson, B. Jones and R.D. Peng, 2018: Projected trends in high-mortality heatwaves under different scenarios of climate, population, and adaptation in 82 US communities. Clim. Change, 146 (3-4), 455–470, doi:10.1007/s10584-016-1779-x.
Andrews, O., et al., 2018: Implications for workability and survivability in populations exposed to extreme heat under climate change: a modelling study. Lancet Planet. Health, 2 (12), E540–E547, doi:10.1016/s2542-5196(18)30240-7.
Anenberg, S.C., et al., 2020: Synergistic health effects of air pollution, temperature, and pollen exposure: a systematic review of epidemiological evidence. Environ. Health, 19 (1), doi:10.1186/s12940-020-00681-z.
Anwar, N., A. Sawas and D. Mustafa, 2019: ‘Without water, there is no life’: negotiating everyday risks and gendered insecurities in Karachi’s informal settlements. Urban Stud. , doi:10.1177/0042098019834160.
Apergis, N., 2018: The impact of greenhouse gas emissions on personal well-being: evidence from a panel of 58 countries and aggregate and regional country samples. J. Happiness Stud. , 19 (1), 69–80, doi:10.1007/s10902-016-9809-y.
Aracena, S., et al., 2021: Health system adaptation to climate change: a Peruvian case study. Health Policy Plan. , 36 (1), 45–83, doi:10.1093/heapol/czaa072.
Arbuthnott, K., S. Hajat, C. Heaviside and S. Vardoulakis, 2020: Years of life lost and mortality due to heat and cold in the three largest English cities. Environ. Int. , 144, 105966, doi:10.1016/j.envint.2020.105966.
Archer, J., et al., 2020: Intestinal schistosomiasis and giardiasis co-infection in Sub-Saharan Africa: Can a one health approach improve control of each waterborne parasite simultaneously?Trop. Med. Infect. Dis. , 5 (3), doi:10.3390/tropicalmed5030137.
Archibald, A.T., et al., 2020: On the changes in surface ozone over the twenty-first century: sensitivity to changes in surface temperature and chemical mechanisms. Philos. Trans. Royal Soc. A Math. Phys. Eng. Sci. , 378 (2183), doi:10.1098/rsta.2019.0329.
Arias, P.A., N. Bellouin, E. Coppola, R.G. Jones, G. Krinner, J. Marotzke, V. Naik, M.D. Palmer, G.-K. Plattner, J. Rogelj, M. Rojas, J. Sillmann, T. Storelvmo, P.W. Thorne, B. Trewin, K. Achuta Rao, B. Adhikary, R.P. Allan, K. Armour, G. Bala, R. Barimalala, S. Berger, J.G. Canadell, C. Cassou, A. Cherchi, W. Collins, W.D. Collins, S.L. Connors, S. Corti, F. Cruz, F.J. Dentener, C. Dereczynski, A. Di Luca, A. Diongue Niang, F.J. Doblas-Reyes, A. Dosio, H. Douville, F. Engelbrecht, V. Eyring, E. Fischer, P. Forster, B. Fox-Kemper, J.S. Fuglestvedt, J.C. Fyfe, N.P. Gillett, L. Goldfarb, I. Gorodetskaya, J.M. Gutierrez, R. Hamdi, E. Hawkins, H.T. Hewitt, P. Hope, A.S. Islam, C. Jones, D.S. Kaufman, R.E. Kopp, Y. Kosaka, J. Kossin, S. Krakovska, J.-Y. Lee, J. Li, T. Mauritsen, T.K. Maycock, M. Meinshausen, S.-K. Min, P.M.S. Monteiro, T. Ngo-Duc, F. Otto, I. Pinto, A. Pirani, K. Raghavan, R. Ranasinghe, A.C. Ruane, L. Ruiz, J.-B. Sallée, B.H. Samset, S. Sathyendranath, S.I. Seneviratne, A.A. Sörensson, S. Szopa, I. Takayabu, A.-M. Tréguier, B. van den Hurk, R. Vautard, K. von Schuckmann, S. Zaehle, X. Zhang, and K. Zickfeld, 2021: Technical Summary. In Climate Change 2021: The Physical Science Basis. Contribution of Working Group I to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change[Masson-Delmotte, V., P. Zhai, A. Pirani, S.L. Connors, C. Péan, S. Berger, N. Caud, Y. Chen, L. Goldfarb, M.I. Gomis, M. Huang, K. Leitzell, E. Lonnoy, J.B.R. Matthews, T.K. Maycock, T. Waterfield, O. Yelekçi, R. Yu, and B. Zhou (eds.)]. Cambridge University Press. In Press.
Armitage, R. and L. Nellums, 2020: Water, climate change, and COVID-19: prioritising those in water-stressed settings. Lancet Planet. Health, 4 (5), E175–E175.
Armstrong, B., et al., 2017: Longer-term impact of high and low temperature on mortality: an international study to clarify length of mortality displacement. Environ. Health Perspect. , 125 (10), doi:10.1289/ehp1756.
Arnall, A., 2014: A climate of control: flooding, displacement and planned resettlement in the Lower Zambezi River valley, Mozambique. Geogr. J. , 180 (2), 141–150, doi:10.1111/geoj.12036.
Arora, D., et al., 2017: Gender (Im)balance in Productive and Reproductive Labor Among Livestock Producers in Colombia: Implications for Climate Change Responses. CGIAR Research Program on Climate Change, Agriculture and Food Security, https://hdl.handle.net/10568/79940 Last accessed 30 September 2021.
Arroyo, V., et al., 2016: Impact of air pollution and temperature on adverse birth outcomes: Madrid, 2001–2009. Environ. Pollut. , 218, 1154–1161, doi:10.1016/j.envpol.2016.08.069.
Asadgol, Z., et al., 2019: The effect of climate change on cholera disease: the road ahead using artificial neural network. PLoS ONE, 14 (11), e224813, doi:10.1371/journal.pone.0224813.
Asefi-Najafabady, S., et al., 2018: Climate change, population, and poverty: vulnerability and exposure to heat stress in countries bordering the Great Lakes of Africa. Clim. Change, 148 (4), 561–573, doi:10.1007/s10584-018-2211-5.
Ash, K. and N. Obradovich, 2020: Climatic stress, internal migration, and Syrian civil war onset. J. Confl. Resolut. , 64 (1), 3–31.
Asmall, T., et al., 2021: The adverse health effects associated with drought in Africa. Sci. Total Environ. , 793, 148500, doi:10.1016/j.scitotenv.2021.148500.
Asmare, B., M. Taddele, S. Berihun and F. Wagnew, 2018: Nutritional status and correlation with academic performance among primary school children, northwest Ethiopia. BMC Res. Notes, 11 (1), 1–6.
Asplund, T. and M. Hjerpe, 2020: Project coordinators’ views on climate adaptation costs and benefits–justice implications. Local Environ. , 25 (2), 114–129.
Åström, C., et al., 2017: Vulnerability reduction needed to maintain current burdens of heat-related mortality in a changing climate—magnitude and determinants. Int. J. Environ. Res. Public Health, 14 (7), 741–741.
Åström, D.O., et al., 2020: Heat wave-related mortality in Sweden: a case-crossover study investigating effect modification by neighbourhood deprivation. Scand. J. Public Health, 48 (4), 428–435, doi:10.1177/1403494818801615.
Åström, D.O., K.L. Ebi, A.M. Vicedo-Cabrera and A. Gasparrini, 2018: Investigating changes in mortality attributable to heat and cold in Stockholm, Sweden. Int. J. Biometeorol. , 62 (9), 1777–1780, doi:10.1007/s00484-018-1556-9.
Åström, D.O., B. Forsberg, K.L. Ebi and J. Rocklöv, 2013: Attributing mortality from extreme temperatures to climate change in Stockholm, Sweden. Nat. Clim. Change, 3 (12), 1050–1054, doi:10.1038/nclimate2022.
Asugeni, J., D. MacLaren, P.D. Massey and R. Speare, 2015: Mental health issues from rising sea level in a remote coastal region of the Solomon Islands: current and future. Australas. Psychiatry, 23 (6), 22–25, doi:10.1177/1039856215609767.
Atef, S.S., F. Sadeqinazhad, F. Farjaad and D.M. Amatya, 2019: Water conflict management and cooperation between Afghanistan and Pakistan. J. Hydrol. Reg. Stud. , 570, 875–892.
Atkinson, H. and J. Bruce, 2015: Adolescent girls, human rights and the expanding climate emergency. Ann. Glob. Health, 81 (3), 323–330, doi:10.1016/j.aogh.2015.08.003.
Åtland, K., 2013: The security implications of climate change in the Arctic Ocean. In: Environmental Security in the Arctic Ocean. Springer, Dordrecht. pp. 205–216.
Auger, N., et al., 2017: Elevated outdoor temperatures and risk of stillbirth. Int. J. Epidemiol. , 46 (1), 200–208.
Avaria-Llautureo, J., et al., 2021: Historical warming consistently decreased size, dispersal and speciation rate of fish. Nat. Clim. Change, 1–7. DOI https://doi.org/10.1038/s41558-021-01123-5.
Avashia, V., A. Garg and H. Dholakia, 2021: Understanding temperature related health risk in context of urban land use changes. Landsc. Urban Plan. , 212, doi:10.1016/j.lurbplan.2021.104107.
Avila-Palencia, I., et al., 2018: The effects of transport mode use on self-perceived health, mental health, and social contact measures: a cross-sectional and longitudinal study. Environ. Int. , 120, 199–206, doi:10.1016/j.envint.2018.08.002.
Awuor, L., R. Meldrum and E. Liberda, 2020: Institutional engagement practices as barriers to public health capacity in climate change policy discourse: lessons from the Canadian province of Ontario. Int. J. Environ. Res. Public Health, 17 (17), doi:10.3390/ijerph17176338.
Axelsen, J.B., R. Yaari, B.T. Grenfell and L. Stone, 2014: Multiannual forecasting of seasonal influenza dynamics reveals climatic and evolutionary drivers. Proc. Natl. Acad. Sci. U.S.A. , 111 (26), 9538–9542, doi:10.1073/pnas.1321656111.
Ayano, G., 2018: Significance of mental health legislation for successful primary care for mental health and community mental health services: a review. Afr. J. Prim. Health Care Fam. Med. , 10 (1), 1–4, doi:10.4102/phcfm.v10i1.1429.
Ayeb-Karlsson, S., D. Kniveton and T. Cannon, 2020: Trapped in the prison of the mind: notions of climate-induced (im)mobility decision-making and wellbeing from an urban informal settlement in Bangladesh. Palgrave Commun. , 6 (1), 62, doi:10.1057/s41599-020-0443-2.
Ayeb-Karlsson, S., C.D. Smith and D. Kniveton, 2018: A discursive review of the textual use of ‘trapped’ in environmental migration studies: the conceptual birth and troubled teenage years of trapped populations. Ambio, 47 (5), 557–573, doi:10.1007/s13280-017-1007-6.
Azage, M., A. Kumie, A. Worku and A. Bagtzoglou, 2015: Childhood diarrhea exhibits spatiotemporal variation in Northwest Ethiopia: a SaTScan spatial statistical analysis. PLoS ONE, 10 (12), doi:10.1371/journal.pone.0144690.
Baez, J., G. Caruso, V. Mueller and C. Niu, 2017: Droughts augment youth migration in Northern Latin America and the Caribbean. Clim. Change, 140 (3), 423–435.
Bai, X., et al., 2019: Distribution of geographical scale, data aggregation unit and period in the correlation analysis between temperature and incidence of HFRS in mainland China: A systematic review of 27 ecological studies. PLoS Negl. Trop. Dis. , 13 (8), doi:10.1371/journal.pntd.0007688.
Bai, Y.T., et al., 2015: Effects of climate and rodent factors on hemorrhagic fever with renal syndrome in Chongqing, China, 1997–2008. PLoS ONE, 10 (7), doi:10.1371/journal.pone.0133218.
Baidya, D., S. Maitra and S. Bhattacharjee, 2020: Facing post-cyclone disaster in times of COVID-19 pandemic in India: possible testing strategy to reduce further spread of disease. Asia-Pac. J. Public Health, 32 (6-7), 376–376, doi:10.1177/1010539520944717.
Baker-Austin, C., J. Trinanes, N. Gonzalez-Escalona and J. Martinez-Urtaza, 2017: Non-cholera vibrios: the microbial barometer of climate change. Trends Microbiol. , 25 (1), 76–84, doi:10.1016/j.tim.2016.09.008.
Balestri, S. and M. A. Maggioni, 2017: Land-use change and communal confllicts in Sub-Saharan Africa. Peace Econ. Peace Sci. Public Policy, 23 (4), doi:10.1515/peps-2017-0032.
Bamberg, S., T. Masson, K. Brewitt and N. Nemetschek, 2017: Threat, coping and flood prevention – a meta-analysis. J. Environ. Psychol. , 54, 116–126, doi:10.1016/j.jenvp.2017.08.001.
Bandura, A., 1982: Self-efficacy mechanism in human agency. American Psychologist, 37 (2), 122–147, doi:10.1037/0003-066X.37.2.122.
Bandyopadhyay, R., et al., 2016: Biological control of aflatoxins in Africa: current status and potential challenges in the face of climate change. World Mycotoxin J. , 9 (5), 771–789, doi:10.3920/wmj2016.2130.
Banerjee, S., R. Black, A. Mishra and D. Kniveton, 2019a: Assessing vulnerability of remittance-recipient and nonrecipient households in rural communities affected by extreme weather events: case studies from South-West China and North-East India. Popul. Space Place, 25 (2), doi:10.1002/psp.2157.
Banerjee, S., A. Hussain, S. Tuladhar and A. Mishra, 2019b: Building capacities of women for climate change adaptation: insights from migrant-sending households in Nepal. Clim. Change, 157 (3), 587–609, doi:10.1007/s10584-019-02572-w.
Bannister, T., et al., 2021: A pilot forecasting system for epidemic thunderstorm asthma in southeastern Australia. Bull. Am. Meteorol. Soc. , 102 (2), E399–E420, doi:10.1175/bams-d-19-0140.1.
Banwell, N., S. Rutherford, B. Mackey and C. Chu, 2018: Towards improved linkage of disaster risk reduction and climate change adaptation in health: a review. Int. J. Environ. Res. Public Health, 15 (4), doi:10.3390/ijerph15040793.
Bao, J., et al., 2019: Effects of heat on first-ever strokes and the effect modification of atmospheric pressure: a time-series study in Shenzhen, China. Sci. Total Environ. , 654, 1372–1378, doi:10.1016/j.scitotenv.2018.11.101.
Barach, P., et al., 2020: Disruption of healthcare: Will the COVID pandemic worsen non-COVID outcomes and disease outbreaks?Prog. Pediatr. Cardiol. , 59, 101254, doi:10.1016/j.ppedcard.2020.101254.
Barange, M., et al., 2018: Impacts of Climate Change on Fisheries and Aquaculture: Synthesis of Current Knowledge, Adaptation and Mitigation Options. Fisheries and Aquaculture Technical Paper. FAO, Rome.
Barnes, J.H., E.T. Hayes, T.J. Chatterton and J.W.S. Longhurst, 2014: Air quality action planning: why do barriers to remediation in local air quality management remain?J. Environ. Plan. Manag. , 57 (5), 660–681, doi:10.1080/09640568.2012.762573.
Barnett, J., 2019: Global environmental change I: climate resilient peace?Prog. Hum. Geogr. , 43 (5), 927–936, doi:10.1177/0309132518798077.
Barnett, J. and C. McMichael, 2018: The effects of climate change on the geography and timing of human mobility. Popul. Environ. , 39 (4), 339–356, doi:10.1007/s11111-018-0295-5.
Barquet, K., 2015: “Yes to peace”? Environmental peacemaking and transboundary conservation in Central America. Geoforum, 63, 14–24.
Barquet, K., P. Lujala and J. Rod, 2014: Transboundary conservation and militarized interstate disputes. Polit. Geogr. , 42, 1–11, doi:10.1016/j.polgeo.2014.05.003.
Barreca, A., et al., 2016: Adapting to climate change: the remarkable decline in the US temperature-mortality relationship over the twentieth century. J. Polit. Econ. , 124 (1), 105–159, doi:10.1086/684582.
Baryshnikova, N. and N. Pham, 2019: Natural disasters and mental health: a quantile approach. Econ. Lett. , 180, 62–66, doi:10.1016/j.econlet.2019.04.016.
Basel, B., G. Goby and J. Johnson, 2020: Community-based adaptation to climate change in villages of Western Province, Solomon Islands. Mar. Pollut. Bull. , 156, doi:10.1016/j.marpolbul.2020.111266.
Bateman, I., et al., 2020: Editorial: economics of the environment in the shadow of coronavirus. Environ. Resour. Econ. , 76 (4), 519–523, doi:10.1007/s10640-020-00496-z.
Battilani, P., et al., 2016: Aflatoxin B1 contamination in maize in Europe increases due to climate change. Sci. Rep. , 6. DOI: https://doi.org/10.1038/srep24328
Baylis, P., et al., 2018: Weather impacts expressed sentiment. PLoS ONE, 13 (4), doi:10.1371/journal.pone.0195750.
Beach, R., et al., 2019: Combining the effects of increased atmospheric carbon dioxide on protein, iron, and zinc availability and projected climate change on global diets: a modelling study. Lancet Planet. Health, 3 (7), E307–E317, doi:10.1016/s2542-5196(19)30094-4.
Becquart, N.A., E.N. Naumova, G. Singh and K.K.H. Chui, 2018: Cardiovascular disease hospitalizations in Louisiana parishes’ elderly before, during and after Hurricane Katrina. Int. J. Environ. Res. Public Health, 16 (1), doi:10.3390/ijerph16010074.
Beggs, P.J., 2021: Climate change, aeroallergens, and the aeroexposome. Environ. Res. Lett. , 16 (3), doi:10.1088/1748-9326/abda6 f.
Belay, A., J. Recha, T. Woldeamanuel and J. Morton, 2017: Smallholder farmers’ adaptation to climate change and determinants of their adaptation decisions in the Central Rift Valley of Ethiopia. Agric. Food Secur. , 6, 1–13, doi:10.1186/s40066-017-0100-1.
Belesova, K., I. Kelman and R. Boyd, 2016: Governance through economic paradigms: addressing climate change by accounting for health. Polit. Gov. , 4 (4), 87–96, doi:10.17645/pag.v4i4.729.
Belkin, L. and M. Kouchaki, 2017: Too hot to help! Exploring the impact of ambient temperature on helping. Eur. J. Soc. Psychol. , 47 (5), 525–538, doi:10.1002/ejsp.2242.
Bellemare, M.F., 2015: Rising food prices, food price volatility, and social unrest. Am. J. Agric. Econ. , 97 (1), 1–21.
Benmarhnia, T., et al., 2016: A difference-in-differences approach to assess the effect of a heat action plan on heat-related mortality, and differences in effectiveness according to sex, age, and socioeconomic status (Montreal, Quebec). Environ. Health Perspect. , 124 (11), 1694–1699, doi:10.1289/ehp203.
Benmarhnia, T., S. Deguen, J.S. Kaufman and A. Smargiassi, 2015: Vulnerability to heat-related mortality a systematic review, meta-analysis, and meta-regression analysis. Epidemiology, 26 (6), 781–793, doi:10.1097/ede.0000000000000375.
Bennett, S., et al., 2020: Understanding the implications of the Sustainable Development Goals for health policy and systems research: results of a research priority setting exercise. Global. Health, 16 (1), doi:10.1186/s12992-019-0534-2.
Benveniste, H., J.C. Cuaresma, M. Gidden and R. Muttarak, 2021: Tracing international migration in projections of income and inequality across the Shared Socioeconomic Pathways. Clim. Change, 166, doi:10.1007/s10584-021-03133-w.
Benveniste, H., O. Michael and F. Marc, 2020: Effect of border policy on exposure and vulnerability to climate change. Proc. Natl. Acad. Sci. , 117 (43), doi:10.1073/pnas.2007597117.
Berndtsson, R. and K. Tussupova, 2020: The Future of Water Management in Central Asia. Multidisciplinary Digital Publishing Institute, Basel, Switzerland.
Berrang-Ford, L., et al., 2021: Systematic mapping of global research on climate and health: a machine learning review. Lancet Planet. Health. DOI: https://doi.org/10.1016/S2542-5196(21)00179-0
Berry, H.L., K. Bowen and T. Kjellstrom, 2010: Climate change and mental health: a causal pathways framework. Int. J. Public Health, 55 (2), 123–132, doi:10.1007/s00038-009-0112-0.
Berry, L. and D. Peel, 2015: Worrying about climate change: is it responsible to promote public debate?BJPsych Int. , 12 (2), 31–32.
Berry, P., et al., 2018: Assessing health vulnerabilities and adaptation to climate change: a review of international progress. Int. J. Environ. Res. Public Health, 15 (12), doi:10.3390/ijerph15122626.
Bertana, A., 2020: The role of power in community participation: relocation as climate change adaptation in Fiji. Environ. Plan. C Polit. Space, 38, 239965442090939, doi:10.1177/2399654420909394.
Bettini, G. and G. Gioli, 2016: Waltz with development: insights on the developmentalization of climate-induced migration. Migr. Dev. , 5 (2), 171–189.
Betts, R., et al., 2018: Changes in climate extremes, fresh water availability and vulnerability to food insecurity projected at 1.5 degrees C and 2 degrees C global warming with a higher-resolution global climate model. Philos. Trans. Royal Soc. A Math. Phys. Eng. Sci. , 376 (2119), doi:10.1098/rsta.2016.0452.
Beveridge, L., et al., 2019: Experiences and drivers of food insecurity in Guatemala’s dry corridor: insights from the integration of ethnographic and household survey data. Front. Sustain. Food Syst. , 3, doi:10.3389/fsufs.2019.00065.
Beyene, T., D. Endalamaw, Y. Tolossa and A. Feyisa, 2015: Evaluation of rational use of veterinary drugs especially antimicrobials and anthelmintics in Bishoftu, Central Ethiopia. BMC Res. Notes. DOI: https://doi.org/10.1186/s13104-015-1466-4
Beyer, J. and A. Vandermosten, 2021: Greenness of Stimulus Index. An Assessment of COVID-19 Stimulus by G20 Countries and Other Major Economies in Relation to Climate Action and Biodiversity Goals. Vivid Economics, London, UK. 93 pp.
Bezner Kerr, R., et al., 2021: Can agroecology improve food security and nutrition? A review. Glob. Food Secur. Policy Econ. Environ. , 29, doi:10.1016/j.gfs.2021.100540.
Bhagat, R., 2017: Migration, gender and right to the city. Econ. Polit. Wkly. , volume LII.pp. 35–40.
Bharara, T., et al., 2018: Green hospital initiative by a North Delhi tertiary care hospital: current scenario and future prospects. J. Clin. Diagn. Res. , 12, DC10–DC14, doi:10.7860/jcdr/2018/34360.11758.
Bhatt, S., et al., 2013: The global distribution and burden of dengue. Nature, 496 (7446), 504–507, doi:10.1038/nature12060.
Bhatta, G., P. Aggarwal, S. Poudel and D. Belgrave, 2015: Climate-induced migration in South Asia: migration decisions and the gender dimensions of adverse climatic events. J. Rural Community Dev. , 10, 1–23.
Bhavnani, R.R. and B. Lacina, 2015: The effects of weather-induced migration on sons of the soil riots in India. World Pol. , 67, 760.
Billiot, S., et al., 2019: Indigenous perspectives for strengthening social responses to global environmental changes: a response to the social work grand challenge on environmental change. J. Community Pract. , 27 (3-4), 296–316, doi:10.1080/10705422.2019.1658677.
Binder, S., J. Barile, C. Baker and B. Kulp, 2019: Home buyouts and household recovery: neighborhood differences three years after Hurricane Sandy. Environ. Hazards, 18 (2), 127–145, doi:10.1080/17477891.2018.1511404.
Blattman, C. and E. Miguel, 2010: Civil war. J. Econ. Lit. , 48 (1), 3–57.
Bless, P.J., et al., 2016: Acute gastroenteritis and campylobacteriosis in Swiss primary care: the viewpoint of general practitioners. PLoS ONE, 11 (9), e161650, doi:10.1371/journal.pone.0161650.
Boas, I., et al., 2019: Climate migration myths. Nat. Clim. Change, 9 (12), 901–903, doi:10.1038/s41558-019-0633-3.
Boas, I. and D. Rothe, 2016: From conflict to resilience? Explaining recent changes in climate security discourse and practice. Environ. Polit. , 25 (4), 613–632, doi:10.1080/09644016.2016.1160479.
Bob, U. and S. Bronkhorst, 2014: Conflict-sensitive Adaptation to Climate Change in Africa[Carius, A. and D. Tänzler (eds.)]. Climate Diplomacy Series. Berliner Wissenschafts-Verlag, Berlin.
Boeckmann, M. and I. Rohn, 2014: Is planned adaptation to heat reducing heat-related mortality and illness? A systematic review. BMC Public Health, 14, doi:10.1186/1471-2458-14-1112.
Bogdanova, E., et al., 2021: The impact of climate change on the food (in)security of the Siberian indigenous peoples in the Arctic: environmental and health risks. Sustainability, 13 (5), doi:10.3390/su13052561.
Bohra-Mishra, P., et al., 2017: Climate variability and migration in the Philippines. Popul. Environ. , 38 (3), 286–308, doi:10.1007/s11111-016-0263-x.
Boin, A., P. ’t Hart, E. Stern and B. Sundelius, 2005: The Politics of Crisis Management: Public Leadership Under Pressure. Cambridge University Press, Cambridge.
Boithias, L., et al., 2016: Hydrological regime and water shortage as drivers of the seasonal incidence of diarrheal diseases in a tropical montane environment. PLoS Negl. Trop. Dis. , 10 (12), e5195, doi:10.1371/journal.pntd.0005195.
Bol, D., M. Giani, A. Blais and P. Loewen, 2020: The effect of COVID-19 lockdowns on political support: some good news for democracy?Eur. J. Polit. Res. , 60 (2), 497–505, doi:10.1111/1475-6765.12401.
Bollyky, T.J., T. Templin, M. Cohen and J.L. Dieleman, 2017: Lower-income countries that face the most rapid shift in noncommunicable disease burden are also the least prepared. Health Aff. , 36 (11), 1866–1875.
Boon, E.K. and S.W. Anuga, 2020: Circular economy and its relevance for improving food and nutrition security in Sub-Saharan Africa: the case of Ghana. Mater. Circ. Econ. , 2. pp. 1-14.
Boonruksa, P., T. Maturachon, P. Kongtip and S. Woskie, 2020: Heat stress, physiological response, and heat-related symptoms among Thai sugarcane workers. Int. J. Environ. Res. Public Health, 17 (17), doi:10.3390/ijerph17176363.
Booth, S. and D. Zeller, 2005: Mercury, food webs, and marine mammals: implications of diet and climate change for human health. Environ. Health Perspect. , 113 (5), 521–526, doi:10.1289/ehp.7603.
Borderon, M., et al., 2019: Migration influenced by environmental change in Africa: a systematic review of empirical evidence. Demogr. Res. , 41, 491–544, doi:10.4054/DemRes.2019.41.18.
Borg, M., et al., 2017: The impact of daily temperature on renal disease incidence: an ecological study. Environ. Health, 16, doi:10.1186/s12940-017-0331-4.
Borg, M. A., et al., 2021: Occupational heat stress and economic burden: a review of global evidence. Environ. Res. , 195, doi:10.1016/j.envres.2021.110781.
Borrows, J., 2019: Earth bound: indigenous resurgence and environmental reconciliation. In: Resurgence and Reconciliation: Indigenous-Settler Relations and Earth Teachings[Asch, M., J. Borrows and J. Tully(eds.)]. University of Toronto Press, Toronto, pp. 49–82.
Boscarino, J.A., et al., 2017: Mental health outcomes among vulnerable residents after Hurricane Sandy: implications for disaster research and planning. Am. J. Disaster Med. , 9 (2), 97–106.
Boscarino, J.A., et al., 2013: Mental health outcomes at the Jersey shore after Hurricane Sandy. Int. J. Emerg. Ment. Health, 15 (3), 147–158.
Bose-O’Reilly, S., et al., 2021: COVID-19 and heat waves: New challenges for healthcare systems. Environ. Res. , 198, 111153, doi:10.1016/j.envres.2021.111153.
Botana, L.M., 2016: Toxicological perspective on climate change: aquatic toxins. Chem. Res. Toxicol. , 29 (4), 619–625, doi:10.1021/acs.chemrestox.6b00020.
Bouma, M., A. Siraj, X. Rodo and M. Pascual, 2016: El Nino-based malaria epidemic warning for Oromia, Ethiopia, from August 2016 to July 2017. Trop. Med. Int. Health, 21 (11), 1481–1488, doi:10.1111/tmi.12776.
Bouman, T., L. Steg and T. Dietz, 2020: Insights from early COVID-19 responses about promoting sustainable action. Nat. Sustain. , doi:10.1038/s41893-020-00626-x.
Bourke, S., et al., 2018: Evidence Review of Indigenous Culture for Health and Wellbeing. Int. J. Health Wellness Soc. , 8 (4), 11-27
Bowen, K., D. Alexander, F. Miller and V. Dany, 2014a: Using social network analysis to evaluate health-related adaptation decision-making in Cambodia. Int. J. Environ. Res. Public Health, 11 (2), 1605–1625, doi:10.3390/ijerph110201605.
Bowen, K., K. Ebi and S. Friel, 2014b: Climate change adaptation and mitigation: next steps for cross-sectoral action to protect global health. Mitig. Adapt. Strateg. Glob. Change, 19 (7), 1033–1040, doi:10.1007/s11027-013-9458-y.
Bowen, K., et al., 2021: Human health and climate change in the Pacific: a review of current knowledge. Glob. Transitions (In press).
Bowen, K.J. and K.L. Ebi, 2017: Health risks of climate change in the World Health Organization South-East Asia Region. WHO South East Asia J. Public Health, 6 (2), 3–8.
Bowles, D.C., 2015: Climate change and health adaptation: consequences for indigenous physical and mental health. Ann. Glob. Health, 81 (3), 427–431, doi:10.1016/j.aogh.2015.06.004.
Boyer, C., et al., 2020: Using implementation science for health adaptation: opportunities for Pacific island countries. Health Aff. , 39 (12), 2160–2167, doi:10.1377/hlthaff.2020.01101.
Boyle, M., et al., 2020: Cities and the climate and ecological emergency: the Liverpool city region response. J. Urban Regen. Renew. , 13, 365–379.
Bradley, G.L., J.P. Reser, A.I. Glendon and M.C. Ellul, 2014: Distress and coping in response to climate change. In: Stress and Anxiety: Applications to Social and Environmental Threats, Psychological Well-being, Occupational Challenges, and Developmental Psychology Climate Change, Lagos Verlag Berlin, Berlin. pp. 33–42.
Bragg, C., et al., 2018: Remittances as aid following major sudden-onset natural disasters. Disasters, 42 (1), 3–18, doi:10.1111/disa.12229.
Brauer, M., J. Zhao, F. Bennitt and J. Stanaway, 2020: Global access to handwashing: implications for COVID-19 control in low-income countries. Environ. Health Perspect. , 128 (5), doi:10.1289/ehp7200.
Bremberg, N., H. Sonnsjö and M. Mobjörk, 2019: The EU and climate-related security risks: a community of practice in the making?J. Eur. Integr. , 41 (5), 623–639.
Brenkert-Smith, H., R. Meldrum and A. Champ, 2015: Climate change beliefs and hazard mitigation behaviors: homeowners and wildfire risk. Environ. Hazards, 14 (4), 341–360.
Broadbent, A.M., E.S. Krayenhoff and M. Georgescu, 2020: The motley drivers of heat and cold exposure in 21st century US cities. Proc. Natl. Acad. Sci. U.S.A. , 117 (35), 21108–21117, doi:10.1073/pnas.2005492117.
Bromet, E., et al., 2017: Post-traumatic stress disorder associated with natural and human-made disasters in the World Mental Health Surveys. Psychol. Med. , 47 (2), 227–241, doi:10.1017/s0033291716002026.
Brooks, H.E., 2013: Severe thunderstorms and climate change. Atmos. Res. , 123, 129–138, doi:10.1016/j.atmosres.2012.04.002.
Brosemer, K., et al., 2020: The energy crises revealed by COVID: intersections of indigeneity, inequity, and health. Energy Res. Soc. Sci. , 68, doi:10.1016/j.erss.2020.101661.
Brown, M.R.G., et al., 2019: After the Fort McMurray wildfire there are significant increases in mental health symptoms in grade 7–12 students compared to controls. BMC Psychiatry, 19, doi:10.1186/s12888-019-2074-y.
Brown, R.C., et al., 2017: Psychosocial interventions for children and adolescents after man-made and natural disasters: a meta-analysis and systematic review. Psychol. Med. , 47 (11), 1893–1905, doi:10.1017/s0033291717000496.
Brubacher, J., et al., 2020: Associations of five food- and water-borne diseases with ecological zone, land use and aquifer type in a changing climate. Sci. Total Environ. , 728, 138808, doi:10.1016/j.scitotenv.2020.138808.
Brügger, A., et al., 2015: Psychological responses to the proximity of climate change. Nat. Clim. Change, 5 (12), 1031–1037, doi:10.1038/nclimate2760.
Brunekreef, B., et al., 2021: Air pollution and COVID-19. Including Elements of Air Pollution in Rural Areas, Indoor Air Pollution and Vulnerability and Resilience Aspects of Our Society Against Respiratory Disease, Social Inequality Stemming from Air Pollution Study for the Committee on Environment, Public Health and Food Safety. Policy Department for Economic, Scientific and Quality of Life Policies, European Parliament, Luxembourg.
Bryson, J., et al., 2021: Seasonality, climate change, and food security during pregnancy among indigenous and non-indigenous women in rural Uganda: implications for maternal-infant health. PLoS ONE, 16 (3), doi:10.1371/journal.pone.0247198.
Brzoska, M., 2018: Weather extremes, disasters, and collective violence: conditions, mechanisms, and disaster-related policies in recent research. Curr. Clim. Change Rep. , 4 (4), 320–329.
Buckley, R., et al., 2019: Economic value of protected areas via visitor mental health. Nat. Commun. , 10 (1), 1–10, doi:10.1038/s41467-019-12631-6.
Buhaug, H., M. Croicu, H. Fjelde and N. v. Uexkull, 2020: A conditional model of local income shock and civil conflict. The Journal of Politics, 83 (1), 354-366.
Buhaug, H., et al., 2014: One effect to rule them all? A comment on climate and conflict. Clim. Change, 127 (3-4), 391–397.
Buhaug, H. and J. Vestby, 2019: On growth projections in the Shared Socioeconomic Pathways. Glob. Environ. Polit. , 19 (4), 118–132.
Buhaug, H. and N. von Uexkull, 2021: Vicious circles: violence, vulnerability, and climate change. Annu. Rev. Environ. Resour. , 46, 545-568.
Bukvic, A. and G. Owen, 2017: Attitudes towards relocation following Hurricane Sandy: should we stay or should we go?Disasters, 41 (1), 101–123, doi:10.1111/disa.12186.
Bunker, A., et al., 2016: Effects of air temperature on climate-sensitive mortality and morbidity outcomes in the elderly; a systematic review and meta-analysis of epidemiological evidence. EBioMedicine, 6, 258–268, doi:10.1016/j.ebiom.2016.02.034.
Bunn, M., 2019: Nuclear disarmament, nuclear energy, and climate change: exploring the linkages. Routledge , Oxfordshire .
Burkart, G., et al., 2021: Projecting global mortality due to non-optimal temperature from 2020 to 2100: a global burden of disease forecasting study. The Lancet., http://dx.doi.org/10.2139/ssrn.3723614 .
Burke, M., et al., 2018: Higher temperatures increase suicide rates in the United States and Mexico. Nat. Clim. Change, 8 (8), 723, doi:10.1038/s41558-018-0222-x.
Burke, M., S.M. Hsiang and E. Miguel, 2015a: Global non-linear effect of temperature on economic production. Nature, 527 (7577), 235–239, doi:10.1038/nature15725.
Burke, M., S. M. Hsiang and E. Miguel, 2015b: Climate and conflict. Annu. Rev. Econ. , 7 (1), 577–617, doi:10.1146/annurev-economics-080614-115430.
Burnham, M. and Z. Ma, 2017: Climate change adaptation: factors influencing Chinese smallholder farmers’ perceived self-efficacy and adaptation intent. Reg. Environ. Change, 17 (1), 171–186.
Busby, J., 2018: Taking stock: the field of climate and security. Curr. Clim. Change Rep. , 4 (4), 338–346.
Busby, J. and N. Krishnan, 2017: Widening the Scope to Asia: Climate Change and Security. The Center for Climate and Security, Washington DC.
Busby, J., et al., 2018: In harm’s way: climate security vulnerability in Asia. World Dev. , 112, 88–118.
Butler, C.D. and D. Harley, 2010: Primary, secondary and tertiary effects of eco-climatic change: the medical response. Postgrad. Med. J. , 86 (1014), 230, doi:10.1136/pgmj.2009.082727.
Butler, T., et al., 2019: Aboriginal and Torres Strait Islander people’s domains of wellbeing: a comprehensive literature review. Soc. Sci. Med. , 233, 138–157, doi:10.1016/j.socscimed.2019.06.004.
Butt, N., F. Lambrick, M. Menton and A. Renwick, 2019: The supply chain of violence. Nat. Sustain. , 2 (8), 742–747.
Cai, R., S. Feng, M. Oppenheimer and M. Pytlikova, 2016: Climate variability and international migration: the importance of the agricultural linkage. J. Environ. Econ. Manag. , 79, 135–151, doi:10.1016/j.jeem.2016.06.005.
Cai, W.J., et al., 2021: The 2020 China report of the Lancet Countdown on health and climate change. Lancet Public Health, 6 (1), E64–E81, doi:10.1016/s2468-2667(20)30256-5.
Caini, S., F. Schellevis, C.E. Seblain and J. Paget, 2018: Important changes in the timing of influenza epidemics in the WHO European Region over the past 20 years: virological surveillance 1996 to 2016. Euro Surveill. , 23 (1), 2–10, doi:10.2807/1560-7917.es.2018.23.1.17-00302.
Call, M., C. Gray, M. Yunus and M. Emch, 2017: Disruption, not displacement: environmental variability and temporary migration in Bangladesh. Glob. Environ. Change, 46, 157–165.
Camacho, A., et al., 2018: Cholera epidemic in Yemen, 2016–18: an analysis of surveillance data. Lancet Glob. Health, 6 (6), e680–e690, doi:10.1016/s2214-109x(18)30230-4.
Caminade, C., K.M. McIntyre and A.E. Jones, 2019: Impact of recent and future climate change on vector-borne diseases. Ann. N. Y. Acad. Sci. , 1436 (1), 157–173, doi:10.1111/nyas.13950.
Campagnolo, L. and M. Davide, 2019: Can the Paris deal boost SDGs achievement? An assessment of climate mitigation co-benefits or side-effects on poverty and inequality. World Dev. , 122, 96–109, doi:10.1016/j.worlddev.2019.05.015.
Campbell, S., T.A. Remenyi, C.J. White and F.H. Johnston, 2018: Heatwave and health impact research: a global review. Health Place, 53, 210–218, doi:10.1016/j.healthplace.2018.08.017.
Canu, W.H., J.P. Jameson, E.H. Steele and M. Denslow, 2017: Mountaintop removal coal mining and emergent cases of psychological disorder in Kentucky. Community Ment. Health J. , 53 (7), 802–810, doi:10.1007/s10597-017-0122-y.
Cárdenas, M.L. and E. Olivius, 2021: Building peace in the shadow of war: women-to-women diplomacy as alternative peacebuilding practice in Myanmar. J. Interv. Statebuild. , 1–20. https://doi.org/10.1080/17502977.2021.1917254
Carleton, T.A., 2017: Crop-damaging temperatures increase suicide rates in India. Proc. Natl. Acad. Sci. U.S.A. , 114 (33), 8746–8751, doi:10.1073/pnas.1701354114.
Carleton, T.A. and S.M. Hsiang, 2016: Social and economic impacts of climate. Science, 353 (6304).
Carlsten, C., S. Salvi, G.W.K. Wong and K.F. Chung, 2020: Personal strategies to minimise effects of air pollution on respiratory health: advice for providers, patients and the public. Eur. Respir. J. , 55 (6), doi:10.1183/13993003.02056-2019.
Carlton, E., et al., 2016: A systematic review and meta-analysis of ambient temperature and diarrhoeal diseases. Int. J. Epidemiol. , 45 (1), 117–130, doi:10.1093/ije/dyv296.
Carman, J. and M. Zint, 2020: Defining and classifying personal and household climate change adaptation behaviors. Glob. Environ. Change Policy Dimens. , 61, doi:10.1016/j.gloenvcha.2020.102062.
Carrico, A.R. and K. Donato, 2019: Extreme weather and migration: evidence from Bangladesh. Popul. Environ. , 41 (1), 1–31, doi:10.1007/s11111-019-00322-9.
Carter, M. and S. Janzen, 2018: Social protection in the face of climate change: targeting principles and financing mechanisms. Environ. Dev. Econ. , 23 (3), 369–389, doi:10.1017/s1355770x17000407.
Caruso, R., I. Petrarca and R. Ricciuti, 2016: Climate change, rice crops, and violence: evidence from Indonesia. J. Peace Res. , 53 (1), 66–83, doi:10.1177/0022343315616061.
Carvajal, T.M., et al., 2018: Machine learning methods reveal the temporal pattern of dengue incidence using meteorological factors in metropolitan Manila, Philippines. BMC Infect. Dis. , 18 (1), 183, doi:10.1186/s12879-018-3066-0.
Casado-Asensio, J., T. Kato and J. Sedemund, 2020: Climate resilient development. In: Development Co-operation Report 2020: Learning from Crises, Building Resilience[Oecd(ed.)]. OECD Publishing, Paris.
Cattaneo, C., et al., 2019: Human migration in the era of climate change. Rev. Environ. Econ. Policy, 13 (2), 189–206, doi:10.1093/reep/rez008.
Cattaneo, C. and G, Peri, 2016: The migration response to increasing temperatures. J. Dev. Econ. , 122, 127–146.
Cattaneo, C. and E. Massetti, 2019: Does harmful climate increase or decrease migration? Evidence from rural households in Nigeria. Clim. Change Econ. , 10 (4), doi:10.1142/s2010007819500131.
Cederman, L.-E. and N.B. Weidmann, 2017: Predicting armed conflict: time to adjust our expectations?Science, 355 (6324), 474–476.
Centers for Disease Control and Prevention., 2019: CDC’s Building Resilience Against Climate Effects (BRACE) Framework. National Centre for Environmental Health, Atlanta.
Céspedes-Báez, L.M.R. and F. J. Ruiz, 2018: ‘Peace without women does not go!’ Women’s struggle for inclusion in Colombia’s peace process with the FARC, Colombia Internacional, 83–109, https://doi.org/107440/colombiaint94.2018.04.
Chadsuthi, S., S. Iamsirithaworn, W. Triampo and D.A. Cummings, 2016: The impact of rainfall and temperature on the spatial progression of cases during the chikungunya re-emergence in Thailand in 2008–2009. Trans. R. Soc. Trop. Med. Hyg. , 110 (2), 125–133, doi:10.1093/trstmh/trv114.
Chambers, J., 2020: Global and cross-country analysis of exposure of vulnerable populations to heatwaves from 1980 to 2018. Clim. Change, 163 (1), 539–558, doi:10.1007/s10584-020-02884-2.
Chan, E., et al., 2018: Association between ambient temperatures and mental disorder hospitalizations in a subtropical city: a time-series study of Hong Kong special administrative region. Int. J. Environ. Res. Public Health, 15 (4), 754.
Chan, E.Y.Y. and S. Peijun, 2017: Health and risks: integrating health into disaster risk reduction, risk communication, and building resilient communities. Int. J. Disaster Risk Sci. , 8 (2), 107–108, doi:10.1007/s13753-017-0131-z.
Chandra, A., et al., 2017: Gendered vulnerabilities of smallholder farmers to climate change in conflict-prone areas: a case study from Mindanao, Philippines. J. Rural Stud. , 50, 45–59, doi:10.1016/j.jrurstud.2016.12.011.
Chang, A.Y., et al., 2019: Past, present, and future of global health financing: a review of development assistance, government, out-of-pocket, and other private spending on health for 195 countries, 1995–2050. Lancet , 393 (10187), 2233–2260.
Chang, C.C. and S.C. Chen, 2015: Colliding epidemics and the rise of cryptococcosis. J. Fungi, 2 (1), doi:10.3390/jof2010001.
Chang, C.J., C.S. Chen, C.J. Tien and M.R. Lu, 2018: Epidemiological, clinical and climatic characteristics of dengue fever in Kaohsiung City, Taiwan with implication for prevention and control. PLoS ONE, 13 (1), e190637, doi:10.1371/journal.pone.0190637.
Chang, K.M., et al., 2017: Ancillary health effects of climate mitigation scenarios as drivers of policy uptake: a review of air quality, transportation and diet co-benefits modeling studies. Environ. Res. Lett. , 12 (11), 113001, doi:10.1088/1748-9326/aa8f7b.
Chapin, III, F.S., et al., 2016: Community-empowered adaptation for self-reliance. Curr. Opin. Environ. Sustain. , 19, 67–75, doi:10.1016/j.cosust.2015.12.008.
Chapra, S.C., et al., 2017: Climate change impacts on harmful algal blooms in US freshwaters: a screening-level assessment. Environ. Sci. Technol. , 51 (16), 8933–8943.
Charlesworth, K. and M. Jamieson, 2019: Healthcare in a carbon-constrained world. Aust. Health Rev. , 43 (3), 241–245, doi:10.1071/ah17184.
Charlesworth, K.E. and M. Jamieson, 2018: Healthcare in a carbon-constrained world. Aust. Health Rev. , doi:10.1071/ah17184.
Charlesworth, K.E., G.J. Stewart and P. Sainsbury, 2018: Addressing the carbon footprint of health organisations: eight lessons for implementation. Public Health Res. Pract. , 28 (4), doi:10.17061/phrp2841830.
Charlson, F., et al., 2021: Climate change and mental health: a scoping review. Int. J. Environ. Res. Public Health, 18 (9), doi:10.3390/ijerph18094486.
Chen, C.C., et al., 2021a: Projection of future temperature extremes, related mortality, and adaptation due to climate and population changes in Taiwan. Sci. Total Environ. , 760, doi:10.1016/j.scitotenv.2020.143373.
Chen, J., et al., 2020: Global socioeconomic exposure of heat extremes under climate change. J. Clean. Prod. , 277, doi:10.1016/j.jclepro.2020.123275.
Chen, J.J., V. Mueller, Y. Jia and S. Tseng, 2017: Validating migration responses to flooding using satellite and vital registration data. Am. Econ. Rev. , 107 (5), 441–445.
Chen, K., et al., 2019: Temporal variations in the triggering of myocardial infarction by air temperature in Augsburg, Germany, 1987–2014. Eur. Heart. J. , doi:10.1093/eurheartj/ehz116.
Chen, K., et al., 2018: Future ozone-related acute excess mortality under climate and population change scenarios in China: a modeling study. PLoS Med. , 15 (7), doi:10.1371/journal.pmed.1002598.
Chen, L., et al., 2021b: The occurrence and control of waterborne viruses in drinking water treatment: a review. Chemosphere, 281, 130728, doi:10.1016/j.chemosphere.2021.130728.
Chen, M., 2015: Self-efficacy or collective efficacy within the cognitive theory of stress model: Which more effectively explains people’s self-reported proenvironmental behavior?J. Environ. Psychol. , 42, 66–75, doi:10.1016/j.jenvp.2015.02.002.
Cheng, A., et al., 2017: Analyzing the potential risk of climate change on Lyme disease in Eastern Ontario, Canada using time series remotely sensed temperature data and tick population modelling. Remote Sens. , 9 (6), doi:10.3390/rs9060609.
Cheng, J. and P. Berry, 2013: Development of key indicators to quantify the health impacts of climate change on Canadians. Int. J. Public Health, 58 (5), 765–775, doi:10.1007/s00038-013-0499-5.
Cheng, J., et al., 2018: Heatwave and elderly mortality: an evaluation of death burden and health costs considering short-term mortality displacement. Environ. Int. , 115, 334–342, doi:10.1016/j.envint.2018.03.041.
Cheng, J., et al., 2019: Impacts of heat, cold, and temperature variability on mortality in Australia, 2000–2009. Sci. Total Environ. , 651, 2558–2565, doi:10.1016/j.scitotenv.2018.10.186.
Cheng, J., et al., 2016: Impacts of temperature change on ambulance dispatches and seasonal effect modification. Int. J. Biometeorol. , 60 (12), 1863–1871, doi:10.1007/s00484-016-1173-4.
Cheng, L., et al., 2020: Record-setting ocean warmth continued in 2019. Adv. Atmos. Sci. , 37 (2), 137–142, doi:10.1007/s00376-020-9283-7.
Cheng, S., et al., 2021: The effect of average temperature on suicide rates in five urban California counties 1999–2019: an ecological time series analysis. BMC public health, 21 (1), 1-9.
Chersich, M.F., F. Scorgie, H. Rees and C.Y. Wright, 2018: How climate change can fuel listeriosis outbreaks in South Africa. S. Afr. Med. J. , 108 (6), 453–454, doi:10.7196/SAMJ.2018.v108i6.13274.
Chhetri, B.K., et al., 2019: Projected local rain events due to climate change and the impacts on waterborne diseases in Vancouver, British Columbia, Canada. Environ. Health, 18 (1), 116, doi:10.1186/s12940-019-0550-y.
Chiabai, A., et al., 2018a: The nexus between climate change, ecosystem services and human health: towards a conceptual framework. Sci. Total Environ. , 635, 1191–1204, doi:10.1016/j.scitotenv.2018.03.323.
Chiabai, A., J.V. Spadaro and M.B. Neumann, 2018b: Valuing deaths or years of life lost? Economic benefits of avoided mortality from early heat warning systems. Mitig. Adapt. Strateg. Glob. Change, 23 (7), 1159–1176, doi:10.1007/s11027-017-9778-4.
Chindarkar, N., 2012: Gender and climate change-induced migration: proposing a framework for analysis. Environ. Res. Lett. , 7 (2), 25601–25601, doi:10.1088/1748-9326/7/2/025601.
Choi, C., P. Berry and A. Smith, 2021: The climate benefits, co-benefits, and trade-offs of green infrastructure: a systematic literature review. J. Environ. Manag. , 291, doi:10.1016/j.jenvman.2021.112583.
Chong, K.C., et al., 2020a: Association between meteorological variations and activities of influenza A and B across different climate zones: a multi-region modelling analysis across the globe. J. Infect. , 80 (1), 84–98, doi:10.1016/j.jinf.2019.09.013.
Chong, K.C., et al., 2020b: Latitudes mediate the association between influenza activity and meteorological factors: a nationwide modelling analysis in 45 Japanese prefectures from 2000 to 2018. Sci. Total Environ. , 703, doi:10.1016/j.scitotenv.2019.134727.
Chort, I. and M. de la Rupelle, 2016: Determinants of Mexico-U.S. outward and return migration flows: a state-level panel data analysis. Demography, 53 (5), 1453–1476.
Choularton, R. and P. Krishnamurthy, 2019: How accurate is food security early warning? Evaluation of FEWS NET accuracy in Ethiopia. Food Sec. , 11 (2), 333–344, doi:10.1007/s12571-019-00909-y.
Chowdhury, F.R., et al., 2018a: The association between temperature, rainfall and humidity with common climate-sensitive infectious diseases in Bangladesh. PLoS ONE, 13 (6), e199579, doi:10.1371/journal.pone.0199579.
Chowdhury, S., S. Dey and K.R. Smith, 2018b: Ambient PM2.5 exposure and expected premature mortality to 2100 in India under climate change scenarios. Nat. Commun. , 9 (1), 318, doi:10.1038/s41467-017-02755-y.
Chu, E. and K. Michael, 2018: Recognition in urban climate justice: marginality and exclusion of migrants in Indian cities. Environ. Urban. , 31 (1), 139–156, doi:10.1177/0956247818814449.
Chuang, T.W., L.F. Chaves and P.J. Chen, 2017: Effects of local and regional climatic fluctuations on dengue outbreaks in southern Taiwan. PLoS ONE, 12 (6), e178698, doi:10.1371/journal.pone.0178698.
Chun, H.B.C., K. Hong, H. Hwang and S. Sohn, 2019: Effects of the El Niño southern oscillation on influenza peak activity timing. Online J. Public Health Inform. , 11 (1).DOI: https://doi.org/10.5210/ojphi.v11i1.9834
Chung, Y., et al., 2018: Changing susceptibility to non-optimum temperatures in Japan, 1972–2012: the role of climate, demographic, and socioeconomic factors. Environ. Health Perspect. , 126 (5), 57002–57002, doi:10.1289/ehp2546.
Cianconi, P., S. Betro and L. Janiri, 2020: The impact of climate change on mental health: a systematic descriptive review. Front. Psychiatry, 11, doi:10.3389/fpsyt.2020.00074.
Cidro, J., B. Adekunle, E. Peters and T. Martens, 2015: Beyond food security: understanding access to cultural food for urban indigenous people in Winnipeg as indigenous food sovereignty. Can. J. Urban Res. , 24, 24.
Cil, G. and T.A. Cameron, 2017: Potential climate change health risks from increases in heat waves: abnormal birth outcomes and adverse maternal health conditions. Risk Anal. , 37 (11), 2066–2079, doi:10.1111/risa.12767.
Cisse, G., 2019: Food-borne and water-borne diseases under climate change in low- and middle-income countries: further efforts needed for reducing environmental health exposure risks. Acta Trop. , 194, 181–188, doi:10.1016/j.actatropica .2019.03.012.
Cissé, G., J.A. Menezes and U. Confalonieri, 2018: Climate-sensitive infectious diseases. In: The Adaptation Gap Report 2018[Unep(ed.)]. United Nations Environment Programme (UNEP), Nairobi, Kenya, pp. 49–59. ISBN 978-9280737288.
Cissé, G., et al., 2016: Vulnerabilities of water and sanitation at households and community levels in face of climate variability and change: trends from historical climate time series in a West African medium-sized town. Int. J. Glob. Environ. Issues, 15 (1/2), 81–99.
Claeys, M.J., S. Rajagopalan, T.S. Nawrot and R.D. Brook, 2017: Climate and environmental triggers of acute myocardial infarction. Eur. Heart J. , 38 (13), 955–960, doi:10.1093/eurheartj/ehw151.
Clare, A., R. Graber, L. Jones and D. Conway, 2017: Subjective measures of climate resilience: What is the added value for policy and programming?Glob. Environ. Change Policy Dimens. , 46, 17–22, doi:10.1016/j.gloenvcha.2017.07.001.
Clark, M. and D. Tilman, 2017: Comparative analysis of environmental impacts of agricultural production systems, agricultural input efficiency, and food choice. Environ. Res. Lett. , 12 (6), doi:10.1088/1748-9326/aa6cd5.
Clayton, S. and B. Karazsia, 2020: Development and validation of a measure of climate change anxiety. J. Environ. Psychol. , 69, doi:10.1016/j.jenvp.2020.101434.
Clayton, S., C.M. Manning, K. Krygsman and M. Speiser, 2017: Mental Health and Our Changing Climate: Impacts, Implications, and Guidance. American Psychological Association, and ecoAmerica, Washington, DC. 69 pp.
Clow, K.M., et al., 2017: Northward range expansion of Ixodes scapularis evident over a short timescale in Ontario, Canada. Plos One, 12 (12), doi:10.1371/journal.pone.0189393.
Cohen, B., E. Tyler and T. Gunfas, 2017: Lessons from co-impacts assessment under the Mitigation Action Plans and Scenarios (MAPS) Programme. Clim. Policy, 17 (8), 1065–1075, doi:10.1080/14693062.2016.1222258.
Collaco, J.M., L.J. Appel, J. McGready and G.R. Cutting, 2018: The relationship of lung function with ambient temperature. PLoS ONE, 13 (1), e191409, doi:10.1371/journal.pone.0191409.
Colon-Gonzalez, F., C. Fezzi, I. Lake and P. Hunter, 2013: The effects of weather and climate change on dengue. PLoS Negl. Trop. Dis. , 7 (11), doi:10.1371/journal.pntd.0002503.
Confalonieri, U., J.A. Menezes and C. Margonari, 2017: Environmental change and the emergence of infectious diseases: a regional perspective from South America. In: Examining the Role of Environmental Change on Emerging Infectious Diseases and Pandemics, pp. 109–137. IGI Global, Hershey PA.
Confalonieri, U. E., J.A. Menezes and C. Margonari de Souza, 2015: Climate change and adaptation of the health sector: the case of infectious diseases. Virulence, 6 (6), 554–557, doi:10.1080/21505594.2015.1023985.
Coniglio, N.D. and G. Pesce, 2015: Climate variability and international migration: an empirical analysis. Envir. Dev. Econ. , 20 (4), 438–468.
Connell, J., 2016: Last days in the Carteret Islands? Climate change, livelihoods and migration on coral atolls. Asia Pac. Viewp. , 57 (1), 3–15.
Connolly, M., 2013: Some like it mild and not too wet: the influence of weather on subjective well-being. J. Happiness Stud. , 14 (2), 457–473, doi:10.1007/s10902-012-9338-2.
Corvalan, C., et al., 2020: Towards climate resilient and environmentally sustainable health care facilities. Int. J. Environ. Res. Public Health, 17 (23), doi:10.3390/ijerph17238849.
Costa, A. F., G. Hoek, B. Brunekreef and A. de Leon, 2017: Air pollution and deaths among elderly residents of Sao Paulo, Brazil: an analysis of mortality displacement. Environ. Health Perspect. , 125 (3), 349–354, doi:10.1289/ehp98.
Coughlan de Perez, E., et al., 2021: Epidemiological versus meteorological forecasts: best practice for linking models to policy making. Int. J. Forecast . DOI: https://doi.org/10.1016/j.ijforecast.2021.08.003
Crawford, A. and C. Church, 2020: The NAP Process and Peacebuilding. NAP Global Network Briefing Note. International Institute for Sustainable Development (IISD), Geneva.
Crawford, A., et al., 2015: Promoting Climate-resilient Peacebuilding in Fragile States. International Institute for Sustainable Development (IISD), Geneva.
Cromar, K.R., M. Ghazipura, L.A. Gladson and L. Perlmutt, 2020: Evaluating the US Air Quality Index as a risk communication tool: comparing associations of index values with respiratory morbidity among adults in California. PLoS ONE, 15 (11), doi:10.1371/journal.pone.0242031.
Cunado, J. and F.P. de Gracia, 2013: Environment and happiness: new evidence for Spain. Soc. Indic. Res. , 112 (3), 549–567, doi:10.1007/s11205-012-0038-4.
Cundill, G., et al., 2021: Toward a climate mobilities research agenda: intersectionality, immobility, and policy responses. Glob. Environ. Change, 69. DOI: https://doi.org/10.1016/j.gloenvcha.2021.102315 Available at: https://www.sciencedirect.com/science/article/pii/S0959378021000947.
Cunsolo, A., et al., 2020: “You can never replace the caribou”: Inuit experiences of ecological grief from caribou declines. Am. Imago, 77 (1), 31–59, doi:10.1353/aim.2020.0002.
Cunsolo, A. and N.R. Ellis, 2018: Ecological grief as a mental health response to climate change-related loss. Nat. Clim. Change, 8 (4), 275–281, doi:10.1038/s41558-018-0092-2.
Cunsolo Willox, A., et al., 2013: Climate change and mental health: an exploratory case study from Rigolet, Nunatsiavut, Canada. Clim. Change, 121 (2), 255–270.
Cunsolo Willox, A., et al., 2015: Examining relationships between climate change and mental health in the Circumpolar North. Reg. Environ. Change, 15 (1), 169–182.
Curriero, F.C., J.A. Patz, J.B. Rose and S. Lele, 2001: The association between extreme precipitation and waterborne disease outbreaks in the United States, 1948–1994. Am. J. Public Health, 91 (8), 1194–1199, doi:10.2105/ajph.91.8.1194.
Curtis, K., E. Fussell and J. DeWaard, 2015: Recovery migration after Hurricanes Katrina and Rita: spatial concentration and intensification in the migration system. Demography, 52 (4), 1269–1293.
Curtis, S., et al., 2017: Impact of extreme weather events and climate change for health and social care systems. Environ. Health, 16, 23–32, doi:10.1186/s12940-017-0324-3.
Cusack, L., C. de Crespigny and P. Athanasos, 2011: Heatwaves and their impact on people with alcohol, drug and mental health conditions: a discussion paper on clinical practice considerations. J. Adv. Nurs. , 67 (4), 915–922, doi:10.1111/j.1365-2648.2010.05551.x.
D’Amato, G., et al., 2020: The effects of climate change on respiratory allergy and asthma induced by pollen and mold allergens. Allergy, 75 (9), 2219–2228, doi:10.1111/all.14476.
D’Odorico, P., et al., 2018: The global food-energy-water nexus. Rev. Geophys. , 56 (3), 456–531.
Dahl, K., R. Licker, J.T. Abatzoglou and J. Declet-Barreto, 2019: Increased frequency of and population exposure to extreme heat index days in the United States during the 21st century. Environ. Res. Commun. , 1 (7), doi:10.1088/2515-7620/ab27cf.
Damschroder, L.J., et al., 2009: Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement. Sci. , 4 (1), 50.
Daniel, M., et al., 2018: Increased relative risk of tick-borne encephalitis in warmer weather. Front. Cell. Infect. Microbiol. , 8, doi:10.3389/fcimb.2018.00090.
Dannenberg, A., H. Frumkin, J. Hess and K. Ebi, 2019: Managed retreat as a strategy for climate change adaptation in small communities: public health implications. Clim. Change, 153 (1-2), 1–14, doi:10.1007/s10584-019-02382-0.
Dar, O., et al., 2014: Integrating health into disaster risk reduction strategies: key considerations for success. Am. J. Public Health, 104 (10), 1811–1816, doi:10.2105/ajph.2014.302134.
Dasandi, N., H. Graham, P. Lampard and S. Mikhaylov, 2021: Engagement with health in national climate change commitments under the Paris Agreement: a global mixed-methods analysis of the nationally determined contributions. Lancet Planet. Health, 5 (2), 93–101.
David-Chavez, D. and M. Gavin, 2018: A global assessment of Indigenous community engagement in climate research. Environ. Res. Lett. , 13 (12), doi:10.1088/1748-9326/aaf300.
Davies, M., et al., 2013: Promoting resilient livelihoods through adaptive social protection: lessons from 124 programmes in South Asia. Dev. Policy Rev. , 31, doi:10.1111/j.1467-7679.2013.00600.x.
Davis, R.E., et al., 2016: Cold, dry air is associated with influenza and pneumonia mortality in Auckland, New Zealand. Influenza Other Respi. Viruses, 10 (4), 310–313, doi:10.1111/irv.12369.
Day, A. and J. Caus, 2020: Conflict Prevention in the Era of Climate Change: Adapting the UN to Climate-Security Risks. United Nations University, New York, ISBN 978-9280865141.
De’Donato, F., et al., 2018: Temporal variation in the effect of heat and the role of the Italian heat prevention plan. Public Health, 161, 154–162, doi:10.1016/j.puhe.2018.03.030.
De Châtel, F., 2014: The role of drought and climate change in the Syrian uprising: untangling the triggers of the revolution. Middle East. Stud. , 50 (4), 521–535.
De Dominicis, S., et al., 2015: We are at risk, and so what? Place attachment, environmental risk perceptions and preventive coping behaviours. J. Environ. Psychol. , 43, 66–78.
De Juan, A., 2015: Long-term environmental change and geographical patterns of violence in Darfur, 2003–2005. Polit. Geogr. , 45, 22–33.
de la Vega-Leinert, A.C., S. Stoll-Kleemann and E. Wegener, 2018: Managed realignment (MR) along the Eastern German Baltic Sea: a catalyst for conflict or for a coastal zone management consensus. J. Coast. Res. , 34 (3), 586–601, doi:10.2112/jcoastres-d-15-00217.1.
de Leon-Martinez, L., et al., 2020: Critical review of social, environmental and health risk factors in the Mexican indigenous population and their capacity to respond to the COVID-19. Sci. Total Environ. , 733, doi:10.1016/j.scitotenv.2020.139357.
de Lima, C., et al., 2021: Heat stress on agricultural workers exacerbates crop impacts of climate change. Environ. Res. Lett. , 16 (4), doi:10.1088/1748-9326/abeb9 f.
De Neve, J.-E., E. Diener, L. Tay and C. Xuereb, 2013: The objective benefits of subjective well-being. In: World Happiness Report 2013[Helliwell, J.L.R. and J. e. Sachs(eds.)]. UN Sustainable Development Solutions Network, New York (Available at: https://ssrn.com/abstract=2306651).
Defor, A. and T.V. Oheneba-Dornyo, 2020: Is climate change hampering global health security? A review of the evidence. School of Diplomacy and International Relations Seton Hall University, New Jersey.
Degen, A. and S. El-Meccawi, 2009: Livestock production among urban Negev Bedouin. Outlook Agric. , 38 (4), 327–335, doi:10.5367/000000009790422106.
Delhey, J. and G. Dragolov, 2016: Happier together. Social cohesion and subjective well-being in Europe. Int. J. Psychol. , 51 (3), 163–176, doi:10.1002/ijop.12149.
Dellink, R., J. Chateau, E. Lanzi and B. Magné, 2017: Long-term economic growth projections in the Shared Socioeconomic Pathways. Glob. Environ. Change, 42, 200–214.
Demain, J., 2018: Climate change and the impact on respiratory and allergic disease: 2018. Curr. Allergy Asthma Rep. , 18 (4), 1–5, doi:10.1007/s11882-018-0777-7.
Deng, S.Z., et al., 2020: Climate change, air pollution, and allergic respiratory diseases: a call to action for health professionals. Chin. Med. J. , 133 (13), 1552–1560, doi:10.1097/cm9.0000000000000861.
Dennekamp, M., et al., 2015: Forest fire smoke exposures and out-of-hospital cardiac arrests in Melbourne, Australia: a case-crossover study. Environ. Health Perspect. , 123 (10), 959–964, doi:10.1289/ehp.1408436.
Desai, B., et al., 2021: Addressing the human cost in a changing climate. Science, 372 (6548), 1284–1287. Available at: http://science.sciencemag.org/content/372/6548/1284.abstract.
Deshpande, A., H.H. Chang and K. Levy, 2020: Heavy rainfall events and diarrheal diseases: the role of urban-rural geography. Am. J. Trop. Med. Hyg. , 103 (3), 1043–1049, doi:10.4269/ajtmh.19-0768.
Deslatte, A., 2020: The erosion of trust during a global pandemic and how public administrators should counter it. Am. Rev. Public Adm. , 50 (6-7), 489–496, doi:10.1177/0275074020941676.
DeWaard, J., K.J. Curtis and E. Fussell, 2016: Population recovery in New Orleans after Hurricane Katrina: exploring the potential role of stage migration in migration systems. Popul. Environ. , 37 (4), 449–463, doi:10.1007/s11111-015-0250-7.
Deyle, E.R., et al., 2016: Global environmental drivers of influenza. Proc. Natl. Acad. Sci. U.S.A. , 113 (46), 13081–13086, doi:10.1073/pnas.1607747113.
Dialesandro, J., N. Brazil, S. Wheeler and Y. Abunnasr, 2021: Dimensions of thermal inequity: neighborhood social demographics and urban heat in the southwestern US. Int. J. Environ. Res. Public Health, 18 (3), doi:10.3390/ijerph18030941.
Diaz-Mendez, S.E., et al., 2018: Economic, environmental and health co-benefits of the use of advanced control strategies for lighting in buildings of Mexico. Energy Policy, 113, 401–409, doi:10.1016/j.enpol.2017.11.028.
Diaz, D.B., 2016: Estimating global damages from sea level rise with the Coastal Impact and Adaptation Model (CIAM). Clim. Change, 137 (1), 143–156.
Diaz, J., et al., 2018: Time trend in the impact of heat waves on daily mortality in Spain for a period of over thirty years (1983–2013). Environ. Int. , 116, 10–17, doi:10.1016/j.envint.2018.04.001.
Diaz, J., et al., 2019: Time trends in the impact attributable to cold days in Spain: incidence of local factors. Sci. Total Environ. , 655, 305–312, doi:10.1016/j.scitotenv.2018.11.254.
Diaz, J., et al., 2015: Comparison of the effects of extreme temperatures on daily mortality in Madrid (Spain), by age group: the need for a cold wave prevention plan. Environ. Res. , 143 (Pt A), 186–191, doi:10.1016/j.envres.2015.10.018.
Dicker, D., et al., , 2018a: Global, regional, and national age-sex-specific mortality and life expectancy, 1950–2017: a systematic analysis for the Global Burden of Disease Study 2017. The Lancet, 392 (10159), 1684–1735, doi:10.1016/S0140-6736(18)31891-9.
Diener, E. and L. Tay, 2015: Subjective well-being and human welfare around the world as reflected in the Gallup World Poll. Int. J. Psychol. , 50 (2), 135–149, doi:10.1002/ijop.12136.
Dillender, M., 2021: Climate change and occupational health are there limits to our ability to adapt?J. Hum. Resour. , 56 (1), 184–224, doi:10.3368/jhr.56.1.0718-9594R3.
Dilling, L., et al., 2017: Drivers of adaptation: responses to weather- and climate-related hazards in 60 local governments in the Intermountain Western U.S. Environ. Plan. A, 49 (11), 2628–2648, doi:10.1177/0308518x16688686.
Dimitrova, A., et al., 2021: Association between ambient temperature and heat waves with mortality in South Asia: systematic review and meta-analysis. Environ. Int. , 146, doi:10.1016/j.envint.2020.106170.
Dinar, S., D. Katz, L. De Stefano and B. Blankespoor, 2015: Climate change, conflict, and cooperation: global analysis of the effectiveness of international river treaties in addressing water variability. Polit. Geogr. , 45, 55–66.
Ding, H.L., H.J. Li and N.N. Sze, 2021: Effects of the abolishment of London western charging zone on traffic flow and vehicle emissions. Int. J. Sustain. Transp. , doi:10.1080/15568318.2021.1914790.
Djennad, A., et al., 2019: Seasonality and the effects of weather on Campylobacter infections. BMC Infect. Dis. , 19 (1), 255, doi:10.1186/s12879-019-3840-7.
Djoudi, H., et al., 2016: Beyond dichotomies: gender and intersecting inequalities in climate change studies. Ambio, 45 (3), S248–S262.
Doan, V.Q. and H. Kusaka, 2018: Projections of urban climate in the 2050s in a fast-growing city in Southeast Asia: the greater Ho Chi Minh City metropolitan area, Vietnam. Int. J. Climatol. , 38 (11), 4155–4171, doi:10.1002/joc.5559.
Dockery, A., 2020: Inter-generational transmission of indigenous culture and children’s wellbeing: evidence from Australia. Int. J. Intercult. Relat. , 74, 80–93, doi:10.1016/j.ijintrel.2019.11.001.
Dodd, W., et al., 2018: The summer of smoke: ecosocial and health impacts of a record wildfire season in the Northwest Territories, Canada. Lancet Glob. Health, 6, S30–S30, doi:10.1016/s2214-109x(18)30159-1.
Dodd, W., et al., 2017: Determinants of internal migrant health and the healthy migrant effect in South India: a mixed methods study. BMC Int. Health Hum. Rights, 17, doi:10.1186/s12914-017-0132-4.
Dodds, K., et al., 2020: The COVID-19 pandemic: territorial, political and governance dimensions of the crisis. Territ. Polit. Gov. , 8 (3), 289–298, doi:10.1080/21622671.2020.1771022.
Doherty, R.M., M.R. Heal and F.M. O’Connor, 2017: Climate change impacts on human health over Europe through its effect on air quality. Environ. Health, 16, 33–44, doi:10.1186/s12940-017-0325-2.
Dombrowsky, I., 2010: The role of intra-water sector issue linkage in the resolution of transboundary water conflicts. Water Int. , 35 (2), 132–149.
Domínguez-Morueco, N., et al., 2019: Combining monitoring and modelling approaches for BaP characterization over a petrochemical area. Sci. Total Environ. , 658, 424–438, doi:10.1016/j.scitotenv.2018.12.202.
Donatuto, J., L. Campbell and W. Trousdale, 2020: The “value” of values-driven data in identifying Indigenous health and climate change priorities. Clim. Change, 158 (2), 161–180, doi:10.1007/s10584-019-02596-2.
Dong, C., et al., 2019: Wastewater treatment in amine-based carbon capture. Chemosphere, 222, 742–756, doi:10.1016/j.chemosphere.2019.01.038.
Dosio, A., L. Mentaschi, E. Fischer and K. Wyser, 2018: Extreme heat waves under 1.5°C and 2°C global warming. Environ. Res. Lett. , 13, doi:10.1088/1748-9326/aab827.
DPPA, UNDP and UNEP, 2020: United Nations Climate Security Mechanism Toolbox Briefing Note. Climate Security Mechanism, New York.
Dresse, A., I. Fischhendler, J.Ø. Nielsen and D. Zikos, 2019: Environmental peacebuilding: towards a theoretical framework. Coop. Confl. , 54 (1), 99–119.
Drewnowski, A., et al., 2020: Toward healthy diets from sustainable food systems. Curr. Dev. Nutr. , 4 (6), doi:10.1093/cdn/nzaa083.
Duane, B., et al., 2019: Environmentally sustainable dentistry: a brief introduction to sustainable concepts within the dental practice. Br. Dent. J. , 226, 292–295, doi:10.1038/s41415-019-0010-7.
Duarte, J.L., F.A. Diaz-Quijano, A.C. Batista and L.L. Giatti, 2019: Climatic variables associated with dengue incidence in a city of the Western Brazilian Amazon region. Rev. Soc. Bras. Med. Trop. , 52, e20180429, doi:10.1590/0037-8682-0429-2018.
Dube, E. and E. Munsaka, 2018: The contribution of indigenous knowledge to disaster risk reduction activities in Zimbabwe: a big call to practitioners. Jamba J. Disaster Risk Stud. , 10, doi:10.4102/jamba.v10i1.493.
Dudgeon, P., A. Bray, B. D’Costa and R. Walker, 2017: Decolonising psychology: validating social and emotional wellbeing. Aust. Psychol. , 52 (4), 316–325, doi:10.1111/ap.12294.
Dudley, J.P., E.P. Hoberg, E.J. Jenkins and A.J. Parkinson, 2015: Climate change in the North American Arctic: a one health perspective. EcoHealth, 12 (4), 713–725, doi:10.1007/s10393-015-1036-1.
Dumic, I. and E. Severnini, 2018: “Ticking bomb”: the impact of climate change on the incidence of Lyme disease. Can. J. Infect. Dis. Med. Microbiol. , 5719081, doi:10.1155/2018/5719081.
Dunn, H. and R. Matthew, 2015: Natural resources and gender in conflict settings. Peace Rev. J. Soc. Justice, 27 (2), 156–164, doi:10.1080/10402659.2015.1037619.
Durkalec, A., C. Furgal, M. Skinner and T. Sheldon, 2015: Climate change influences on environment as a determinant of indigenous health: relationships to place, sea ice, and health in an Inuit community. Soc. Sci. Med. , 136, 17–26.
Ebi, K., 2011: Climate change and health risks: assessing and responding to them through ‘adaptive management’. Health Aff. , 30 (5), 924–930, doi:10.1377/hlthaff.2011.0071.
Ebi, K., 2016: Adaptation and resilience. Public Health Rev. , 37, doi:10.1186/s40985-016-0032-5.
Ebi, K., et al., 2020: Using detection and attribution to quantify how climate change is affecting health. Health Aff. , 39 (12), 2168–2174, doi:10.1377/hlthaff.2020.01004.
Ebi, K., et al., 2018a: Stress testing the capacity of health systems to manage climate change-related shocks and stresses. Int. J. Environ. Res. Public Health, 15 (11), doi:10.3390/ijerph15112370.
Ebi, K., et al., 2018b: Health risks of warming of 1.5 degrees C, 2 degrees C, and higher, above pre-industrial temperatures. Environ. Res. Lett. , 13 (6), doi:10.1088/1748-9326/aac4bd.
Ebi, K., et al., 2021a: Burning embers: synthesis of the health risks of climate change. Environ. Res. Lett. , 16 (4), doi:10.1088/1748-9326/abeadd.
Ebi, K., et al., 2021b: Interactions between two existential threats: COVID-19 and climate change, Clim Risk Manag, doi: 10.1016/j.crm.2021.100363
Ebi, K. and J. Hess, 2020: Health risks due to climate change: inequity in causes and consequences. Health Aff. , 39 (12), 2056–2062, doi:10.1377/hlthaff.2020.01125.
Ebi, K. and I. Loladze, 2019: Elevated atmospheric CO2 concentrations and climate change will affect our food’s quality and quantity. Lancet Planet. Health, 3 (7), E283–E284, doi:10.1016/s2542-5196(19)30108-1. Comment.
Ebi, K., 2019: Effective heat action plans: research to interventions. Environ. Res. Lett. , 14 (12), doi:10.1088/1748-9326/ab5ab0.
Ebi, K., N.H. Ogden, J.C. Semenza and A. Woodward, 2017: Detecting and attributing health burdens to climate change. Environ. Health Perspect. , 125 (8), 85004, doi:10.1289/EHP1509.
Ebi, K. and M. Otmani del Barrio, 2017: Lessons learned on health adaptation to climate variability and change: experiences across low- and middle-income countries. Environ. Health Perspect. , 125 (6), doi:10.1289/EHP405.
Ebrahim, S., et al., 2020: Forward planning for disaster-related mass gatherings amid COVID-19. Lancet Planet. Health, 4 (9), E379–E380, doi:10.1016/s2542-5196(20)30175-3.
Echenique, M. and L. Melgar, 2018: Mapping Puerto Rico’s Hurricane Migration With Mobile Phone Data.Publisher name: Bloomberg City Lab URL: https://www.bloomberg.com/news/articles/2018-05-11/where-puerto-rico-s-residents-migrated-since-maria. Last accessed 3 September 2021.
Eckstein, D., V. Künzel and L. Schäfer, 2017: Global Climate Risk Index 2018. Germanwatch eV, Bonn, Germany. London, UK. 93 pp.
Edmonds, D.A., R. L. Caldwell, E. S. Brondizio and S. M. O. Siani, 2020: Coastal flooding will disproportionately impact people on river deltas. Nat. Commun. , 11 (1), 4741, doi:10.1038/s41467-020-18531-4.
Edwards, B., M. Gray and B. Hunter, 2015: The impact of drought on mental health in rural and regional Australia. Soc. Indic. Res. , 121 (1), 177–194, doi:10.1007/s11205-014-0638-2.
Efstratiou, A., J. Ongerth and P. Karanis, 2017: Waterborne transmission of protozoan parasites: review of worldwide outbreaks – an update 2011–2016. Water Res. , 114, 14–22, doi:10.1016/j.watres.2017.01.036.
Eguiluz-Gracia, I., et al., 2020: The need for clean air: the way air pollution and climate change affect allergic rhinitis and asthma. Allergy, 75 (9), 2170–2184, doi:10.1111/all.14177.
Eisenman, D., S. McCaffrey, I. Donatello and G. Marshal, 2015: An ecosystems and vulnerable populations perspective on solastalgia and psychological distress after a wildfire. EcoHealth, 12 (4), 602–610.
Ekstrom, J.A. and L. Bedsworth, 2018: Adapting air quality management for a changing climate: survey of local districts in California. J. Air Waste Manag. Assoc. , 68 (9), 931–944, doi:10.1080/10962247.2018.1459325.
El-Zein, A. and F.N. Tonmoy, 2017: Nonlinearity, fuzziness and incommensurability in indicator-based assessments of vulnerability to climate change: a new mathematical framework. Ecol. Indic. , 82, 82–93.
Ellis, N.R. and G.A. Albrecht, 2017: Climate change threats to family farmers’ sense of place and mental wellbeing: a case study from the Western Australian Wheatbelt. Soc. Sci. Med. , 175, 161–168, doi:10.1016/j.socscimed.2017.01.009.
Emmerson, K.M., et al., 2021: Atmospheric modelling of grass pollen rupturing mechanisms for thunderstorm asthma prediction. PLoS ONE, 16 (4), doi:10.1371/journal.pone.0249488.
Ensor, J., J. Forrester and N. Matin, 2018: Bringing rights into resilience: revealing complexities of climate risks and social conflict. Disasters, 42, S287–S305.
Epstein, A., et al., 2020a: Drought and intimate partner violence towards women in 19 countries in sub-Saharan Africa during 2011–2018: a population-based study. PLoS Med, 17 (3), e1003064, doi:10.1371/journal.pmed.1003064.
Epstein, A., T. Benmarhnia and S.D. Weiser, 2020b: Drought and illness among young children in Uganda, 2009–2012. Am. J. Trop. Med. Hyg. , 102 (3), 644–648, doi:10.4269/ajtmh.19-0412.
Epstein, Y. and R. Yanovich, 2019: Heatstroke. N. Engl. J. Med. , 380 (25), 2449–2459, doi:10.1056/NEJMra1810762.
Eriksen, S., A. Nightingale and H. Eakin, 2015: Reframing adaptation: the political nature of climate change adaptation. Glob. Environ. Change, 35, 523–533.
Eriksen, S., et al., 2021: Adaptation interventions and their effect on vulnerability in developing countries: help, hindrance or irrelevance?World Dev. , 141, doi:10.1016/j.worlddev.2020.105383.
Escobar, L.E., et al., 2015: A global map of suitability for coastal Vibrio cholerae under current and future climate conditions. Acta Trop. , 149, 202–211, doi:10.1016/j.actatropica .2015.05.028.
Espejo, W., J. Celis, G. Chiang and P. Bahamonde, 2020: Environment and COVID-19: pollutants, impacts, dissemination, management and recommendations for facing future epidemic threats. Sci. Total Environ. , 747, doi:10.1016/j.scitotenv.2020.141314.
Estrada-Peña, A. and N. Fernández-Ruiz, 2020: A retrospective assessment of temperature trends in Northern Europe reveals a deep impact on the life cycle of Ixodes ricinus (Acari: Ixodidae). Pathogens, 9 (5), doi:10.3390/pathogens9050345.
European Environmental Agency 2017: Climate Change, Impacts and Vulnerability in Europe 2016: An Indicator-based Report . Publications office of the European Union, Luexembourg. 419 pp.
European Food Safety Authority (EFSA), 2020: Climate Change as a Driver of Emerging Risks for Food and Feed Safety, Plant, Animal Health and Nutritional Quality. EFSA (European Food Safety Authority), 1–146. doi:10.2903/sp.efsa.2020.EN-1881
Evangeliou, N., et al., 2014: Wildfires in Chernobyl-contaminated forests and risks to the population and the environment: a new nuclear disaster about to happen?Environ. Int. , 73, 346–358, doi:10.1016/j.envint.2014.08.012.
Evans, G., 2019: Projected behavioral impacts of global climate change. Annu. Rev. Psychol. , 70, 449–474, doi:10.1146/annurev-psych-010418-103023.
Evertsen, K. and K. Van Der Geest, 2019: Gender, environment and migration in Bangladesh. Clim. Dev. , doi:10.1080/17565529.2019.1596059.
Ezeh, A., F. Kissling and P. Singer, 2020: Why sub-Saharan Africa might exceed its projected population size by 2100. Lancet , 396 (10258), 1131–1133, doi:10.1016/s0140-6736(20)31522-1.
Fan, J. and Q. Liu, 2019: Potential impacts of climate change on dengue fever distribution using RCP scenarios in China. Adv. Clim. Change Res. , 10 (1), 1–8, doi:10.1016/j.accre.2019.03.006.
Fan, Y., et al., 2021: Molecular characterization of the waterborne pathogens Cryptosporidium spp., Giardia duodenalis, Enterocytozoon bieneusi, Cyclospora cayetanensis and Eimeria spp. in wastewater and sewage in Guangzhou, China. Parasit Vectors, 14 (1), 66, doi:10.1186/s13071-020-04566-5.
Fanzo, J., et al., 2020: Nutrients, foods, diets, people: promoting healthy eating. Curr. Dev. Nutr. , 4 (6), doi:10.1093/cdn/nzaa069.
FAO, 2020: Climate Change: Unpacking the Burden on Food Safety. Food Safety and Quality Series. Food and Agriculture Organization of the United Nations, Rome, Italy.
FAO and Alliance of Biodiversity International and CIAT, 2021: Indigenous Peoples’ Food Systems: Insights on Sustainability and Resilience from the Front Line of Climate Change. FAO, Rome
FAO, et al., 2018: The State of Food Security and Nutrition in the World 2018. Building Climate Resilience for Food Security and Nutrition. Policy Support and Governance, Fao, Rome, http://www.fao.org/3/I9553EN/i9553en.pdf. Last accessed 3 September 2021.
FAO, et al., 2020: The State of Food Security and Nutrition in the World 2020. Transforming Food Systems for Affordable Healthy Diets. Fao, Rome, http://www.fao.org/3/ca9692en/ca9692en.pdf. Last accessed 3 September 2021.
FAO, et al., 2021: The State of Food Security and Nutrition in the World 2021. Transforming Food Systems for Food Security, Improved Nutrition and Affordable Healthy Diets for All. FAO, Rome.
FAO and WHO, 2018: Evaluation of Certain Veterinary Drug Residues in Food: Eighty-Fifth Report of the Joint FAO/WHO Expert Committee on Food Additives. World Health Organization, Geneva, Switzerland, Vol. 1008, 1–150.
FAOLEX, 2021: Plant Protection (Damage by Goats) Law, 1950. https://www.ecolex.org/details/legislation/plant-protection-damage-by-goats-law-1950-lex-faoc014270/ Last accessed 3 September 2021.
Farbotko, C., et al., 2020: Relocation planning must address voluntary immobility. Nat. Clim. Change, 10 (8), 702–704, doi:10.1038/s41558-020-0829-6.
Farbotko, C. and C. McMichael, 2019: Voluntary immobility and existential security in a changing climate in the Pacific. Asia Pac. Viewp. , 60, 148–162, doi:10.1111/apv.12231.
Farchi, S., et al., 2017: Meat consumption reduction in Italian regions: health co-benefits and decreases in GHG emissions. PLoS ONE, 12 (8), doi:10.1371/journal.pone.0182960.
Farhat, J.B., et al., 2018: Syrian refugees in Greece: experience with violence, mental health status, and access to information during the journey and while in Greece. BMC Med. , 1–12. DOI: https://doi.org/10.1186/s12916-018-1028-4
Fatehpanah, A., et al., 2020: Water safety in drought: an indigenous knowledge-based qualitative study. J. Water Health, 18 (5), 692–703, doi:10.2166/wh.2020.141.
Fawcett, D., T. Pearce, J.D. Ford and L. Archer, 2017: Operationalizing longitudinal approaches to climate change vulnerability assessment. Glob. Environ. Change, 45, 79–88.
Fazey, I., et al., 2016: Past and future adaptation pathways. Clim. Dev. , 8 (1), 26–44, doi:10.1080/17565529.2014.989192.
Fei, L., et al., 2015: Population change of farmland rodent and the influences of climate and cultivation factors in Fengxian District of Shanghai, China. Ying Yong Sheng Tai Xue Bao J. Appl. Ecol. , 26 (2), 579–587.
Fenech, S., et al., 2019: Meteorological drivers and mortality associated with O-3 and PM2.5 air pollution episodes in the UK in 2006. Atmosph. Environ. , 213, 699–710, doi:10.1016/j.atmosenv.2019.06.030.
Ferkol, T. and D. Schraufnagel, 2014: The global burden of respiratory disease. Ann. Am. Thorac. Soc. , 11 (3), 404–406, doi:10.1513/AnnalsATS.201311-405 PS.
Fernandez, A., et al., 2015: Flooding and mental health: a systematic mapping review. PLoS ONE, 10 (4), doi:10.1371/journal.pone.0119929.
Ferreira-Coimbra, J., C. Sarda and J. Rello, 2020: Burden of community-acquired pneumonia and unmet clinical needs. Adv. Ther. , 37 (4), 1302–1318, doi:10.1007/s12325-020-01248-7.
Ferreira, D.C., I. Graziele, R.C. Marques and J. Gonçalves, 2021: Investment in drinking water and sanitation infrastructure and its impact on waterborne diseases dissemination: the Brazilian case. Sci. Total Environ. , 779, 146279, doi:10.1016/j.scitotenv.2021.146279.
Flahault, A., R.R. de Castaneda and I. Bolon, 2016: Climate change and infectious diseases. Public Health Rev. , 37, doi:10.1186/s40985-016-0035-2.
Flatø, M., R. Muttarak and A. Pelser, 2017: Women, weather, and woes: the triangular dynamics of female-headed households, economic vulnerability, and climate variability in South Africa. World Dev. , 90, 41–62.
Fogg-Rogers, L., et al., 2021: Applying social learning to climate communications – visualising ‘people like me’ in air pollution and climate change data. Sustainability, 13 (6), doi:10.3390/su13063406.
Folkerts, M. A., et al., 2020: Long term adaptation to heat stress: shifts in the minimum mortality temperature in the Netherlands. Front. Physiol. , 11, doi:10.3389/fphys.2020.00225.
Follos, F., et al., 2021: Evolution of the minimum mortality temperature (1983–2018): Is Spain adapting to heat?Sci. Total Environ. , 784, doi:10.1016/j.scitotenv.2021.147233.
Ford, J. and D. King, 2015: A framework for examining adaptation readiness. Mitigation and Adaptation Strategies for Global Change, 20 pp. 505-526.
Ford, J., et al., 2020: The resilience of indigenous peoples to environmental change. One Earth, 2 (6), 532–543, doi:10.1016/j.oneear.2020.05.014.
Ford, J.D., et al., 2018: Preparing for the health impacts of climate change in indigenous communities: the role of community-based adaptation. Glob. Environ. Change, 49, 129–139, doi:10.1016/j.gloenvcha.2018.02.006.
Ford, T.E. and S. Hamner, 2018: A perspective on the global pandemic of waterborne disease. Microb. Ecol. , 76 (1), 2–8, doi:10.1007/s00248-015-0629-0.
Foreman, K.J., et al., 2018: Forecasting life expectancy, years of life lost, and all-cause and cause-specific mortality for 250 causes of death: reference and alternative scenarios for 2016–40 for 195 countries and territories. Lancet , 392 (10159), 2052–2090, doi:10.1016/s0140-6736(18)31694-5.
Foster, J., S.G. Hodder, J. Goodwin and G. Havenith, 2020: Occupational heat stress and practical cooling solutions for healthcare and industry workers during the COVID-19 pandemic. Ann. Work Expo. Health, 64 (9), 915–922, doi:10.1093/annweh/wxaa082.
Foudi, S., N. Osés-Eraso and I. Galarraga, 2017: The effect of flooding on mental health: lessons learned for building resilience. Water Resour. Res. , 53 (7), 5831–5844.
Fox, M., et al., 2019: Integrating public health into climate change policy and planning: state of practice update. Int. J. Environ. Res. Public Health, 16 (18), doi:10.3390/ijerph16183232.
Froese, R. and J. Schilling, 2019: The nexus of climate change, land use, and conflicts. Curr. Clim. Change Rep. , 5 (1), 24–35.
Fröhlich, C. and G. Gioli, 2015: Gender, conflict, and global environmental change. Peace Rev. J. Soc. Justice, 27 (2), 137–146, doi:10.1080/10402659.2015.1037609.
Fröhlich, C., G. Gioli, R. Cremades and H. Myrttinen, 2018: Water Security Across the Gender Divide. Springer, Dordrecht, ISBN 978-3319640464.
Fröhlich, C.J., 2016: Climate migrants as protestors? Dispelling misconceptions about global environmental change in pre-revolutionary Syria. Contemp. Levant , 1 (1), 38–50.
Frumkin, H., 2018: The US health care sector’s carbon footprint: stomping or treading lightly?Am. J. Public Health, 108 (S2), S56–S57, doi:10.2105/ajph.2017.304160.
Frumkin, H. and A. Haines, 2019: Global environmental change and noncommunicable disease risks. Annu. Rev. Public Health, 40 (1), 261–282, doi:10.1146/annurev-publhealth-040218-043706.
FSIN, 2020: Global Report on Food Crises: Joint Analysis for Better Decisions. Food and Agriculture Organization (FAO); World Food Programme (WFP); and International Food Policy Research Institute (IFPRI), Rome, Italy and Washington, DC
FSIN and GNAFC, 2020: Global Report on Food Crises 2020. Food Security Information Network and Global Network Against Food Crises, FSIN/GNAFC, Rome.
Fu, T.M. and H. Tian, 2019: Climate change penalty to ozone air quality: review of current understandings and knowledge gaps. Curr. Pollut. Rep. , 5 (3), 159–171, doi:10.1007/s40726-019-00115-6.
Fuentes, L., H. Asselin, A. Belisle and O. Labra, 2020: Impacts of environmental changes on well-being in indigenous communities in eastern Canada. Int. J. Environ. Res. Public Health, 17 (2), 11, doi:10.3390/ijerph17020637.
Fujii, H., et al., 2015: Fatigue and sleep under large summer temperature differences. Environ. Res. , 138, 17–21, doi:10.1016/j.envres.2015.02.006.
Fullilove, M.T., 1996: Psychiatric implications of displacement: contributions from the psychology of place. Am. J. Psychiatry, 153, 1516–1523.
Fullman, N., et al., 2017: Measuring progress and projecting attainment on the basis of past trends of the health-related Sustainable Development Goals in 188 countries: an analysis from the Global Burden of Disease Study 2016. Lancet , 390 (10100), 1423–1459, doi:10.1016/s0140-6736(17)32336-x.
Fummi, M., J. Andries and B. Yonas, 2017: The role of indigenous knowledge in drought risk reduction: a case of communal farmers in South Africa. J. Disaster Risk Stud. , 9, 1–6, doi:10.4102/jamba.v9i1.420.
Funk, C., et al., 2018: Contrasting Kenyan Resilience to Drought: 2011 and 2017. US AID, https://www.usaid.gov/sites/default/files/documents/1867/Kenya_Report_-_Full_Compliant.PDF. (Special Report ed., Aid, U. S., USA, 20 pp). Last accessed 3 September 2021.
Funk, C., et al., 2019: Recognizing the famine early warning systems network: over 30 years of drought early warning science advances and partnerships promoting global food security. Bull. Am. Meteorol. Soc. , 100 (6), 1011–1027, doi:10.1175/bams-d-17-0233.1.
Furberg, M., B. Evengard and M. Nilsson, 2011: Facing the limit of resilience: perceptions of climate change among reindeer herding Sami in Sweden. Glob. Health Action, 4, doi:10.3402/gha.v4i0.8417.
Furgal, C. and J. Seguin, 2006: Climate change, health, and vulnerability in Canadian northern Aboriginal communities. Environ. Health Perspect. , 114 (12), 1964–1970, doi:10.1289/ehp.8433.
Fussell, E., R. McLeman and F. Gemenne, 2018: Population displacements and migration patterns in response to Hurricane Katrina. In: Handbook of Environmental Displacement and Migration. London/ New York, Routledge, pp. 277–288.
Gakidou et al., 2018b: Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet , 392 (10159), 1923–1994, doi:10.1016/S0140-6736(18)32225-6.
Gamage, P.J., L.V. Fortington and C.F. Finch, 2020: Epidemiology of exertional heat illnesses in organised sports: a systematic review. J. Sci. Med. Sport , 23 (8), 701–709, doi:10.1016/j.jsams.2020.02.008.
Gandon, S., T. Day, C.J.E. Metcalf and B.T. Grenfell, 2016: Forecasting epidemiological and evolutionary dynamics of infectious diseases. Trends Ecol. Evol. , 31 (10), 776–788, doi:10.1016/j.tree.2016.07.010.
Gao, J., et al., 2018: Public health co-benefits of greenhouse gas emissions reduction: a systematic review. Sci. Total Environ. , 627, 388–402, doi:10.1016/j.scitotenv.2018.01.193.
Garcia, D.M. and M.C. Sheehan, 2016: Extreme weather-driven disasters and children’s health. Int. J. Health Serv. , 46 (1), 79–105, doi:10.1177/0020731415625254.
Gari, T., et al., 2017: Anaemia among children in a drought affected community in south-central Ethiopia. PLoS ONE, 12 (3), e170898, doi:10.1371/journal.pone.0170898.
Gariepy, G., H. Honkaniemi and A. Quesnel-Vallée, 2016: Social support and protection from depression: systematic review of current findings in Western countries. Br. J. Psychiatry, 209, doi:10.1192/bjp.bp.115.169094.
Garnier, J., et al., 2020: Helping to heal nature and ourselves through human-rights-based and gender-responsive One Health. One Health Outlook, 2 (1), 22, doi:10.1186/s42522-020-00029-0.
Garrido-Perez, J.M., C. Ordonez, R. Garcia-Herrera and J.L. Schnell, 2019: The differing impact of air stagnation on summer ozone across Europe. Atmosp. Environ. , 219, doi:10.1016/j.atmosenv.2019.117062.
Gascon, M., et al., 2019: Correlates of walking for travel in seven European cities: the PASTA project. Environ. Health Perspect. , 127 (9), doi:10.1289/ehp4603.
Gaskin, C., et al., 2017: Factors associated with the climate change vulnerability and the adaptive capacity of people with disability: a systematic review. Weather. Clim. Soc. , 9 (4), 801–814, doi:10.1175/wcas-d-16-0126.1.
Gasmi, S., et al., 2017: Surveillance for Lyme disease in Canada: 2009–2015. Can. Commun. Dis. Rep. , 43 (10), 194–199, doi:10.14745/ccdr.v43i10a01.
Gasparrini, A., Y. Guo and F. Sera, 2017: Projections of temperature-related excess mortality under climate change scenarios. Lancet Planet. Health, 1 (9), e360–e367.
Gasparrini, A., et al., 2015: Mortality risk attributable to high and low ambient temperature: a multicountry observational study. Lancet , 386 (9991), 369–375, doi:10.1016/s0140-6736(14)62114-0.
Gautier, D., D. Denis and B. Locatelli, 2016: Impacts of drought and responses of rural populations in West Africa: a systematic review. WIREs Clim. Change, 7 (5), 666–681.
Gebreslassie, M., 2020: COVID-19 and energy access: an opportunity or a challenge for the African continent?Energy Res. Soc. Sci. , 68, doi:10.1016/j.erss.2020.101677.
Geier, D.A., J.K. Kern and M.R. Geier, 2018: A longitudinal ecological study of seasonal influenza deaths in relation to climate conditions in the United States from 1999 through 2011. Infect. Ecol. Epidemiol. , 8, doi:10.1080/20008686.2018.1474708.
Gemenne, F. and J. Blocher, 2017: How can migration serve adaptation to climate change? Challenges to fleshing out a policy ideal. Geogr. J. , 183 (4), 336–347, doi:10.1111/geoj.12205.
Ghazani, M., et al., 2018: Temperature variability and gastrointestinal infections: a review of impacts and future perspectives. Int. J. Environ. Res. Public Health, 15 (4), 16, doi:10.3390/ijerph15040766. Electronic Resource.
Ghimire, R., S. Ferreira and J.H. Dorfman, 2015: Flood-induced displacement and civil conflict. World Dev. , 66, 614–628, doi:10.1016/j.worlddev.2014.09.021.
Ghimire, S. and S. Dhakal, 2015: Japanese encephalitis: challenges and intervention opportunities in Nepal. Vet. World, 8 (1), 61–65, doi:10.14202/vetworld.2015.61-65.
Gibb, R., et al., 2020: Zoonotic host diversity increases in human-dominated ecosystems. Nature, 584 (7821), 398, doi:10.1038/s41586-020-2562-8.
Gibon, T., et al., 2017: Health benefits, ecological threats of low-carbon electricity. Environ. Res. Lett. , 12 (3), 34023, doi:10.1088/1748-9326/aa6047.
Gibson, K., J. Barnett, N. Haslam and I. Kaplan, 2020: The mental health impacts of climate change: findings from a Pacific island atoll nation. J. Anxiety Disord. , 73, doi:10.1016/j.janxdis.2020.102237.
Gilmore, E.A. and H. Buhaug, 2021: Climate mitigation policies and the potential pathways to conflict: outlining a research agenda. Wiley Interdiscip. Rev. Clim. Change, 12 (5), e722.
Gilmore, E.A., L.H. Risi, E. Tennant and H. Buhaug, 2018: Bridging research and policy on climate change and conflict. Curr. Clim. Change Rep. , 4 (4), 313–319.
Giorgini, P., et al., 2017: Climate changes and human health: a review of the effect of environmental stressors on cardiovascular diseases across epidemiology and biological mechanisms. Curr. Pharm. Des. , 23 (22), 3247–3261, doi:10.2174/1381612823666170317143248.
Gleick, P.H., 2014: Water, drought, climate change, and conflict in Syria. Weather Clim. Soc. , 6 (3), 331–340, doi:10.1175/wcas-d-13-00059.1.
Global Nutrition Report 2020: Global Nutrition Report: Action on Equity to End Malnutrition. Development Initiatives, Bristol, UK.
Glover, D. and N. Poole, 2019: Principles of innovation to build nutrition-sensitive food systems in South Asia. Food Policy, 82, 63–73, doi:10.1016/j.foodpol.2018.10.010.
Gnonlonfin, G.J.B., et al., 2013: A review on aflatoxin contamination and its implications in the developing world: a sub-Saharan African perspective. Crit. Rev. Food Sci. Nutr. , 53 (4), 349–365, doi:10.1080/10408398.2010.535718.
GNR, 2018: Global Nutrition Report: Shining a Light to Spur Action on Nutrition. Development Initiatives, Bristol, UK.
Gobler, C.J., et al., 2017: Ocean warming since 1982 has expanded the niche of toxic algal blooms in the North Atlantic and North Pacific oceans. Proc. Natl. Acad. Sci. , 114 (19), 4975, doi:10.1073/pnas.1619575114.
Goggins, W.B. and E.Y.Y. Chan, 2017: A study of the short-term associations between hospital admissions and mortality from heart failure and meteorological variables in Hong Kong: weather and heart failure in Hong Kong. Int. J. Cardiol. , 228, 537–542, doi:10.1016/j.ijcard.2016.11.106.
Goodrich, C., A. Prakash and P. Udas, 2019: Gendered vulnerability and adaptation in Hindu-Kush Himalayas: research insights. Environ. Dev. , 31, 1–8, doi:10.1016/j.envdev.2019.01.001.
Gordon, K., A.L. Xavier and H.T. Neufeld, 2018: Healthy roots: building capacity through shared stories rooted in Haudenosaunee knowledge to promote indigenous foodways and well-being. Can. Food Stud. , 52 (2), 180–195.
Gosling, S.N., et al., 2017: Adaptation to climate change: a comparative analysis of modeling methods for heat-related mortality. Environ. Health Perspect. , 125 (8), doi:10.1289/ehp634.
Goyal, M., et al., 2021: The effect of the COVID-19 pandemic on maternal health due to delay in seeking health care: experience from a tertiary center. Int. J. Gynecol. Obstet. , 152 (2), 231–235, doi:10.1002/ijgo.13457.
Gray, C., D. Hopping and V. Mueller, 2020: The changing climate-migration relationship in China, 1989–2011. Clim. Change, doi:10.1007/s10584-020-02657-x.
Gray, C. and E. Wise, 2016: Country-specific effects of climate variability on human migration. Clim. Change, 135 (3-4), 555–568, doi:10.1007/s10584-015-1592-y.
Green, D. and L. Minchin, 2014: Living on climate-changed country: indigenous health, well-being and climate change in remote Australian communities. EcoHealth, 11 (2), 263–272, doi:10.1007/s10393-013-0892-9.
Green, D., et al., 2017: Advancing Australia’s role in climate change and health research. Nat. Clim. Change, 7 (2), 103–106, doi:10.1038/nclimate3182.
Green, H., et al., 2019: Impact of heat on mortality and morbidity in low and middle income countries: a review of the epidemiological evidence and considerations for future research. Environ. Res. , 171, 80–91, doi:10.1016/j.envres.2019.01.010.
Green, R., et al., 2015: The potential to reduce greenhouse gas emissions in the UK through healthy and realistic dietary change. Climatic Change, 129 (1), 253–265, doi:10.1007/s10584-015-1329-y.
Greenwood, M. and N. Lindsay, 2019: A commentary on land, health, and Indigenous knowledge(s). Glob. Health Promot. , 26 (3), 82–86, doi:10.1177/1757975919831262.
Grey, S. and R. Patel, 2015: Food sovereignty as decolonization: some contributions from Indigenous movements to food system and development politics. Agric. Hum. Values, 32 (3), 431–444, doi:10.1007/s10460-014-9548-9.
Grundstein, A., et al., 2017: American football and fatal exertional heat stroke: a case study of Korey Stringer. Int. J. Biometeorol. , 61 (8), 1471–1480, doi:10.1007/s00484-017-1324-2.
Guetter, C.R., et al., 2018: Greening the operating room. Am. J. Surg. , 216 (4), 683–688, doi:10.1016/j.amjsurg.2018.07.021.
Guirguis, K., et al., 2018: Heat, disparities, and health outcomes in San Diego county’s diverse climate zones. GeoHealth, 2 (7), 212–223, doi:10.1029/2017gh000127.
Guo, Y., et al., 2020: The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak – an update on the status. Mil. Med. Res. , 7 (1), doi:10.1186/s40779-020-00240-0.
Guo, Y., et al., 2016: Temperature variability and mortality: a multi-country study. Environ. Health Perspect. , 124 (10), 1554–1559, doi:10.1289/ehp149.
Guo, Y., et al., 2018: Quantifying excess deaths related to heatwaves under climate change scenarios: a multicountry time series modelling study. PLoS Med. , 15 (7), e1002629, doi:10.1371/journal.pmed.1002629.
Guo, Y.M., 2017: Hourly associations between heat and ambulance calls. Environ. Pollut. , 220, 1424–1428, doi:10.1016/j.envpol.2016.10.091.
Guyot, M., et al., 2006: Local observations of climate change and impacts on traditional food security in two northern Aboriginal communities. Int. J. Circumpolar Health, 65 (5), 403–415, doi:10.3402/ijch.v65i5.18135.
Guzman Herrador, B., et al., 2016: Association between heavy precipitation events and waterborne outbreaks in four Nordic countries, 1992–2012. J. Water Health, 14 (6), 1019–1027, doi:10.2166/wh.2016.071.
Guzman Herrador, B.R., et al., 2015: Analytical studies assessing the association between extreme precipitation or temperature and drinking water-related waterborne infections: a review. Environ. Health, 14, 29, doi:10.1186/s12940-015-0014-y.
Haas, S., A. Gianoli and M. Van Eerd, 2021: The roles of community resilience and risk appraisal in climate change adaptation: the experience of the Kannagi Nagar resettlement in Chennai. Environ. Urban. , doi:10.1177/0956247821993391.
Haasnoot, M., J. Lawrence and A.K. Magnan, 2021: Pathways to coastal retreat. Science, 372 (6548), 1287–1290. http://science.sciencemag.org/content/372/6548/1287.abstract.
Habibi, P., et al., 2021: The impacts of climate change on occupational heat strain in outdoor workers: a systematic review. Urban Clim. , 36, doi:10.1016/j.uclim.2021.100770.
Haddout, S., K.L. Priya, A.M. Hoguane and I. Ljubenkov, 2020: Water scarcity: a big challenge to slums in Africa to fight against COVID-19. Sci. Technol. Libr. , 39 (3), 1–8.
Haghighi, M.M., et al., 2021: Impacts of high environmental temperatures on congenital anomalies: a systematic review. Int. J. Environ. Res. Public Health, 18 (9), doi:10.3390/ijerph18094910.
Haines, A. and K. Ebi, 2019: The imperative for climate action to protect health. N. Engl. J. Med. , 380 (3), 263–273, doi:10.1056/NEJMra1807873.
Hajat, S., 2017: Health effects of milder winters: a review of evidence from the United Kingdom. Environ. Health, 16, 109, doi:10.1186/s12940-017-0323-4.
Hajat, S., et al., 2017: The effect of ambient temperature on type-2-diabetes: case-crossover analysis of 4+ million GP consultations across England. Environ. Health, 16 (1), 73, doi:10.1186/s12940-017-0284-7.
Hall, N., et al., 2021: Climate change and infectious diseases in Australia’s Torres Strait Islands. Aust. N. Z. J. Public Health, 45 (2), 122–128, doi:10.1111/1753-6405.13073.
Hall, N. and L. Crosby, 2020: Climate change impacts on health in remote indigenous communities in Australia. Int. J. Environ. Health Res, 16, doi:10.1080/09603123.2020.1777948.
Hallema, D., F. Robinne and S. McNulty, 2020: Pandemic spotlight on urban water quality. Ecol. Process. , 9 (1), doi:10.1186/s13717-020-00231-y.
Hamaoui-Laguel, L., et al., 2015: Effects of climate change and seed dispersal on airborne ragweed pollen loads in Europe. Nat. Clim. Change, 5, 766, doi:10.1038/nclimate2652.
Hamilton, I., et al., 2021: The public health implications of the Paris Agreement: a modelling study. Lancet Planet. Health, 5 (2), E74–E83.
Hamilton, L.C., K. Saito and P.A. Loring, 2016: Climigration? Population and climate change in Arctic Alaska, Population and environment , 38 (2), 115–133.
Hanigan, I., C. Butler, P. Kokic and M. Hutchinson, 2012: Suicide and drought in New South Wales, Australia, 1970–2007. Proc. Natl. Acad. Sci. U.S.A. , 109 (35), 13950–13955, doi:10.1073/pnas.1112965109.
Hanigan, I.C., K.B.G. Dear and A. Woodward, 2021: Increased ratio of summer to winter deaths due to climate warming in Australia, 1968–2018. Aust. N. Z. J. Public Health, doi:10.1111/1753-6405.13107.
Hansel, N.N., M.C. McCormack and V. Kim, 2016: The effects of air pollution and temperature on COPD. COPD, 13 (3), 372–379, doi:10.3109/15412555.2015.1089846.
Hansen, A., et al., 2008: The effect of heat waves on mental health in a temperate Australian city. Environ. Health Perspect. , 116 (10), 1369–1375, doi:10.1289/ehp.11339.
Hansen, A., et al., 2015: Transmission of haemorrhagic fever with renal syndrome in china and the role of climate factors: a review. Int. J. Infect. Dis. , 33, 212–218, doi:10.1016/j.ijid.2015.02.010.
Haq, G. and G. Gutman, 2014: Climate gerontology meeting the challenge of population ageing and climate change. Z. Gerontol. Geriat. , 47 (6), 462, doi:10.1007/s00391-014-0677-y.
Haque, M., et al., 2015: Behavioral change due to climate change effects accelerate tiger human conflicts: a study on Sundarbans mangrove forests, Bangladesh. Int. J. Conserv. Sci. , 6 (4), 669–684.
Haque, M.R., N. Parr and S. Muhidin, 2019: Parents’ healthcare-seeking behavior for their children among the climate-related displaced population of rural Bangladesh. Soc. Sci. Med. , 226, 9–20, doi:10.1016/j.socscimed.2019.02.032.
Harder, R., M. Giampietro and S. Smukler, 2021: Towards a circular nutrient economy. A novel way to analyze the circularity of nutrient flows in food systems. Resour. Conserv. Recycl. , 172, doi:10.1016/j.resconrec.2021.105693.
Harper, S., et al., 2015: Climate-sensitive health priorities in Nunatsiavut, Canada. BMC Public Health, 15, doi:10.1186/s12889-015-1874-3.
Harrington, L. and F. Otto, 2018: Changing population dynamics and uneven temperature emergence combine to exacerbate regional exposure to heat extremes under 1.5°C and 2°C of warming. Environ. Res. Lett. , 13, doi:10.1088/1748-9326/aaaa99.
Harrington, L.J., D.J. Frame, E. Hawkins and M. Joshi, 2017: Seasonal cycles enhance disparities between low- and high-income countries in exposure to monthly temperature emergence with future warming. Environ. Res. Lett. , 12 (11), doi:10.1088/1748-9326/aa95ae.
Hasegawa, T., et al., 2018: Risk of increased food insecurity under stringent global climate change mitigation policy. Nat. Clim. Change, 8 (8), 699–703, doi:10.1038/s41558-018-0230-x.
Hasegawa, T., S. Fujimori, K. Takahashi and T. Masui, 2015: Scenarios for the risk of hunger in the twenty-first century using Shared Socioeconomic Pathways. Environ. Res. Lett. , 10 (1), doi:10.1088/1748-9326/10/1/014010.
Hashim, J.H. and Z. Hashim, 2016: Climate change, extreme weather events, and human health implications in the Asia Pacific region. Asia Pac. J. Public Health, 28 (2 Suppl), 8S–14S, doi:10.1177/1010539515599030.
Hassan, E.M., et al., 2021: A review of Cryptosporidium spp. and their detection in water. Water Sci. Technol. , 83 (1), 1–25, doi:10.2166/wst.2020.515.
Hatfield, S., et al., 2018: Indian time: time, seasonality, and culture in traditional ecological knowledge of climate change. Ecol. Process. , 7, doi:10.1186/s13717-018-0136-6.
Hatvani-Kovacs, G., J. Bush, E. Sharifi and J. Boland, 2018: Policy recommendations to increase urban heat stress resilience. Urban Clim. , 25, 51–63.
Hauer, M. E., 2017: Migration induced by sea-level rise could reshape the US population landscape. Nat. Clim. Change, 7 (5), 321, doi:10.1038/nclimate3271.
Hauer, M. E., J.M. Evans and D.R. Mishra, 2016: Millions projected to be at risk from sea-level rise in the continental United States. Nat. Clim. Change, 6, 691–695.
Hauer, M. E., R.D. Hardy, D.R. Mishra and J.S. Pippin, 2019: No landward movement: examining 80 years of population migration and shoreline change in Louisiana. Popul. Environ, 40(4), 369-387.
Haussig, J.M., et al., 2018: Early start of the West Nile fever transmission season 2018 in Europe. Euro Surveill. , 23 (32), 7–12, doi:10.2807/1560-7917.es.2018.23.32.1800428.
Hayashida, K., K. Shimizu and H. Yokota, 2019: Severe heatwave in Japan. Acute Med. Surg. , 6 (2), 206–207, doi:10.1002/ams2.387.
Hayek, M., H. Harwatt, W. Ripple and N. Mueller, 2021: The carbon opportunity cost of animal-sourced food production on land. Nat. Sustain. , 4 (1), 21–24, doi:10.1038/s41893-020-00603-4.
Hayes, K., P. Berry and K. Ebi, 2019: Factors influencing the mental health consequences of climate change in Canada. Int. J. Environ. Res. Public Health, 16, 1583, doi:10.3390/ijerph16091583.
Hayes, K., et al., 2018: Climate change and mental health: risks, impacts and priority actions. Int. J. Ment. Health Syst. , 12, 1–12, doi:10.1186/s13033-018-0210-6.
Hayes, K. and B. Poland, 2018: Addressing mental health in a changing climate: incorporating mental health indicators into climate change and health vulnerability and adaptation assessments. Int. J. Environ. Res. Public Health, 15 (9), doi:10.3390/ijerph15091806.
Hayward, G. and S. Ayeb-Karlsson, 2021: ‘Seeing with Empty Eyes’: a systems approach to understand climate change and mental health in Bangladesh. Clim. Change, 165 (1), 1–30.
Heaney, A. and S. Winter, 2016: Climate-driven migration: an exploratory case study of Maasai health perceptions and help-seeking behaviors. Int. J. Public Health, 61 (6), 641–649, doi:10.1007/s00038-015-0759-7.
Heaviside, C., S. Vardoulakis and X.M. Cai, 2016: Attribution of mortality to the urban heat island during heatwaves in the West Midlands, UK. Environ. Health, 15, doi:10.1186/s12940-016-0100-9.
Hedenus, F., S. Wirsenius and D.J. Johansson, 2014: The importance of reduced meat and dairy consumption for meeting stringent climate change targets. Climatic change, 124 (1), 79–91, doi:10.1007/s10584-014-1104-5.
Hegre, H., et al., 2016: Forecasting civil conflict along the shared socioeconomic pathways. Environ. Res. Lett. , 11 (5), 54002.
Hegre, H., H.M. Nygård and P. Landsverk, 2021: Can we predict armed conflict? How the first 9 years of published forecasts stand up to reality. Int. Stud. Q. 65 (3), 660-668.
Hegre, H. and N. Sambanis, 2006: Sensitivity analysis of empirical results on civil war onset. J. Confl. Resolut. , 50 (4), 508–535.
Heilmann, K., M. Kahn and C. Tang, 2021: The urban crime and heat gradient in high and low poverty areas. J .Public Econ. , 197, doi:10.1016/j.jpubeco.2021.104408.
Heininen, L. and H. Exner-Pirot, 2020: Climate Change and Arctic Security. Springer International Publishing.
Hellberg, R.S. and E. Chu, 2016: Effects of climate change on the persistence and dispersal of foodborne bacterial pathogens in the outdoor environment: a review. Crit. Rev. Microbiol. , 42 (4), 548–572, doi:10.3109/1040841x.2014.972335.
Hellden, D., et al., 2021: Climate change and child health: a scoping review and an expanded conceptual framework. Lancet Planet. Health, 5 (3), E164–E175.
Helm, S., et al., 2018: Differentiating environmental concern in the context of psychological adaption to climate change. Glob. Environ. Change Policy Dimens. , 48, 158–167, doi:10.1016/j.gloenvcha.2017.11.012.
Hendrix, C. and S. Haggard, 2015: Global food prices, regime type, and urban unrest in the developing world. J. Peace Res. , 52 (2), 143–157, doi:10.1177/0022343314561599.
Henrique, K. and P. Tschakert, 2020: Pathways to urban transformation: from dispossession to climate justice. Prog. Hum. Geogr. , doi:10.1177/0309132520962856.
Heo, S., M.L. Bell and J.T. Lee, 2019a: Comparison of health risks by heat wave definition: applicability of wet-bulb globe temperature for heat wave criteria. Environ. Res. , 168, 158–170, doi:10.1016/j.envres.2018.09.032.
Heo, S., et al., 2019b: The use of a quasi-experimental study on the mortality effect of a heat wave warning system in Korea. Int. J. Environ. Res. Public Health, 16 (12), doi:10.3390/ijerph16122245.
Hepburn, C., et al., 2020: Will COVID-19 fiscal recovery packages accelerate or retard progress on climate change?Oxf. Rev. Econ. Policy, 36, 359–S381, doi:10.1093/oxrep/graa015.
Hermans, K. and L. Garbe, 2019: Droughts, livelihoods, and human migration in northern Ethiopia. Reg. Environ. Change, doi:10.1007/s10113-019-01473-z.
Heslin, A., 2019: Climate migration and cultural preservation: the case of the Marshallese diaspora. In: Loss and Damage from Climate Change: Concepts, Methods and Policy Options. Springer, Cham. ISBN 978-3319720265.
Heslin, A., 2021: Riots and resources: how food access affects collective violence. J. Peace Res. , 58 (2), 199–214.
Hess, J., J. McDowell and G. Luber, 2012: Integrating climate change adaptation into public health practice: using adaptive management to increase adaptive capacity and build resilience. Environ. Health Perspect. , 120 (2), 171–179, doi:10.1289/ehp.1103515.
Hillier, S.A., A. Taleb, E. Chaccour and C. Aenishaenslin, 2021: Examining the concept of One Health for indigenous communities: a systematic review. One Health, 12, 100248, doi:10.1016/j.onehlt.2021.100248.
Hino, M., C.B. Field and K.J. Mach, 2017: Managed retreat as a response to natural hazard risk. Nat. Clim. Change, 7, 364–370.
HLPE, 2020: Food Security and Nutrition: Building a Global narrative Towards 2030. FAO, Rome.
Hobbie, S.E. and N.B. Grimm, 2020: Nature-based approaches to managing climate change impacts in cities. Philos. Trans. Royal Soc. B Biol. Sci. , 375 (1794), doi:10.1098/rstb.2019.0124.
Hochman, A., et al., 2021: The relationship between cyclonic weather regimes and seasonal influenza over the Eastern Mediterranean. Sci. Total Environ. , 750, doi:10.1016/j.scitotenv.2020.141686.
Hock, S., et al., 2018: Childhood malnutrition and maltreatment are linked with personality disorder symptoms in adulthood: Results from a Barbados lifespan cohort. Psychiatry Res. , 269, 301–308.
Høeg, E. and C. Tulloch, 2018: Sinking strangers: media representations of climate refugees on the BBC and Al Jazeera. J. Commun. Inq. , 43, 19685991880948, doi:10.1177/0196859918809486.
Hoffman, J., V. Shandas and N. Pendleton, 2020: The effects of historical housing policies on resident exposure to intra-urban heat: a study of 108 US urban areas. Climate, 8 (1), doi:10.3390/cli8010012.
Hoffmann, R., et al., 2020: A meta-analysis of country-level studies on environmental change and migration. Nat. Clim. Change, 10 (10), 904–912, doi:10.1038/s41558-020-0898-6.
Hollowed, A., et al., 2013: Projected impacts of climate change on marine fish and fisheries. Ices J. Mar. Sci. , 70 (5), 1023–1037, doi:10.1093/icesjms/fst081.
Holman, C., R.M. Harrison and X. Querol, 2015: Review of the efficacy of low emission zones to improve urban air quality in European cities. Atmos. Environ. , 111, 161–169, doi:10.1016/j.atmosenv.2015.04.009.
Holsman, K., et al., 2020: Ecosystem-based fisheries management forestalls climate-driven collapse. Nat. Commun. , 11 (1), doi:10.1038/s41467-020-18300-3.
Honda, Y. and D. Onozuka, 2020: Heat-Related Mortality/Morbidity in East Asia. In: Extreme Weather Events and Human Health: International Case Studies, pp. 131–144. Springer, Dordrecht. doi:10.1007/978-3-030-23773-8_10.
Hondula, D.M., M. Georgescu and R.C. Balling, 2014: Challenges associated with projecting urbanization-induced heat-related mortality. Sci. Total Environ. , 490, 538–544, doi:10.1016/j.scitotenv.2014.04.130.
Hong, C.P., et al., 2019: Impacts of climate change on future air quality and human health in China. Proc. Natl. Acad. Sci. U.S.A. , 116 (35), 17193–17200, doi:10.1073/pnas.1812881116.
Hooijer, A. and R. Vernimmen, 2021: Global LiDAR land elevation data reveal greatest sea-level rise vulnerability in the tropics. Nat. Commun. , 12 (1), 3592, doi:10.1038/s41467-021-23810-9.
Hopp, S., F. Dominici and J.F. Bobb, 2018: Medical diagnoses of heat wave-related hospital admissions in older adults. Prev. Med. , 110, 81–85, doi:10.1016/j.ypmed.2018.02.001.
Horn, L.M., et al., 2018: Association between precipitation and diarrheal disease in Mozambique. Int. J. Environ. Res. Public Health, 15 (4), doi:10.3390/ijerph15040709.
Hornsey, M., E. Harris, P. Bain and K. Fielding, 2016: Meta-analyses of the determinants and outcomes of belief in climate change. Nat. Clim. Change, 6 (6), 622, doi:10.1038/nclimate2943.
Horton, R.M., A.W. de Sherbinin, D.Wrathall and M. Oppenheimer, 2021: Assessing human habitability and migration. Science372 (6548), 1279–1283. Available at: http://science.sciencemag.org/content/372/6548/1279.abstract.
Hossain, K., 2016: Securitizing the Arctic indigenous peoples: a community security perspective with special reference to the Sámi of the European high north. Polar Sci. , 10 (3), 415–424.
Houde, M., et al., 2020: Mercury in ringed seals (Pusa hispida) from the Canadian Arctic in relation to time and climate parameters. Environ. Toxicol. Chem. , 39 (12), 2462–2474, doi:10.1002/etc.4865.
Houéménou, H., et al., 2021: Pathogenic Leptospira and water quality in African cities: a case study of Cotonou, Benin. Sci. Total Environ. , 774, 145541, doi:10.1016/j.scitotenv.2021.145541.
Howard, C., et al., 2021: SOS! Summer of Smoke: a retrospective cohort study examining the cardiorespiratory impacts of a severe and prolonged wildfire season in Canada’s high subarctic. BMJ Open, 11 (2), doi:10.1136/bmjopen-2020-037029.
Howard, G., R. Calow, A. Macdonald and J. Bartram, 2016: Climate change and water and sanitation: likely impacts and emerging trends for action. Annu. Rev. Environ. Resour. , 41, 253–276, doi:10.1146/annurev-environ-110615-085856.
Hoy, D., et al., 2014: Adapting to the health impacts of climate change in a sustainable manner. Glob. Health, 10, doi:10.1186/s12992-014-0082-8.
Hrabok, M., A. Delorme and V.I. Agyapong, 2020: Threats to mental health and well-being associated with climate change. J. Anxiety Disord. , 76, 102295.
Hsiang, S., M. Burke and E. Miguel, 2013: Quantifying the influence of climate on human conflict. Science, 341 (6151), 1212, doi:10.1126/science.1235367.
Hsiang, S., et al., 2017: Estimating economic damage from climate change in the United States. Science, 356 (6345), 1362–1369, doi:10.1126/science.aal4369.
Hsiang, S.M. and B. Marshall, 2014: Climate, conflict, and social stability: what does the evidence say?Clim. Change, 123 (1), 39–55, doi:10.1007/s10584-013-0868-3.
Hu, L.Q., O.V. Wilhelmi and C. Uejio, 2019: Assessment of heat exposure in cities: combining the dynamics of temperature and population. Sci. Total Environ. , 655, 1–12, doi:10.1016/j.scitotenv.2018.11.028.
Huang, C., et al., 2018: Mortality burden attributable to heatwaves in Thailand: a systematic assessment incorporating evidence-based lag structure. Environ. Int. , 121, 41–50, doi:10.1016/j.envint.2018.08.058.
Huang, J., et al., 2018: Projections for temperature-related years of life lost from cardiovascular diseases in the elderly in a Chinese city with typical subtropical climate. Environ. Res. , 167, 614–621.
Huber, R., et al., 2020a: Symposium report: emerging threats for human health – impact of socioeconomic and climate change on zooanthroponosis in the Republic of Sakha (Yakutia), Russia. Int. J. Circumpolar Health, 79 (1), doi:10.1080/22423982.2020.1715698.
Huber, V., et al., 2020b: Temperature-related excess mortality in German cities at 2 degrees C and higher degrees of global warming. Environ. Res. , 186, doi:10.1016/j.envres.2020.109447.
Huda, M.S., 2021: An ecological response to ethno-nationalistic populism: grassroots environmental peacebuilding in south Asia. Int. Aff. , 97 (1), 119–138.
Huda, M.S. and S.H. Ali, 2018: Environmental peacebuilding in South Asia: establishing consensus on hydroelectric projects in the Ganges-Brahmaputra-Meghna (GBM) Basin. Geoforum, 96, 160–171.
Hueffer, K., M. Ehrlander, K. Etz and A. Reynolds, 2019: One health in the circumpolar North. Int. J. Circumpolar Health, 78 (1), doi:10.1080/22423982.2019.1607502.
Hundessa, S., et al., 2018: Projecting potential spatial and temporal changes in the distribution of Plasmodium vivax and Plasmodium falciparum malaria in China with climate change. Sci. Total Environ. , 627, 1285–1293, doi:10.1016/j.scitotenv.2018.01.300.
Hunter, L.M. and D.H. Simon, 2017: Might climate change the “healthy migrant” effect?Glob. Environ. Change, 47, 133–142.
Hunter, L.M., et al., 2021: Scales and sensitivities in climate vulnerability, displacement, and health. Popul. Environ. , 43 (1), 61–81, doi:10.1007/s11111-021-00377-7.
Hussain-Alkhateeb, L., et al., 2018: Early warning and response system (EWARS) for dengue outbreaks: recent advancements towards widespread applications in critical settings. PLoS ONE, 13 (5), doi:10.1371/journal.pone.0196811.
Hynes, W., T. Benjamin, L. Patrick and L. Igor, 2020: Bouncing forward: a resilience approach to dealing with COVID-19 and future systemic shocks. Environ. Syst. Decis. , 40, 174–184.
Ide, T., 2019: The impact of environmental cooperation on peacemaking: definitions, mechanisms, and empirical evidence. Int. Stud. Rev. , 21 (3), 327–346.
Ide, T., 2020: The dark side of environmental peacebuilding. World Dev. , 127, 104777.
Ide, T., et al., 2021: The past and future (s) of environmental peacebuilding. Int. Aff. , 97 (1), 1–16.
Ide, T., M. Brzoska, J. Donges and C. Schleussner, 2020: Multi-method evidence for when and how climate-related disasters contribute to armed conflict risk. Glob. Environ. Change Policy Dimens. , 62, doi:10.1016/j.gloenvcha.2020.102063.
Ide, T. and C. Frohlich, 2015: Socio-environmental cooperation and conflict? A discursive understanding and its application to the case of Israel and Palestine. Earth Syst. Dyn. , 6 (2), 659–671, doi:10.5194/esd-6-659-2015.
Ide, T. and A. Tubi, 2020: Education and environmental peacebuilding: insights from three projects in Israel and Palestine. Ann. Am. Assoc. Geogr. , 110 (1), 1–17.
Ikaheimo, T.M., 2018: Cardiovascular diseases, cold exposure and exercise. Temperature, 5 (2), 123–146, doi:10.1080/23328940.2017.1414014.
Im, E., J. Pal and E. Eltahir, 2017: Deadly heat waves projected in the densely populated agricultural regions of South Asia. Sci. Adv. , 3 (8), doi:10.1126/sciadv.1603322.
IMF, 2020: World Economic Outlook: a Long and Difficult Ascent . International Monetary Fund, Washington, DC.
Internal Displacement Monitoring Centre, 2020: Global Report on Internal Displacement . IDMC, Geneva. 136p.
International Organization for Migration, 2019: World Migration Report 2020. Geneva, https://www.un.org/sites/un2.un.org/files/wmr_2020.pdf. Last accessed 3 September 2021.
IPCC, 2019a: IPCC Special Report on the Ocean and Cryosphere in a Changing Climate[H.-O. Pörtner, D.C. Roberts, V. Masson-Delmotte, P. Zhai, M. Tignor, E. Poloczanska, K. Mintenbeck, A. Alegría, M. Nicolai, A. Okem, J. Petzold, B. Rama, N.M. Weyer (eds.)]. https://report.ipcc.ch/srocc/pdf/SROCC_FinalDraft_FullReport.pdf. (1170 pp).
IPCC, 2019b: Climate Change and Land: an IPCC special report on climate change, desertification, land degradation, sustainable land management, food security, and greenhouse gas fluxes in terrestrial ecosystems[P.R. Shukla, J. Skea, E. Calvo Buendia, V. Masson-Delmotte, H.-O. Pörtner, D. C. Roberts, P. Zhai, R. Slade, S. Connors, R. van Diemen, M. Ferrat, E. Haughey, S. Luz, S. Neogi, M. Pathak, J. Petzold, J. Portugal Pereira, P. Vyas, E. Huntley, K. Kissick, M. Belkacemi, J. Malley, (eds.)].
IPES-Food, 2018: Breaking Away from Industrial Food and Farming Systems: Seven Case Studies of Agroecological Transition. IPES Secretariat, Brussels.
IPES-Food, 2020: The Added Value(s) of Agroecology: Unlocking the Potential for Transition in West Africa. IPES Secretariat, Brussels.
Ishida, H., et al., 2014: Global-scale projection and its sensitivity analysis of the health burden attributable to childhood undernutrition under the latest scenario framework for climate change research. Environ. Res. Lett. , 9 (6), doi:10.1088/1748-9326/9/6/064014.
Islam, M., M. Alharthi and M. Alam, 2019: The impacts of climate change on road traffic accidents in Saudi Arabia. Climate, 7 (9), 103.
Islam, M.R. and M. Hasan, 2016: Climate-induced human displacement: a case study of Cyclone Aila in the south-west coastal region of Bangladesh. Nat. Hazards, 81 (2), 1051–1071.
Islam, M.R. and M. Shamsuddoha, 2017: Socioeconomic consequences of climate induced human displacement and migration in Bangladesh. Int. Sociol. , 32 (3), 277-298.
Islam, M.Z., O. Kolade and G. Kibreab, 2018: Post-disaster housing reconstruction: the impact of resourcing in post-cyclones Sidr and Aila in Bangladesh. J. Int. Dev. , 30 (6), 934–960.
Islam, S., C. Chu, J. Smart and L. Liew, 2020: Integrating disaster risk reduction and climate change adaptation: a systematic literature review. Clim. Dev. , 12 (3), 255–267, doi:10.1080/17565529.2019.1613217.
Ito, Y., M. Akahane and T. Imamura, 2018: Impact of temperature in summer on emergency transportation for heat-related diseases in Japan. Chin. Med. J. , 131, 574–582, doi:10.4103/0366-6999.226061.
Jaakkola, J.J.K., S. Juntunen and K. Nakkalajarvi, 2018: The holistic effects of climate change on the culture, well-being, and health of the Saami, the only indigenous people in the European Union. Curr. Environ. Health Rep. , 5 (4), 401–417, doi:10.1007/s40572-018-0211-2.
Jacob, B. and M. Kazaura, 2021: Access to safe water, sanitation, and hygiene: a cross-sectional study among the Maasai in Tanzania. Am. J. Trop. Med. Hyg. , doi:10.4269/ajtmh.20-0134.
Jahn, S. and E. Hertig, 2021: Modeling and projecting health-relevant combined ozone and temperature events in present and future Central European climate. Air Qual. Atmos. Health, 14 (4), 563–580, doi:10.1007/s11869-020-00961-0.
Jalilov, S.M., S.A. Amer and F.A. Ward, 2018: Managing the water-energy-food nexus: opportunities in Central Asia. J. Hydrol. , 557, 407–425.
Jamero, M., et al., 2017: Small-island communities in the Philippines prefer local measures to relocation in response to sea-level rise. Nat. Clim. Change, 7 (8), 581–586, doi:10.1038/nclimate3344.
James, L.E., C. Welton-Mitchell, J.R. Noel and A.S. James, 2020: Integrating mental health and disaster preparedness in intervention: a randomized controlled trial with earthquake and flood-affected communities in Haiti. Psychol. Med. , 50 (2), 342–352, doi:10.1017/s0033291719000163.
James, S.L., et al., 2018: Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet , 392 (10159), 1789–1858.
Jang, J., et al., 2020: Roles of urban heat anomaly and land-use/land-cover on the heat-related mortality in the national capital region of South Korea: a multi-districts time-series study. Environ. Int. , 145, doi:10.1016/j.envint.2020.106127.
Jardine, S., M. Fisher, S. Moore and J. Samhouri, 2020: Inequality in the economic impacts from climate shocks in fisheries: the case of harmful algal blooms. Ecol. Econ. , 176, doi:10.1016/j.ecolecon.2020.106691.
Jay, O., et al., 2021: Reducing the health effects of hot weather and heat extremes: from personal cooling strategies to green cities. Lancet , 398 (10301), 16, doi:10.1016/S0140-6736(21)01209-5.
Jehn, M., et al., 2013: Tele-monitoring reduces exacerbation of COPD in the context of climate change – a randomized controlled trial. Environ. Health, 12, 99, doi:10.1186/1476-069x-12-99.
Jennings, V. and O. Bamkole, 2019: The relationship between social cohesion and urban green space: an avenue for health promotion. Int. J. Environ. Res. Public Health, 16 (3), doi:10.3390/ijerph16030452.
Jennings, V., C.E. Reid and C.H. Fuller, 2021: Green infrastructure can limit but not solve air pollution injustice. Nat. Commun. , 12 (1), doi:10.1038/s41467-021-24892-1.
Jessoe, K., D. T. Manning, and J. E. Taylor, 2018: Climate change and labour allocation in rural Mexico: evidence from annual fluctuations in weather. Econ J, 128 (608), 230–261.
Jim, C.Y., C.K. van den Bosch and W.Y. Chen, 2018: Acute challenges and solutions for urban forestry in compact and densifying cities. J. Urban Plan. Dev. , 144 (3), doi:10.1061/(asce)up.1943-5444.0000466.
Johansson, J.M., et al., 2020: The European heat wave of 2018 and its promotion of the ozone climate penalty in southwest Sweden. Boreal Environ. Res. , 25, 39–50.
Johnson-Jennings, M., et al., 2020: Ode’imin Giizis: proposing and piloting gardening as an indigenous childhood health intervention. J. Health Care Poor Underserved, 31 (2), 871–888, doi:10.1353/hpu.2020.0066.
Johnson, C., et al., 2013: Social protection and climate change: emerging issues for research, policy and practice. Dev. Policy Rev. , 31 (s2), o2–o18, doi:10.1111/dpr.12036.
Johnson, M.F., 2021: Local engagement in environmental peacebuilding: protected area development as a pathway to peace in Afghanistan. Dev. Pract. , 1–13. DOI: 10.1080/09614524.2021.1937538
Johnston, F.H., A.M. Kavanagh, D.M. Bowman and R.K. Scott, 2002: Exposure to bushfire smoke and asthma: an ecological study. Med. J. Aust. , 176, 535–538.
Jones, A., 2017: Food insecurity and mental health status: a global analysis of 149 countries. Am. J. Prev. Med. , 53 (2), 264–273, doi:10.1016/j.amepre.2017.04.008.
Jones, B., et al., 2018: Avoiding population exposure to heat-related extremes: demographic change vs climate change. Clim. Change, 146 (3-4), 423–437, doi:10.1007/s10584-017-2133-7.
Jones, L., 2019: Resilience isn’t the same for all: comparing subjective and objective approaches to resilience measurement. Wiley Interdiscip. Rev. Clim. Change, 10 (1), doi:10.1002/wcc.552.
Jones, R., H. Bennett, G. Keating and A. Blaiklock, 2014: Climate change and the right to health for Maori in Aotearoa/New Zealand. Health Hum. Rights, 16 (1), 54–68.
Jones, R., A. Macmillan and P. Reid, 2020: Climate change mitigation policies and co-impacts on indigenous health: a scoping review. Int. J. Environ. Res. Public Health, 17 (23), doi:10.3390/ijerph17239063.
Jost, C., et al., 2016: Understanding gender dimensions of agriculture and climate change in smallholder farming communities. Clim. Dev. , 8 (2), 133–144, doi:10.1080/17565529.2015.1050978.
Jugert, P., et al., 2016: Collective efficacy increases pro-environmental intentions through increasing self-efficacy. J. Environ. Psychol. , 48, 12–23, doi:10.1016/j.jenvp.2016.08.003.
Jutla, A., R. Khan and R. Colwell, 2017: Natural disasters and cholera outbreaks: current understanding and future outlook. Curr. Environ. Health Rep. , 4 (1), 99–107, doi:10.1007/s40572-017-0132-5.
Kabir, S.M.S., 2018: Psychological health challenges of the hill-tracts region for climate change in Bangladesh. Asian J. Psychiatr. , 34, 74–77, doi:10.1016/j.ajp.2018.04.001.
Kaczan, D.J. and J. Orgill-Meyer, 2020: The impact of climate change on migration: a synthesis of recent empirical insights. Clim. Change, 158 (3), 281–300, doi:10.1007/s10584-019-02560-0.
Kadandale, S., et al., 2020: Primary health care and the climate crisis. Bull. World Health Organ. , 98 (11), 818–820, doi:10.2471/blt.20.252882.
Kaffenberger, B.H., D. Shetlar, S.A. Norton and M. Rosenbach, 2017: The effect of climate change on skin disease in North America. J. Am. Acad. Dermatol. , 76 (1), 140–147, doi:10.1016/j.jaad.2016.08.014.
Kakinuma, K., et al., 2020: Flood-induced population displacements in the world. Environ. Res. Lett. , 15 (12), 124029, doi:10.1088/1748-9326/abc586.
Kalilou, O., 2021: Climate change and conflict in the Sahel: the acacia gum tree as a tool for environmental peacebuilding. Int. Aff. , 97 (1), 201–218.
Kälin, W., 2018: The global compact on migration: a ray of hope for disaster-displaced persons. Int. J. Refug. Law, 30 (4), 664–667, doi:10.1093/ijrl/eey047.
Kalinda, C., M. Chimbari and S. Mukaratirwa, 2017: Effect of temperature on the Bulinus globosus – Schistosoma haematobium system. Infect. Dis. Poverty, 6, doi:10.1186/s40249-017-0260-z.
Kalisa, E., et al., 2018: Temperature and air pollution relationship during heatwaves in Birmingham, UK. Sustain. Cities Soc. , 43, 111–120, doi:10.1016/j.scs.2018.08.033.
Kamal, A., et al., 2015: A recipe for change: reclamation of indigenous food sovereignty in O-Pipon-na-Piwin Cree nation for decolonization, resource sharing, and cultural restoration. Globalizations, 12 (4), 559–575, doi:10.1080/14747731.2015.1039761.
Kamal, M., et al., 2018: Mapping the global potential distributions of two arboviral vectors Aedes aegypti and Ae. albopictus under changing climate. PLoS ONE, 13 (12), doi:10.1371/journal.pone.0210122.
Kampe, E.O.I., S. Kovats and S. Hajat, 2016: Impact of high ambient temperature on unintentional injuries in high-income countries: a narrative systematic literature review. BMJ Open, 6 (2), doi:10.1136/bmjopen-2015-010399.
Keim, M., 2008: Building human resilience the role of public health preparedness and response as an adaptation to climate change. Am. J. Prev. Med. , 35 (5), 508–516, doi:10.1016/j.amepre.2008.08.022.
Kelley, C.P., et al., 2015: Climate change in the Fertile Crescent and implications of the recent Syrian drought. Proc. Natl. Acad. Sci. U. S. A. , 112 (11), 3241–3246, doi:10.1073/pnas.1421533112.
Kellog, M., 2020: Women Building Resilient Cities in the Context of Climate Change Lessons from Freetown, Sierra Leone. Institute for Women, Peace and Security, Georgetown.
Kelly, F.J., I.S. Mudway and J.C. Fussell, 2021: Air pollution and asthma: critical targets for effective action. Pulm. Ther. , 7 (1), 9–24, doi:10.1007/s41030-020-00138-1.
Kelman, I., J. Field, K. Suri and G.M. Bhat, 2018: Disaster diplomacy in Jammu and Kashmir. Int. J. Disaster Risk Reduct. , 31, 1132–1140.
Kelman, I., et al., 2019: Does climate change influence people’s migration decisions in Maldives?Clim. Change, 153 (1-2), 285–299, doi:10.1007/s10584-019-02376-y.
Kendrovski, V., et al., 2017: Quantifying projected heat mortality impacts under 21st-century warming conditions for selected European countries. Int. J. Environ. Res. Public Health, 14 (7), doi:10.3390/ijerph14070729.
Kennedy, J. and L. King, 2014: The political economy of farmers’ suicides in India: indebted cash-crop farmers with marginal landholdings explain state-level variation in suicide rates. Glob. Health, 10 (1), 16–16, doi:10.1186/1744-8603-10-16.
Kennedy, S., M.P. Kidd, J.T. McDonald and N. Biddle, 2015: The healthy immigrant effect: patterns and evidence from four countries. Int. Migr. Integr. , 16 (2), 317–332, doi:10.1007/s12134-014-0340-x.
Kenney, M. A., A.C. Janetos and G.C. Lough, 2016: Building an integrated U.S. National Climate Indicators System. In: The US National Climate Assessment: Innovations in Science and Engagement [Jacobs, K., S. Moser and J. Buizer(eds.)]. Springer International Publishing, Cham, pp. 85–96. ISBN 978-3319418025.
Kerr, Z.Y., et al., 2020: The epidemiology and management of exertional heat illnesses in high school sports during the 2012/2013–2016/2017 academic years. J. Sport. Rehabil. , 29 (3), 332–338, doi:10.1123/jsr.2018-0364.
Kesetyaningsih, T.W., S. Andarini, Sudarto and H. Pramoedyo, 2018: Determination of environmental factors affecting dengue incidence in Sleman district, Yogyakarta, Indonesia. Afr. J. Infect. Dis. , 12 (1 Suppl), 13–25, doi:10.2101/Ajid.12v1S.3.
Kessler, R.C., et al., 2008: Trends in mental illness and suicidality after Hurricane Katrina. Molecular Psychiatry, 13, 374–384.
Keyes, K., et al., 2014: The burden of loss: unexpected death of a loved one and psychiatric disorders across the life course in a national study. Am. J. Psychiatry, 171 (8), 864–871, doi:10.1176/appi.ajp.2014.13081132.
Khalil, I. A., et al., 2018: Morbidity, mortality, and long-term consequences associated with diarrhoea from Cryptosporidium infection in children younger than 5 years: a meta-analyses study. Lancet Glob. Health, 6 (7), e758–e768, doi:10.1016/s2214-109x(18)30283-3.
Khan, M.R., S. Huq, A.N. Risha, S.S. Alam, , 2021: High-density population and displacement in Bangladesh. Science, 372 (6548), 1290-1293. Available at: http://science.sciencemag.org/content/372/6548/1290.abstract.
Khan, S., et al., 2015: Extreme weather events: Should drinking water quality management systems adapt to changing risk profiles?Water Res. , 85, 124–136, doi:10.1016/j.watres.2015.08.018.
Khanian, M., B. Serpoush and N. Gheitarani, 2019: Balance between place attachment and migration based on subjective adaptive capacity in response to climate change: the case of Famenin County in Western Iran. Clim. Dev. , 11 (1), 69–82, doi:10.1080/17565529.2017.1374238.
Khormi, H. and L. Kumar, 2016: Future malaria spatial pattern based on the potential global warming impact in South and Southeast Asia. Geospat. Health, 11 (3), 290–298, doi:10.4081/gh.2016.416.
Kibret, S., et al., 2016: Malaria and large dams in sub-Saharan Africa: future impacts in a changing climate. Malar. J. , 15, doi:10.1186/s12936-016-1498-9.
Kim, H., et al., 2019a: Difference in temporal variation of temperature-related mortality risk in seven major South Korean cities spanning 1998–2013. Sci. Total Environ. , 656, 986–996, doi:10.1016/j.scitotenv.2018.11.210.
Kim, J., et al., 2016: Effect of climate factors on the childhood pneumonia in Papua New Guinea: a time-series analysis. Int. J. Environ. Res. Public Health, 13 (2), doi:10.3390/ijerph13020213.
Kim, S., B. Fleisher and Y. Sun, 2017: The long-term health effects of fetal malnutrition: evidence from the 1959–1961 China Great Leap Forward famine. Health Econ. , 26 (10), 1264–1277.
Kim, Y., et al., 2019b: Suicide and ambient temperature: a multi-country multi-city study. Environ. Health Perspect. , 127 (11), doi:10.1289/ehp4898.
King, A.D. and D.J. Karoly, 2017: Climate extremes in Europe at 1.5 and 2 degrees of global warming. Environ. Res. Lett. , 12 (11), doi:10.1088/1748-9326/aa8e2c.
King, U. and C. Furgal, 2014: Is hunting still healthy? Understanding the interrelationships between indigenous participation in land-based practices and human-environmental health. Int. J. Environ. Res. Public Health, 11 (6), 5751–5782, doi:10.3390/ijerph110605751.
Kinney, P., 2018: Temporal trends in heat-related mortality: implications for future projections. Atmosphere, 9, 409, doi:10.3390/atmos9100409.
Kipp, A., et al., 2019: The need for community-led, integrated and innovative monitoring programmes when responding to the health impacts of climate change. Int. J. Circumpolar Health, 78 (2), doi:10.1080/22423982.2018.1517581.
Kirtman, B., et al., 2014: Near-term climate change: projections and predictability. In: Climate Change 2013: The Physical Science Basis, Cambridge University Press, Cambridge. pp. 953–1028.
Kita, S.M., 2017: Urban vulnerability, disaster risk reduction and resettlement in Mzuzu city, Malawi. Int. J. Disaster Risk Reduct. , 22, 158–166.
Kjellstrom, T., et al., 2016: Heat, human performance, and occupational health: a key issue for the assessment of global climate change impacts. Annu. Rev. Public Health, 37 (1), 97–112, doi:10.1146/annurev-publhealth-032315-021740.
Kjellstrom, T., et al., 2018: Estimating population heat exposure and impacts on working people in conjunction with climate change. Int. J. Biometeorol. , 62 (3), 291–306, doi:10.1007/s00484-017-1407-0.
Kjellstrom, T., B. Lemke and J. Lee, 2019: Workplace heat: an increasing threat to occupational health and productivity. Am. J. Ind. Med. , 62 (12), 1076–1078, doi:10.1002/ajim.23051.
Klein, T., et al., 2019: A nation-wide analysis of tree mortality under climate change: forest loss and its causes in Israel 1948–2017. For. Ecol. Manag. , 432, 840–849, doi:10.1016/j.foreco.2018.10.020.
Koc, C.B., P. Osmond and A. Peters, 2018: Evaluating the cooling effects of green infrastructure: a systematic review of methods, indicators and data sources. Sol. Energy, 166, 486–508, doi:10.1016/j.solener.2018.03.008.
Koren, O., B. Bagozzi and T. Benson, 2021: Food and water insecurity as causes of social unrest: evidence from geolocated Twitter data. J. Peace Res. , 58 (1), 67–82, doi:10.1177/0022343320975091.
Koren, O. and B.E. Bagozzi, 2017: Living off the land: the connection between cropland, food security, and violence against civilians. J. Peace Res. , 54 (3), 351–364, doi:10.1177/0022343316684543.
Koslov, L., A.Merdjanoff, E. Sulakshana and E.Klinenberg, 2021: When rebuilding no longer means recovery: the stress of staying put after Hurricane Sandy. Clim. Change, 165 (3), 59, doi:10.1007/s10584-021-03069-1.
Kostyla, C., R. Bain, R. Cronk and J. Bartram, 2015: Seasonal variation of fecal contamination in drinking water sources in developing countries: a systematic review. Sci. Total Environ. , 514, 333–343, doi:10.1016/j.scitotenv.2015.01.018.
Koubi, V., 2019: Climate change and conflict. In: Annual Review of Political Science[Levi, M. and N.L. Rosenblum(eds.)] Vol.22, Annual Reviews, Palo Alto, pp. 343–360.
Koubi, V., T. Bˆhmelt, G. Spilker and L. Schaffer, 2018: The determinants of environmental migrants’ conflict perception. Int. Organ. , 72 (4), 905–936.
Koubi, V., Q. Nguyen, G. Spilker and T. Bohmelt, 2021: Environmental migrants and social-movement participation. J. Peace Res. , 58 (1), 18–32, doi:10.1177/0022343320972153.
Koubi, V., Q.S. Nguyen and G.T. Böhmelt, 2020: Environmental migrants and social-movement participation. J. Peace Res. , 58 (1), 18–32.
Koubi, V., G. Spilker, L. Schaffer and T. Bernauer, 2016a: Environmental stressors and migration: evidence from Vietnam. World Dev. , 79, 197–210, doi:10.1016/j.worlddev.2015.11.016.
Koubi, V., G. Spilker, L. Schaffer and T. Böhmelt, 2016b: The role of environmental perceptions in migration decision-making: evidence from both migrants and non-migrants in five developing countries. Popul. Environ. , 38 (2), 134–163, doi:10.1007/s11111-016-0258-7.
Kousky, C., 2016: Impacts of natural disasters on children. Future Child. , 26 (1), 73–92, doi:10.1353/foc.2016.0004.
Kovach, T. and K. Conca, 2016: Environmental priorities in post-conflict recovery: efficacy of the needs-assessment process. J. Peacebuild. Dev. , 11 (2), 4–24.
Kowalczewski, E. and J. Klein, 2018: Sámi youth health, the role of climate change, and unique health-seeking behaviour. Int. J. Circumpolar Health, 77 (1), 1454785, doi:10.1080/22423982.2018.1454785.
Kraemer, M., et al., 2019: Past and future spread of the arbovirus vectors Aedes aegypti and Aedes albopictus. Nat. Microbiol. , 4 (5), 854–863, doi:10.1038/s41564-019-0376-y.
Krakauer, N.Y., B.I. Cook and M.J. Puma, 2020: Effect of irrigation on humid heat extremes. Environ. Res. Lett. , 15 (9), doi:10.1088/1748-9326/ab9ecf.
Krampe, F., 2017: Toward sustainable peace: a new research agenda for post-conflict natural resource management. Glob. Environ. Polit. , 17 (4), 1–8.
Krampe, F. and S. Gignoux, 2018: Water service provision and peacebuilding in East Timor: exploring the socioecological determinants for sustainings, V peace. J. Interv. Statebuild. , 12 (2), 185–207.
Krampe, F., F. Hegazi and S.D. VanDeveer, 2021: Sustaining peace through better resource governance: three potential mechanisms for environmental peacebuilding. World Dev. , 144, 105508.
Krause, J., W. Krause and P. Bränfors, 2018: Women’s participation in peace negotiations and the durability of peace. Int. Interact. , 44 (6), 985–1016.
Kreppel, K.S., et al., 2014: A non-stationary relationship between global climate phenomena and human plague incidence in Madagascar. PLoS Negl. Trop. Dis. , 8 (10), doi:10.1371/journal.pntd.0003155.
Kron, A., 2019: Environmental Peacebuilding and the UN Security Council[Schrijver, N. J. and N. M. Blokker (eds.)]. Nijhoff Law Specials, Netherlandol. 29. Brill, 248–266.
Krug, A., D. Fenner, A. Holtmann and D. Scherer, 2019: Occurrence and coupling of heat and ozone events and their relation to mortality rates in Berlin, Germany, between 2000 and 2014. Atmosphere, 10 (6), doi:10.3390/atmos10060348.
Krug, A., D. Fenner, H.G. Mucke and D. Scherer, 2020: The contribution of air temperature and ozone to mortality rates during hot weather episodes in eight German cities during the years 2000 and 2017. Nat. Hazards Earth Syst. Sci. , 20 (11), 3083–3097, doi:10.5194/nhess-20-3083-2020.
Kubik, Z. and M. Maurel, 2016: Weather shocks, agricultural production and migration: evidence from Tanzania. J. Dev. Stud. , 52 (5), 665–680, doi:10.1080/00220388.2015.1107049.
Kuehn, L. and S. McCormick, 2017: Heat exposure and maternal health in the face of climate change. Int. J. Environ. Res. Public Health, 14 (8), doi:10.3390/ijerph14080853.
Kuhnlein, H., B. Erasmus and D. Spigelski, 2013: Indigenous Peoples’ Food Systems & Well-Being. Interventions & Policies for Healthy Communities. Agriculture Organization United Nations, Rome.
Kumar, A., et al., 2018a: Mercury from wildfires: Global emission inventories and sensitivity to 2000–2050 global change. Atmos. Environ. , 173, 6–15, doi:10.1016/j.atmosenv.2017.10.061.
Kumar, J.C., V. Gupta, U. Chattopadhyay and B.A. Sreeraman, 2018b: Migration as adaptation strategy to cope with climate change: a study of farmers’ migration in rural India. Int. J. Clim. Change Strateg. Manag. , 10 (1), 121–141, doi:10.1108/ijccsm-03-2017-0059.
Kumar, P., et al., 2019: The nexus between air pollution, green infrastructure and human health. Environ. Int. , 133, doi:10.1016/j.envint.2019.105181.
Kumar, S., R. Molitor and S. Vollmer, 2016: Drought and early child health in rural India. Popul. Dev. Rev. , 42 (1), 53–68.
Kupferberg, J.S., 2021: Migration and dignity – relocation and adaptation in the face of climate change displacement in the Pacific – a human rights perspective. Int. J. Hum. Rights, 1–26, doi:10.1080/13642987.2021.1889515.
Kuusaana, E.D. and K.N. Bukari, 2015: Land conflicts between smallholders and Fulani pastoralists in Ghana: evidence from the Asante Akim North District (AAND). J. Rural Stud. , 42, 52–62.
Lacey, G., et al., 2017: Transient climate and ambient health impacts due to national solid fuel cookstove emissions. Proc. Natl. Acad. Sci. U.S.A. , 114 (6), 1269–1274, doi:10.1073/pnas.1612430114.
Lafond, K.E., et al., 2021: Global burden of influenza-associated lower respiratory tract infections and hospitalizations among adults: a systematic review and meta-analysis. PLoS Med. , 18 (3), doi:10.1371/journal.pmed.1003550.
Lai, D.Y., et al., 2019: A review of mitigating strategies to improve the thermal environment and thermal comfort in urban outdoor spaces. Sci. Total Environ. , 661, 337–353, doi:10.1016/j.scitotenv.2019.01.062.
Lai, Y.H., 2018: The climatic factors affecting dengue fever outbreaks in southern Taiwan: an application of symbolic data analysis. Biomed. Eng. Online, 17 (Suppl 2), 148, doi:10.1186/s12938-018-0575-4.
Lake, A.A., 2018: Neighbourhood food environments: food choice, foodscapes and planning for health. Proc. Nutr. Soc. , 77 (3), 239–246, doi:10.1017/s0029665118000022.
Lake, I.R., 2017: Food-borne disease and climate change in the United Kingdom. Environ. Health, 16 (Suppl 1), 117, doi:10.1186/s12940-017-0327-0.
Lake, I.R. and G.C. Barker, 2018: Climate change, foodborne pathogens and illness in higher-income countries. Curr. Environ. Health Rep. , 5 (1), 187–196, doi:10.1007/s40572-018-0189-9.
Lake, I.R., et al., 2019: Exploring campylobacter seasonality across Europe using The European Surveillance System (TESSy) 2008 to 2016. Euro Surveill. , 24 (13), doi:10.2807/1560-7917.es.2019.24.13.180028.
Lake, I.R., et al., 2017: Climate change and future pollen allergy in Europe. Environ. Health Perspect. , 125 (3), 385–391, doi:10.1289/ehp173.
Lake, L., et al., 2015: The effects of flooding on dioxin and PCB levels in food produced on industrial river catchments. Environ. Int. , 77, 106–115, doi:10.1016/j.envint.2015.01.006.
Lal, A., E. Fearnley and E. Wilford, 2019: Local weather, flooding history and childhood diarrhoea caused by the parasite Cryptosporidium spp.: a systematic review and meta-analysis. Sci. Total Environ. , 674, 300–306, doi:10.1016/j.scitotenv.2019.02.365.
Lal, A., et al., 2016: Spatial and temporal variation in the association between temperature and salmonellosis in NZ. Aust. N. Z. J. Public Health, 40 (2), 165–169, doi:10.1111/1753-6405.12413.
Lam, E.K.S., et al., 2020: The impact of climate and antigenic evolution on seasonal influenza virus epidemics in Australia. Nat. Commun. , 11 (1), doi:10.1038/s41467-020-16545-6.
Lambert, H., et al., 2020: COVID-19 as a global challenge: towards an inclusive and sustainable future. Lancet Planet. Health, 4 (8), E312–E314, doi:10.1016/s2542-5196(20)30168-6.
Laporta, G., et al., 2015: Malaria vectors in South America: current and future scenarios. Parasites Vectors, 8, doi:10.1186/s13071-015-1038-4.
Lawson, E., R. Alare, A. Salifu and M. Thompson-Hall, 2019: Dealing with climate change in semi-arid Ghana: understanding intersectional perceptions and adaptation strategies of women farmers. GeoJournal, doi:10.1007/s10708-019-09974-4.
Lazzaroni, S. and N. Wagner, 2016: Misfortunes never come singly: structural change, multiple shocks and child malnutrition in rural Senegal. Econ. Hum. Biol. , 23, 246–262, doi:10.1016/j.ehb.2016.10.006.
Le Masson, V., C. Benoudji and S. Reyes, 2019: Everyday Violence and its Impact on Insecurity and Resilience in Chad. UNEP, Nairobi.
Le Masson, V., et al., 2016: Gender Resilience from Theory to Practice. Building Resilience and Adaptation to Climate Extremes and Disasters. Overseas Development Institute, London, 60 pp.
Le, P., et al., 2019: Predicting the direct and indirect impacts of climate change on malaria in coastal Kenya. PLoS ONE, 14 (2), doi:10.1371/journal.pone.0211258.
Leard, B. and K. Roth, 2019: Voluntary exposure benefits and the costs of climate change. J. Assoc. Environ. Resour. Econ. , 6 (1), 151–185, doi:10.1086/700268.
Lee, E.C., et al., 2019: The projected impact of geographic targeting of oral cholera vaccination in sub-Saharan Africa: a modeling study. PLoS Med. , 16 (12), e1003003, doi:10.1371/journal.pmed.1003003.
Lee, J., S. Lee and X. Jiang, 2017a: Cyanobacterial toxins in freshwater and food: important sources of exposure to humans. Annu. Rev. Food Sci. Technol. , 8, 281–304, doi:10.1146/annurev-food-030216-030116.
Lee, J.S., et al., 2017b: Early warning signal for dengue outbreaks and identification of high risk areas for dengue fever in Colombia using climate and non-climate datasets. BMC Infect. Dis. , 17 (1), 480, doi:10.1186/s12879-017-2577-4.
Lee, J.Y. and H. Kim, 2016: Projection of future temperature-related mortality due to climate and demographic changes. Environ. Int. , 94, 489–494, doi:10.1016/j.envint.2016.06.007.
Lee, S., et al., 2018a: Mental disease-related emergency admissions attributable to hot temperatures. Sci. Total Environ. , 616, 688–694.
Lee, S.H., et al., 2021: Trends in recent waterborne and foodborne disease outbreaks in South Korea, 2015–2019. Osong Public Health Res. Perspect. , 12 (2), 73–79, doi:10.24171/j.phrp.2021.12.2.04.
Lee, W., et al., 2018b: Temporal changes in mortality attributed to heat extremes for 57 cities in Northeast Asia. Sci. Total Environ. , 616-617, 703–709, doi:10.1016/j.scitotenv.2017.10.258.
Lee, W., et al., 2020: Projections of excess mortality related to diurnal temperature range under climate change scenarios: a multi-country modelling study. Lancet Planet. Health, 4 (11), E512–E521.
Leedale, J., et al., 2016: Projecting malaria hazard from climate change in eastern Africa using large ensembles to estimate uncertainty. Geospat. Health, 11 (1 Suppl), 393, doi:10.4081/gh.2016.393.
Lei, X.N., et al., 2021: Temperature changes between neighboring days and childhood asthma: a seasonal analysis in Shanghai, China. Int. J. Biometeorol. , 65 (6), 827–836, doi:10.1007/s00484-020-02057-x.
Leichenko, R. and J.A. Silva, 2014: Climate change and poverty: vulnerability, impacts, and alleviation strategies. Wiley Interdiscip. Rev. Change, 5 (4), 539–556, doi:10.1002/wcc.287.
Leiserowitz, A., et al., 2017: Climate Change in the American Mind: October 2017. Yale Program on Climate Change Communication. Yale University and George Mason University, New Haven, CT.
Lemelin, H., et al., 2010: Climate change, wellbeing and resilience in the Weenusk First Nation at Peawanuck: the Moccasin Telegraph goes global. RRH, 10 (2), 106-123.
León, V.M., R. Moreno-González, V. García and J.A. Campillo, 2017: Impact of flash flood events on the distribution of organic pollutants in surface sediments from a Mediterranean coastal lagoon (Mar Menor, SE Spain). Environ. Sci. Pollut. Res. Int. , 24 (5), 4284–4300, doi:10.1007/s11356-015-4628-y.
Lerner, H. and C. Berg, 2015: The concept of health in One Health and some practical implications for research and education: what is One Health?Infect. Ecol. Epidemiol. , 5, 25300, doi:10.3402/iee.v5.25300.
Levi, M., T. Kjellstrom and A. Baldasseroni, 2018: Impact of climate change on occupational health and productivity: a systematic literature review focusing on workplace heat. Med. Lav. , 109, doi:10.23749/mdl.v109i3.6851.
Levy, A., 2016: Climate change, urban heat islands and health effects: urban planning in Paris. Environ. Risques Sante, 15 (4), 351–356, doi:10.1684/ers.2016.0888.
Levy, B.S. and J.A. Patz, 2015: Climate change, human rights, and social justice. Ann. Glob. Health, 81 (3), 310–322, doi:10.1016/j.aogh.2015.08.008.
Levy, K., S.M. Smith and E.J. Carlton, 2018: Climate change impacts on waterborne diseases: moving toward designing interventions. Curr. Environ. Health Rep. , 5 (2), 272–282, doi:10.1007/s40572-018-0199-7.
Levy, K., A.P. Woster, R.S. Goldstein and E.J. Carlton, 2016: Untangling the impacts of climate change on waterborne diseases: a systematic review of relationships between diarrheal diseases and temperature, rainfall, flooding, and drought. Environ. Sci. Technol. , 50 (10), 4905–4922, doi:10.1021/acs.est.5b06186.
Lewis, D., L. Williams and R. Jones, 2020: A radical revision of the public health response to environmental crisis in a warming world: contributions of Indigenous knowledges and Indigenous feminist perspectives. Can. J. Public Health, 111 (6), 897–900, doi:10.17269/s41997-020-00388-1.
Leyk, S., et al., 2017: Internal and international mobility as adaptation to climatic variability in contemporary Mexico: evidence from the integration of census and satellite data. Popul. Space Place, doi:10.1002/psp.2047.
Li, C. and Z. Zhu, 2018: Research and application of a novel hybrid air quality early-warning system: a case study in China. Sci. Total Environ. , 626, 1421–1438, doi:10.1016/j.scitotenv.2018.01.195.
Li, M., S. Ferreira and T. Smith, 2020: Temperature and self-reported mental health in the United States. PLoS ONE, 15 (3), doi:10.1371/journal.pone.0230316.
Li, T., et al., 2015: Heat-related mortality projections for cardiovascular and respiratory disease under the changing climate in Beijing, China. Sci. Rep. , 5, 11441, doi:10.1038/srep11441. https://www.nature.com/articles/srep11441#supplementary-information.
Li, X.Q., L.C. Stringer and M. Dallimer, 2021: The spatial and temporal characteristics of urban heat island intensity: implications for East Africa’s urban development. Climate, 9 (4), doi:10.3390/cli9040051.
Li, Y., et al., 2014: Extremely cold and hot temperatures increase the risk of diabetes mortality in metropolitan areas of two Chinese cities. Environ. Res. , 134, 91–97, doi:10.1016/j.envres.2014.06.022.
Li, Y., et al., 2018: Projecting future climate change impacts on heat-related mortality in large urban areas in China. Environ. Res. , 163, 171–185, doi:10.1016/j.envres.2018.01.047.
Liang, L. and P. Gong, 2017: Climate change and human infectious diseases: a synthesis of research findings from global and spatio-temporal perspectives. Environ. Int. , 103, 99–108.
Liang, W., et al., 2018: Mapping the epidemic changes and risks of hemorrhagic fever with renal syndrome in Shaanxi Province, China, 2005–2016. Sci. Rep. , 8 (1), 749, doi:10.1038/s41598-017-18819-4.
Ligon, G. and J. Bartram, 2016: Literature review of associations among attributes of reported drinking water disease outbreaks. Int. J. Environ. Res. Public Health, 13 (6), doi:10.3390/ijerph13060527.
Lim, T.K. and W.T. Siow, 2018: Pneumonia in the tropics. Respirology, 23 (1), 28–35, doi:10.1111/resp.13137.
Lim, Y., et al., 2015: Effects of cold and hot temperature on dehydration: a mechanism of cardiovascular burden. Int. J. Biometeorol. , 59 (8), 1035–1043, doi:10.1007/s00484-014-0917-2.
Limaye, V.S., et al., 2018: Climate change and heat-related excess mortality in the eastern USA. EcoHealth, 15 (3), 485–496, doi:10.1007/s10393-018-1363-0.
Lin, H.L., et al., 2013: Temperature changes between neighboring days and mortality in summer: a distributed lag non-linear time series analysis. Plos One, 8 (6), doi:10.1371/journal.pone.0066403.
Lin, S., M. Sun, E. Fitzgerald and S.A. Hwang, 2016: Did summer weather factors affect gastrointestinal infection hospitalizations in New York State?Sci. Total Environ. , 550, 38–44.
Linke, A.M., et al., 2018: The consequences of relocating in response to drought: human mobility and conflict in contemporary Kenya. Environ. Res. Lett. , 13 (9), 94014.
Liu-Helmersson, J., et al., 2019: Estimating past, present, and future trends in the global distribution and abundance of the arbovirus vector Aedes aegypti under climate change scenarios. Front. Public Health, 7, doi:10.3389/fpubh.2019.00148.
Liu-Helmersson, J., et al., 2016: Climate change and Aedes vectors: 21st century projections for dengue transmission in Europe. EBioMedicine, 7, 267–277, doi:10.1016/j.ebiom.2016.03.046.
Liu, C., Z. Yavar and Q. Sun, 2015a: Cardiovascular response to thermoregulatory challenges. Am. J. Physiol. Circ. Physiol. , 309 (11), H1793–H1812, doi:10.1152/ajpheart.00199.2015.
Liu, K., et al., 2015b: A national assessment of the epidemiology of severe fever with thrombocytopenia syndrome, China. Sci. Rep. , 5, 9679, doi:10.1038/srep09679.
Liu, Q., et al., 2020a: Changing rapid weather variability increases influenza epidemic risk in a warming climate. Environ. Res. Lett. , 15 (4), doi:10.1088/1748-9326/ab70bc.
Liu, X., 2020: Reductions in labor capacity from intensified heat stress in China under future climate change. Int. J. Environ. Res. Public Health, 17 (4), doi:10.3390/ijerph17041278.
Liu, Y., et al., 2014: Temporal relationship between hospital admissions for pneumonia and weather conditions in Shanghai, China: a time-series analysis. BMJ Open, 4 (7), doi:10.1136/bmjopen-2014-004961.
Liu, Y., et al., 2020b: Natural outdoor environment, neighbourhood social cohesion and mental health: using multilevel structural equation modelling, streetscape and remote-sensing metrics. Urban For. Urban Green. , 48, doi:10.1016/j.ufug.2019.126576.
Liu, Z., et al., 2017: Global and regional changes in exposure to extreme heat and the relative contributions of climate and population change. Sci. Rep. , 7, doi:10.1038/srep43909.
Liu, Z., et al., 2018: Association between floods and infectious diarrhea and their effect modifiers in Hunan province, China: a two-stage model. Sci. Total Environ. , 626, 630–637, doi:10.1016/j.scitotenv.2018.01.130.
Liverpool-Tasie, L.S.O., T. Reardon and B. Belton, 2021: “Essential non-essentials”: COVID-19 policy missteps in Nigeria rooted in persistent myths about African food supply chains. Appl. Econ. Perspect. Policy, 43 (1), 205–224, doi:10.1002/aepp.13139.
Lloyd, 2018: A global-level model of the potential impacts of climate change on child stunting via income and food price in 2030. Environ. Health Perspect. , 126 (9), 97007, doi:10.1289/ehp2916.
Lo Iacono, G., et al., 2017: Challenges in developing methods for quantifying the effects of weather and climate on water-associated diseases: a systematic review. PLoS Negl. Trop. Dis. , 11 (6), doi:10.1371/journal.pntd.0005659.
Loebach, P., 2016: Household migration as a livelihood adaptation in response to a natural disaster: Nicaragua and Hurricane Mitch. Popul. Environ, 38(2), 185-206
Lopez-i-Gelats, F., et al., 2015: Adaptation strategies of Andean pastoralist households to both climate and non-climate changes. Hum. Ecol. , 43 (2), 267–282, doi:10.1007/s10745-015-9731-7.
Lopez, M.S., G.V. Muller and W.F. Sione, 2018: Analysis of the spatial distribution of scientific publications regarding vector-borne diseases related to climate variability in South America. Spat. Spatiotemp. Epidemiol. , 26, 35–93, doi:10.1016/j.sste.2018.04.003.
Lovell, R., M. Depledge and S. Maxwell, 2018: Health and the Natural Environment: a Review of Evidence, Policy, Practice and Opportunities for the Future. Department for Environment, Food and Rural Affairs (DFRA), London.
Lu, J.G., 2020: Air pollution: a systematic review of its psychological, economic, and social effects. Curr. Opin. Psychol. , 32, 52–65, doi:10.1016/j.copsyc.2019.06.024.
Lu, P., et al., 2021: Temporal trends of the association between ambient temperature and cardiovascular mortality: a 17-year case-crossover study. Environ. Res. Lett. , 16 (4), doi:10.1088/1748-9326/abab33.
Lu, X., et al., 2016: Detecting climate adaptation with mobile network data in Bangladesh: anomalies in communication, mobility and consumption patterns during Cyclone Mahasen. Clim. Change, 138 (3-4), 505–519.
Luechinger, S., 2010: Life satisfaction and transboundary air pollution. Econ. Lett. , 107 (1), 4–6, doi:10.1016/j.econlet.2009.07.007.
Lund, C., E. Baron and E. Breuer, 2018: Social determinants of mental disorders and the Sustainable Development Goals: a systematic review of reviews. Lancet Psychiatry, 5,357-369.
Lundgren, A.D., 2018: Climate change and skin disease. Cutis, 101 (4), E12–E14.
Lynch, M.J., P.B. Stretesky, M. A. Long and K.L. Barrett, 2020: The climate change-temperature-crime hypothesis: evidence from a sample of 15 large US cities, 2002 to 2015. Int. J. Offender Ther. Comp. Criminol. DOI: https://doi.org/10.1177/0306624X20969934
M’Bra, R.K., et al., 2018: Impact of climate variability on the transmission risk of malaria in northern Cote d’Ivoire. PLoS ONE, 13 (6), e182304, doi:10.1371/journal.pone.0182304.
Ma, F. and X. Yuan, 2021: Impact of climate and population changes on the increasing exposure to summertime compound hot extremes. Sci. Total. Environ. , 772, doi:10.1016/j.scitotenv.2021.145004.
Ma, R., et al., 2019: Estimation of work-related injury and economic burden attributable to heat stress in Guangzhou, China. Sci. Total Environ. , 666, 147–154, doi:10.1016/j.scitotenv.2019.02.201.
Macdiarmid, J. and S. Whybrow, 2019: Nutrition from a climate change perspective. Proc. Nutr. Soc. , 78 (3), 380–387, doi:10.1017/s0029665118002896.
MacFadden, D., et al., 2018: Antibiotic resistance increases with local temperature. Nat. Clim. Change, 8 (6), 510, doi:10.1038/s41558-018-0161-6.
Mach, K., et al., 2019: Climate as a risk factor for armed conflict. Nature, 571 (7764), 193, doi:10.1038/s41586-019-1300-6.
Mach, K.J., et al., 2020: Directions for research on climate and conflict. Earth’s Future. DOI: https://doi.org/10.1029/2020EF001532
Machalaba, C., et al., 2015: Climate change and health: transcending silos to find solutions. Ann. Glob. Health. , 81 (3), 445–458, doi:10.1016/j.aogh.2015.08.002.
Macintyre, H.L. and C. Heaviside, 2019: Potential benefits of cool roofs in reducing heat-related mortality during heatwaves in a European city. Environ. Int. , 127, 430–441, doi:10.1016/j.envint.2019.02.065.
Macintyre, H.L., C. Heaviside, X. Cai and R. Phalkey, 2021: The winter urban heat island: Impacts on cold-related mortality in a highly urbanized European region for present and future climate. Environ. Int. , 154, 106530, doi:10.1016/j.envint.2021.106530.
Macintyre, H.L., et al., 2018: Assessing urban population vulnerability and environmental risks across an urban area during heatwaves – implications for health protection. Sci. Total Environ. , 610, 678–690, doi:10.1016/j.scitotenv.2017.08.062.
Mackenzie, J. and M. Jeggo, 2019: The one health approach – why is it so important?Trop. Med. Infect. Dis. , 4 (2), 88, doi:10.3390/tropicalmed4020088.
Maclean, C., I. Popovici and T. French, 2016: Are natural disasters in early childhood associated with mental health and substance use disorders as an adult?Soc. Sci. Med. , 151, 78–91.
Macnaughton, P., et al., 2018: Energy savings, emission reductions, and health co-benefits of the green building movement. J. Expo. Sci. Environ. Epidemiol. , 28 (4), 307–318, doi:10.1038/s41370-017-0014-9.
Macnight Ngwese, N., et al., 2018: Traditional and local knowledge practices for disaster risk reduction in northern Ghana. Sustainability, 10 (3), 825.
Madureira, H., et al., 2021: Evidences on adaptive mechanisms for cardiorespiratory diseases regarding extreme temperatures and air pollution: a comparative systematic review. Geogr. Sustain. , doi:10.1016/j.geosus.2021.08.001.
Magnan, A., et al., 2016: Addressing the risk of maladaptation to climate change. Wiley Interdiscip. Rev. Clim. Change, 7, 646–665, doi:10.1002/wcc.409.
Mahajan, P.Y. and Dean, 2020: Taken by storm: hurricanes, migrant networks and US immigration. Am. Econ. J. Appl. Econ. , 12 (2), 250–277, doi:10.1257/app.20180438.
Maharjan, A., et al., 2020: Migration and household adaptation in climate-sensitive hotspots in South Asia. Curr. Clim. Change Rep. , doi:10.1007/s40641-020-00153-z.
Maini, R., C. Lorcan, B. Kevin and M. Virginia, 2017: The Sendai framework for disaster risk reduction and its indicators—where does health fit in?Int. J. Disaster Risk Sci. , 8 (2), 150–155, doi:10.1007/s13753-017-0120-2.
Maizlish, N., N.J. Linesch and J. Woodcock, 2017: Health and greenhouse gas mitigation benefits of ambitious expansion of cycling, walking, and transit in California. J. Transp. Health, 6, 490–500, doi:10.1016/j.jth.2017.04.011.
Mala, S. and M.K. Jat, 2019: Implications of meteorological and physiographical parameters on dengue fever occurrences in Delhi. Sci. Total Environ. , 650 (Pt 2), 2267–2283, doi:10.1016/j.scitotenv.2018.09.357.
Maldonado, J., et al., 2021: Addressing the challenges of climate-driven community-led resettlement and site expansion: knowledge sharing, storytelling, healing, and collaborative coalition building. J. Environ. Stud. Sci. , 1–11, doi:10.1007/s13412-021-00695-0.
Mall, R.K., et al., 2019: Disaster risk reduction including climate change adaptation over South Asia: challenges and ways forward. Int. J. Disaster Risk Sci. , 10 (1), 14–27, doi:10.1007/s13753-018-0210-9.
Mallick, B., 2019: The nexus between socio-ecological system, livelihood resilience, and migration decisions: empirical evidence from Bangladesh. Sustainability, 11 (12), doi:10.3390/su11123332.
Mallick, B., B. Ahmed and J. Vogt, 2017: Living with the risks of cyclone disasters in the South-Western coastal region of Bangladesh. Environments, 4 (1), 13.
Mallick, B. and J. Schanze, 2020: Trapped or voluntary? Non-migration despite climate risks. Sustainability, 12 (11), doi:10.3390/su12114718.
Mamo, D. (ed.), 2020: The Indigenous World 2020. The International Work Group for Indigenous Affairs (IWGIA), Eks-Skolen Trykkeri, Copenhagen, Denmark, 784 pp.
Manning, C. and S. Clayton, 2018: Threats to mental health and wellbeing associated with climate change, In Psychology and climate change. Academic Press, London, UK, pp.217–244.
Maor, M., 2018: Rhetoric and doctrines of policy over- and underreactions in times of crisis. Policy Polit. , 46 (1), 47–63, doi:10.1332/030557317x14843233064353.
Mapou, A.E.M., et al., 2017: Environmental factors and fluctuations in daily crime rates. J. Environ. Health, 80 (5), 8–22.
Marcus, H. and L. Hanna, 2020: Understanding national barriers to climate change adaptation for public health: a mixed-methods survey of national public health representatives. Int. J. Health Gov. , doi:10.1108/ijhg-06-2020-0061.
Mares, D.M. and K.W. Moffett, 2016: Climate change and interpersonal violence: a “global” estimate and regional inequities. Clim. Change, 135 (2), 297–310.
Mares, D.M. and K.W. Moffett, 2019: Climate change and crime revisited: an exploration of monthly temperature anomalies and UCR crime data. Environ. Behav. , 51 (5), 502–529.
Marinaccio, A., et al., 2019: Nationwide epidemiological study for estimating the effect of extreme outdoor temperature on occupational injuries in Italy. Environ. Int. , 133, 105176.
Maringe, C., et al., 2020: The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. Lancet Oncol. , 21 (8), 1023–1034, doi:10.1016/s1470-2045(20)30388-0.
Marini, G., et al., 2020: A quantitative comparison of West Nile virus incidence from 2013 to 2018 in Emilia-Romagna, Italy. PLoS Negl. Trop. Dis. , 14 (1). DOI: https://doi.org/10.1371/journal.pntd.0007953
Marino, E., 2018: Adaptation privilege and voluntary buyouts: perspectives on ethnocentrism in sea level rise relocation and retreat policies in the US. Glob. Environ. Change Policy Dimens. , 49, 10–13, doi:10.1016/j.gloenvcha.2018.01.002.
Marino, E. and H. Lazrus, 2015: Migration or forced displacement? The complex choices of climate change and disaster migrants in Shishmaref, Alaska and Nanumea, Tuvalu. Hum. Organ. , 74 (4), 341–350.
Marinucci, G.D., et al., 2014: Building resilience against climate effects—a novel framework to facilitate climate readiness in public health agencies. Int. J. Environ. Res. Public Health, 11 (6), 6433–6458, doi:10.3390/ijerph110606433.
Markandya, A., et al., 2018: Health co-benefits from air pollution and mitigation costs of the Paris Agreement: a modelling study. Lancet Planet. Health, 2 (3), e126–e133, doi:10.1016/s2542-5196(18)30029-9.
Markard, J. and D. Rosenbloom, 2020: A tale of two crises: COVID-19 and climate. Sustain. Sci. Pract. Policy, 16 (1), 53–60, doi:10.1080/15487733.2020.1765679.
Markussen, T., M. Fibæk, F. Tarp and N.D.A. Tuan, 2018: The happy farmer: self-employment and subjective well-being in rural Vietnam. J. Happiness Stud. , 19 (6), 1613–1636, doi:10.1007/s10902-017-9858-x.
Marmot, M., et al., 2020: Health Equity in England: The Marmot Review 10 Years on. Institute of Health Equity, London.
Marselle, M., et al., 2020: Urban street tree biodiversity and antidepressant prescriptions. Sci. Rep. , 10 (1), doi:10.1038/s41598-020-79924-5.
Martin-Shields, C.P. and W. Stojetz, 2019: Food security and conflict: empirical challenges and future opportunities for research and policy making on food security and conflict. World Dev. , 119, 150–164.
Martin, L., et al., 2020: Nature contact, nature connectedness and associations with health, wellbeing and pro-environmental behaviours. J. Environ. Psychol. , 68, doi:10.1016/j.jenvp.2020.101389.
Martinez-Solanas, E. and X. Basagana, 2019: Temporal changes in temperature-related mortality in Spain and effect of the implementation of a heat health prevention plan. Environ. Res. , 169, 102–113, doi:10.1016/j.envres.2018.11.006.
Martinez, G.S. and P. Berry, 2018: The Adaptation Health gap: a Global Overview, Adaptation Gap Report 2018. United Nations Environment Programme (unep), Nairobi, Kenya.
Martinez, G.S., et al., 2018: Cold-related mortality vs heat-related mortality in a changing climate: a case study in Vilnius (Lithuania). Environ. Res. , 166, 384–393, doi:10.1016/j.envres.2018.06.001.
Martinez, G.S., et al., 2019: Heat-health action plans in Europe: challenges ahead and how to tackle them. Environ. Res. , 176, doi:10.1016/j.envres.2019.108548.
Mascarenhas, M., et al., 2018: A scoping review of published literature on chikungunya virus. PLoS ONE, 13 (11), e207554, doi:10.1371/journal.pone.0207554.
Masselot, P., et al., 2019: Toward an improved air pollution warning system in Quebec. Int. J. Environ. Res. Public Health, 16 (12), doi:10.3390/ijerph16122095.
Masson, V., A. Lemonsu and J. Voogt, 2018: The 9th International Conference on Urban Climate. Urban Clim. , 23, 1–7, doi:10.1016/j.uclim.2017.07.007.
Mastrorillo, M., et al., 2016: The influence of climate variability on internal migration flows in South Africa. Glob. Environ. Change, 39, 155–169.
Matsushita, N., et al., 2018: The non-linear and lagged short-term relationship between rainfall and leptospirosis and the intermediate role of floods in the Philippines. PLoS Negl. Trop. Dis. , 12 (4), e6331, doi:10.1371/journal.pntd.0006331.
Matthew, R.A., 2018: Climate change adaptation and peacebuilding. In: Routledge Handbook of Environmental Conflict and Peacebuilding. Routledge, New York, pp. 108–120. ISBN 978-1315473772.
Matthews, T., R. Wilby and C. Murphy, 2019: An emerging tropical cyclone-deadly heat compound hazard. Nat. Clim. Change, 9 (8), 602, doi:10.1038/s41558-019-0525-6.
Mayrhuber, E.A., et al., 2018: Vulnerability to heatwaves and implications for public health interventions – a scoping review. Environ. Res. , 166, 42–54, doi:10.1016/j.envres.2018.05.021.
Mbereko, A., M.J. Chimbari, T. Manyangadze and S. Mukaratirwa, 2020: Knowledge and perceptions of schistosomiasis, a water-borne disease, in two semi-arid rural areas of South Africa (Ndumo) and Zimbabwe (Ntalale). Food Waterborne Parasitol. , 21, e91, doi:10.1016/j.fawpar.2020.e00091.
Mbow, C., C. Rosenzweig, L.G. Barioni, T.G. Benton, M. Herrero, M. Krishnapillai, E. Liwenga, P. Pradhan, M.G. Rivera-Ferre, T. Sapkota, F.N. Tubiello, Y. Xu, 2019: Food Security. In: Climate Change and Land: an IPCC special report on climate change, desertification, land degradation, sustainable land management, food security, and greenhouse gas fluxes in terrestrial ecosystems[P.R. Shukla, J. Skea, E. Calvo Buendia, V. Masson-Delmotte, H.-O. Pörtner, D.C. Roberts, P. Zhai, R. Slade, S. Connors, R. van Diemen, M. Ferrat, E. Haughey, S. Luz, S. Neogi, M. Pathak, J. Petzold, J. Portugal Pereira, P. Vyas, E. Huntley, K. Kissick, M. Belkacemi, J. Malley, (eds.)]. Intergovernmental Panel on Climate Change, Geneve.
McAllister, D.A., et al., 2019: Global, regional, and national estimates of pneumonia morbidity and mortality in children younger than 5 years between 2000 and 2015: a systematic analysis. Lancet Glob. Health, 7 (1), E47–E57, doi:10.1016/s2214-109x(18)30408-x.
McCollum, D., et al., 2018: Connecting the sustainable development goals by their energy inter-linkages. Environ. Res. Lett. , 13 (3), doi:10.1088/1748-9326/aaafe3.
McCormack, M.C., et al., 2016: Respiratory effects of indoor heat and the interaction with air pollution in chronic obstructive pulmonary disease. Ann. Am. Thorac. Soc. , 13 (12), 2125–2131, doi:10.1513/AnnalsATS.201605-329OC.
McCreesh, N. and M. Booth, 2014: The effect of increasing water temperatures on Schistosoma mansoni transmission and Biomphalaria pfeifferi population dynamics: an agent-based modelling study. Plos One, 9 (7), doi:10.1371/journal.pone.0101462.
McCreesh, N., G. Nikulin and M. Booth, 2015: Predicting the effects of climate change on Schistosoma mansoni transmission in eastern Africa. Parasites Vectors, 8, 4, doi:10.1186/s13071-014-0617-0.
McCubbin, S., B. Smit and T. Pearce, 2015: Where does climate fit? Vulnerability to climate change in the context of multiple stressors in Funafuti, Tuvalu. Glob. Environ. Change, 30, 43–55.
McEvoy, D., 2019: Climate resilient urban development. Sustainability, 11 (3), doi:10.3390/su11030724.
McGregor, G., K. Ebi, B. Menne and P. Bessmoulin, 2015: Heatwaves and Health Guidance on Warning System Development . World Meteorological Organisation, Geneva.
McGregor, G.R., A. Bone and F. Pappenberger, 2017: Meteorological risk: extreme temperatures. In: Science for Disaster Risk Management 2017: Knowing Better and Losing Less[Poljanšek, K.(ed.)]. European Union, Luxembourg, pp. 257–270.
McGregor, G.R. and K. Ebi, 2018: El Nino southern oscillation (ENSO) and health: an overview for climate and health researchers. Atmosphere, 9 (7), 32, doi:10.3390/atmos9070282.
McGuirk, E. and M. Burke, 2020: The economic origins of conflict in africa. J. Polit. Econ. , 128 (10), 3940–3997, doi:10.1086/709993.
McIver, L., et al., 2016a: Health impacts of climate change in Pacific island countries: a regional assessment of vulnerabilities and adaptation priorities. Environ. Health Perspect. , 124 (11), 1707–1714, doi:10.1289/ehp.1509756.
McIver, L.J., et al., 2016b: Review of climate change and water-related diseases in Cambodia and findings from stakeholder knowledge assessments. Asia Pac. J. Public Health, 28 (2 Suppl), 49S–58S, doi:10.1177/1010539514558059.
McLeman, R., 2017: Thresholds in climate migration. Popul. Environ. , doi:10.1007/s11111-017-0290-2.
McLeman, R., 2019: International migration and climate adaptation in an era of hardening borders. Nat. Clim. Change, 9 (12), 911–918, doi:10.1038/s41558-019-0634-2.
McLeman, R., M. Mohammad and A. Nasima, 2017: Environmental influences on skilled worker migration from Bangladesh to Canada. Can. Geogr. , 62 (3), 352–371, doi:10.1111/cag.12430.
McLeman, R., et al., 2021: Conceptual framing to link climate risk assessments and climate-migration scholarship. Clim. Change, 165 (24), doi:10.1007/s10584-021-03056-6.
McMahon, S., P. Gamage and L.V. Fortington, 2021: Sports related heat injury in Victoria, Australia: an analysis of 11 years of hospital admission and emergency department data. J. Sci. Med. Sport , 24 (3), 224–228, doi:10.1016/j.jsams.2020.08.011.
McMeeking, S. and C. Savage, 2020: Māori responses to Covid-19. Policy Q. , 16 (3), 36–41, doi:10.26686/pq.v16i3.6553.
McMichael, C., 2015: Climate change-related migration and infectious disease. Virulence, 6 (6), 548–553.
McMichael, C., et al., 2021: Rising seas, immobilities, and translocality in small island states: case studies from Fiji and Tuvalu. Popul. Environ. , 43 (1), 82–107, doi:10.1007/s11111-021-00378-6.
McMichael, C., S. Dasgupta, S. Ayeb-Karlsson and I. Kelman, 2020: A review of estimating population exposure to sea-level rise and the relevance for migration. Environ. Res. Lett. , 15 (12), 123005, doi:10.1088/1748-9326/abb398.
McMichael, C. and M. Katonivualiku, 2020: Thick temporalities of planned relocation in Fiji. Geoforum, 108, 286–294, doi:10.1016/j.geoforum.2019.06.012.
McMichael, C. and T. Powell, 2021: Planned relocation and health: a case study from Fiji. Int. J. Environ. Res. Public Health, 18 (8), doi:10.3390/ijerph18084355.
McNamara, K., R. Bronen, N. Fernando and S. Klepp, 2018: The complex decision-making of climate-induced relocation: adaptation and loss and damage. Clim. Policy, 18 (1), 111–117, doi:10.1080/14693062.2016.1248886.
McNamara, K.E., 2015: Cross-border migration with dignity in Kiribati. Forced Migr. Rev. , 49, 62–62.
McNamara, K.E., R. Westoby and A. Chandra, 2021: Exploring climate-driven non-economic loss and damage in the Pacific Islands. Curr. Opin. Environ. Sustain. , 50, 1–11.
McPherson, M., et al., 2017: Expansion of the Lyme disease vector Ixodes scapularis in Canada inferred from CMIP5 climate projections. Environ. Health Perspect. , 125 (5), doi:10.1289/ehp57.
McTavish, R.K., et al., 2018: Association between high environmental heat and risk of acute kidney injury among older adults in a northern climate: a matched case-control study. Am. J. Kidney Dis. , 71 (2), 200–208, doi:10.1053/j.ajkd.2017.07.011.
Medek, S., E. Danielle, J. Schwartz andS. S. Myers, 2017: Estimated effects of future atmospheric CO2 concentrations on protein intake and the risk of protein deficiency by country and region. Environ. Health Perspect. , 125 (8), 87002, doi:10.1289/ehp41.
Meehl, G.A., et al., 2018: Future heat waves and surface ozone. Environ. Res. Lett. , 13 (6), doi:10.1088/1748-9326/aabcdc.
Meige, P., R. Blewitt and M.K. van Aalst, 2020: A Humanitarian Recipe for a Green, Resilient and Inclusive Recovery from COVID-19. Solferino Academy, Geneva.
Méndez-Lázaro, P.A., et al., 2018: Climate change, heat, and mortality in the tropical urban area of San Juan, Puerto Rico. Int. J. Biometeorol. , 62 (5), 699–707, doi:10.1007/s00484-016-1291-z.
Mendez, M., G. Flores-Haro and L. Zucker, 2020: The (in)visible victims of disaster: understanding the vulnerability of undocumented Latino/a and indigenous immigrants. Geoforum, 116, 50–62, doi:10.1016/j.geoforum.2020.07.007.
Menz, T. and H. Welsch, 2010: Population aging and environmental preferences in OECD countries: the case of air pollution. Ecol. Econ. , 69 (12), 2582–2589, doi:10.1016/j.ecolecon.2010.08.002.
Mercer, N. and M. Hanrahan, 2017: “Straight from the heavens into your bucket”: domestic rainwater harvesting as a measure to improve water security in a subarctic indigenous community. Int. J. Circumpolar Health, 76 (1).DOI: https://doi.org/10.1080/22423982.2017.1312223
Merkens, J., et al., 2018: Regionalisation of population growth projections in coastal exposure analysis. Clim. Change, 151 (3-4), 413–426, doi:10.1007/s10584-018-2334-8.
Merkord, C.L., et al., 2017: Integrating malaria surveillance with climate data for outbreak detection and forecasting: the EPIDEMIA system. Malar. J. , 16 (1), 89, doi:10.1186/s12936-017-1735-x.
Messeri, A., et al., 2021: A web survey to evaluate the thermal stress associated with personal protective equipment among healthcare workers during the COVID-19 pandemic in Italy. Int. J. Environ. Res. Public Health, 18 (8), doi:10.3390/ijerph18083861.
Messina, J., et al., 2019: The current and future global distribution and population at risk of dengue. Nat. Microbiol. , 4 (9), 1508–1515, doi:10.1038/s41564-019-0476-8.
Messina, J.P., et al., 2015: The many projected futures of dengue. Nat. Rev. Microbiol, 13 (4), 230–239, doi:10.1038/nrmicro3430.
Metallinou, M.-M. and T. Log, 2017: Health impacts of climate change-induced subzero temperature fires. Int. J. Environ. Res. Public Health, 14 (7), doi:10.3390/ijerph14070814.
Mezdour, A., L. Veronis and R. McLeman, 2015: Environmental Influences on Haitian Migration to Canada and Connections to Social Inequality: Evidence from Ottawa-Gatineau and Montreal[McLeman, R., J. Schade and T. Faist (eds.)]. Springer, Dordrecht, 103–116.
Miao, Y.F., et al., 2017: Maternal exposure to ambient air temperature during pregnancy and early childhood pneumonia. J. Therm. Biol. , 69, 288–293, doi:10.1016/j.jtherbio.2017.09.001.
Middleton, J., et al., 2020a: “We’re people of the snow:” weather, climate change, and Inuit mental wellness. Soc. Sci. Med. , 262, doi:10.1016/j.socscimed.2020.113137.
Middleton, J., et al., 2020b: Indigenous mental health in a changing climate: a systematic scoping review of the global literature. Environ. Res. Lett. , 15 (5), doi:10.1088/1748-9326/ab68a9.
Midekisa, A., et al., 2015: Seasonal associations of climatic drivers and malaria in the highlands of Ethiopia. Parasites Vectors, 8, doi:10.1186/s13071-015-0954-7.
Milazzo, A., et al., 2016: Heatwaves differentially affect risk of Salmonella serotypes. J. Infect. , 73 (3), 231–240, doi:10.1016/j.jinf.2016.04.034.
Miles-Novelo, A. and C. Anderson, 2019: Climate change and psychology: effects of rapid global warming on violence and aggression. Curr. Clim. Change Rep. , 5 (1), 36–46, doi:10.1007/s40641-019-00121-2.
Milner, J., et al., 2015: Health effects of adopting low greenhouse gas emission diets in the UK. BMJ Open, 5 (4), doi:10.1136/bmjopen-2014-007364.
Milner, J., et al., 2017: Projected health effects of realistic dietary changes to address freshwater constraints in India: a modelling study. Lancet Planet. Health, 1 (1), e26–e32, doi:10.1016/S2542-5196(17)30001-3.
Miltenburg, E., et al., 2021: Seed Sowing: Indigenous Relationship-Building as Processes of Environmental Action. Canadian Institute for Climate Choices, Ottawa.
Miner, K.R., et al., 2018: Quantitative screening level assessment of human risk from PCBs released in glacial meltwater: Silvretta Glacier, Swiss Alps. Ecotoxicol. Environ. Saf. , 166, 251–258, doi:10.1016/j.ecoenv.2018.09.066.
Mirasgedis, S., C. Tourkolias, E. Pavlakis and D. Diakoulaki, 2014: A methodological framework for assessing the employment effects associated with energy efficiency interventions in buildings. Energy Build. , 82, 275–286, doi:10.1016/j.enbuild.2014.07.027.
Miron, I.J., et al., 2015: Changes in cause-specific mortality during heat waves in central Spain, 1975–2008. Int. J. Biometeorol. , 59 (9), 1213–1222, doi:10.1007/s00484-014-0933-2.
Mirsaeidi, M., et al., 2016: Climate change and respiratory infections. Ann. ATS, 13 (8), 1223–1230, doi:10.1513/AnnalsATS.201511-729 PS.
Mirumachi, N., A. Sawas and M. Workman, 2020: Unveiling the security concerns of low carbon development: climate security analysis of the undesirable and unintended effects of mitigation and adaptation. Clim. Dev. , 12 (2), 97–109.
Mishra, V., S. Mukherjee, R. Kumar and D.A. Stone, 2017: Heat wave exposure in India in current, 1.5 degrees C, and 2.0 degrees C worlds. Environ. Res. Lett. , 12 (12), doi:10.1088/1748-9326/aa9388.
Missirian, A. and W. Schlenker, 2017: Asylum applications respond to temperature fluctuations. Science, 358 (6370), 1610–1614.
Mitchell, D., 2016: Human influences on heat-related health indicators during the 2015 Egyptian heat wave. Bull. Am. Meteorol. Soc. , 97, 70–S74, doi:10.1175/bams-d-16-0132.1.
Mitchell, D., 2021: Climate attribution of heat mortality. Nat. Clim. Change, 11 (6), 467–468, doi:10.1038/s41558-021-01049-y.
Mitchell, D., et al., 2018: Extreme heat-related mortality avoided under Paris Agreement goals. Nat. Clim. Change, 8 (7), 551–553, doi:10.1038/s41558-018-0210-1.
Mitchell, D., et al., 2016: Attributing human mortality during extreme heat waves to anthropogenic climate change. Environ. Res. Lett. , 11, doi:10.1088/1748-9326/11/7/074006.
Miyayo, S.F., P.O. Owili, M. A. Muga and T.H. Lin, 2021: Analysis of pneumonia occurrence in relation to climate change in Tanga, Tanzania. Int. J. Environ. Res. Public Health, 18 (9), doi:10.3390/ijerph18094731.
Modenese, A., L. Korpinen and F. Gobba, 2018: Solar radiation exposure and outdoor work: an underestimated occupational risk. Int. J. Environ. Res. Public Health, 15 (10), doi:10.3390/ijerph15102063.
Molina, O. and V. Saldarriaga, 2017: The perils of climate change: In utero exposure to temperature variability and birth outcomes in the Andean region. Econ. Hum. Biol. , 24, 111–124.
Monaghan, A., et al., 2018: The potential impacts of 21st century climatic and population changes on human exposure to the virus vector mosquito Aedes aegypti. Clim. Change, 146 (3), 487–500, doi:10.1007/s10584-016-1679-0.
Monaghan, A.J., et al., 2015: Climate change influences on the annual onset of Lyme disease in the United States. Ticks Tick Borne Dis. , 6 (5), 615–622, doi:10.1016/j.ttbdis.2015.05.005.
Monaghesh, E. and A. Hajizadeh, 2020: The role of telehealth during COVID-19 outbreak: a systematic review based on current evidence. BMC Public Health, 20 (1), doi:10.1186/s12889-020-09301-4.
Monchatre-Leroy, E., et al., 2017: Spatial and temporal epidemiology of nephropathia epidemica incidence and hantavirus seroprevalence in rodent hosts: identification of the main environmental factors in Europe. Transbound. Emerg. Dis. , 64 (4), 1210–1228, doi:10.1111/tbed.12494.
Moore, F.C., N. Obradovich, F. Lehner and P. Baylis, 2019: Rapidly declining remarkability of temperature anomalies may obscure public perception of climate change. Proc. Natl. Acad. Sci. , 116 (11), 4905–4910.
Moore, S., et al., 2018: Dynamics of cholera epidemics from Benin to Mauritania. PLoS Negl. Trop. Dis. , 12 (4), e6379, doi:10.1371/journal.pntd.0006379.
Moore, S.M., et al., 2017: El Niño and the shifting geography of cholera in Africa. Proc. Natl. Acad. Sci. U. S. A. , 114 (17), 4436–4441, doi:10.1073/pnas.1617218114.
Mora, C., C.W.Counsell, C.R. Bielecki and L.V. Louis, 2017a: Twenty-seven ways a heat wave can kill you: Deadly Heat in the Era of Climate Change. Circ. Cardiovasc. Qual. Outcomes, 10 (11), e4233, doi:10.1161/circoutcomes.117.004233.
Mora, C., et al., 2017b: Global risk of deadly heat. Nat. Clim. Change, 7 (7), 501, doi:10.1038/nclimate3322.
Morabito, M., et al., 2021: Heat-related productivity loss: benefits derived by working in the shade or work-time shifting. Int. J. Prod. Perform. Manag. , 70 (3), 507–525, doi:10.1108/ijppm-10-2019-0500.
Morefield, P.E., et al., 2018: Heat-related health impacts under scenarios of climate and population change. Int. J. Environ. Res. Public Health, 15 (11), doi:10.3390/ijerph15112438.
Morens, D.M. and A.S. Fauci, 2014: Chikungunya at the door – deja vu all over again?N. Engl. J. Med. , 371 (10), 885–887, doi:10.1056/NEJMp1408509.
Moretti, A., M. Pascale and A. F. Logrieco, 2019: Mycotoxin risks under a climate change scenario in Europe. Trends Food Sci. Technol. , 84, 38–40, doi:10.1016/j.tifs.2018.03.008.
Morgan, A., A. Ross and N. Reavley, 2018: Systematic review and meta-analysis of mental health first aid training: effects on knowledge, stigma, and helping behaviour. PLoS ONE, 13 (5), doi:10.1371/journal.pone.0197102.
Morin, C., et al., 2018: Unexplored opportunities: use of climate- and weather-driven early warning systems to reduce the burden of infectious diseases. Curr. Environ. Health Rep. , 5 (4), 430–438, doi:10.1007/s40572-018-0221-0.
Morris, N.B., et al., 2020: Sustainable solutions to mitigate occupational heat strain – an umbrella review of physiological effects and global health perspectives. Environ. Health, 19 (1), doi:10.1186/s12940-020-00641-7.
Morton, S., D. Pencheon and G. Bickler, 2019: The sustainable development goals provide an important framework for addressing dangerous climate change and achieving wider public health benefits. Public Health, 174, 65–68, doi:10.1016/j.puhe.2019.05.018.
Mosello, B., C. König, A. Day and C. Nagarajan, 2021: Addressing Climate-related security Risks: Towards a Programme for Action. adelphi, Berlin.
Moss, R.H., P.M. Reed, A. Hadjimichael and J. Rozenberg, 2021: Planned relocation: pluralistic and integrated science and governance. Science, 372 (6548), 1276–1279. Available at: http://science.sciencemag.org/content/372/6548/1276.abstrac.
Mosuela, C., et al., 2015: The Role of A Priori Cross-Border Migration after Extreme Climate Events: The Case of the Philippines after Typhoon Haiyan. In: Environmental Change, Adaptation and Migration: Bringing in the Region, Palgrave Macmillan, London. pp. 98–116.
Mousavi, A., et al., 2020: Climate change and health in Iran: a narrative review. J. Environ. Health Sci. Eng. , 18 (1), 367–378, doi:10.1007/s40201-020-00462-3.
Mpandeli, S., et al., 2018: Climate change adaptation through the water-energy-food nexus in Southern Africa. Int. J. Environ. Res. Public Health, 15 (10), doi:10.3390/ijerph15102306.
Mt. Pleasant, J., 2016: Food yields and nutrient analyses of the three sisters: a Haudenosaunee cropping system. Ethnobiol. Lett. , 7 (1), 87-98.
Muehe, E., et al., 2019: Rice production threatened by coupled stresses of climate and soil arsenic. Nat. Commun. , 10, doi:10.1038/s41467-019-12946-4.
Mueller, V., G. Sheriff, X. Dou and C. Gray, 2020: Temporary migration and climate variation in eastern Africa. World Dev. , 126, 104704. Available at: http://www.sciencedirect.com/science/article/pii/S0305750X19303523.
Mugambiwa, S., 2018: Adaptation measures to sustain indigenous practices and the use of indigenous knowledge systems to adapt to climate change in Mutoko rural district of Zimbabwe. Jamba J. Disaster Risk Stud. , 10, doi:10.4102/jamba.v10i1.388.
Mukeka, J., J. Ogutu, E. Kanga and E. Roskaft, 2019: Human-wildlife conflicts and their correlates in Narok County, Kenya. Glob. Ecol. Conserv. , 18, doi:10.1016/j.gecco.2019.e00620.
Mukherjee, A., S. Babu and S. Ghosh, 2020: Thinking about water and air to attain sustainable development goals during times of COVID-19 pandemic. J. Earth Syst. Sci. , 129 (1), doi:10.1007/s12040-020-01475-0.
Mullins, J. and C. White, 2019: Temperature and mental health: evidence from the spectrum of mental health outcomes. J. Health Econ. , 68, doi:10.1016/j.jhealeco.2019.102240.
Murdock, C.C., E.D. Sternberg and M.B. Thomas, 2016: Malaria transmission potential could be reduced with current and future climate change. Sci. Rep. , 6, 27771, doi:10.1038/srep27771.
Murphy, H.M., K.D. Pintar, E.A. McBean and M.K. Thomas, 2014: A systematic review of waterborne disease burden methodologies from developed countries. J. Water Health, 12 (4), 634–655, doi:10.2166/wh.2014.049.
Murray-Tortarolo, G.N. and S.M. Martnez, 2021: Drought as a driver of Mexico-US migration. Clim. Change, 164 (3), 48, doi:10.1007/s10584-021-03030-2.
Murray, C.J.L., et al., 2020: Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet , 396 (10258), 1223–1249.
Murthy, B.P., et al., 2017: Progress in public health emergency preparedness—United States, 2001–2016. Am. J. Public Health, 107 (S2), S180–S185, doi:10.2105/ajph.2017.304038.
Musacchio, A., et al., 2021: Planning for the health impacts of climate change: flooding, private groundwater contamination and waterborne infection – a cross-sectional study of risk perception, experience and behaviours in the Republic of Ireland. Environ. Res. , 194, 110707, doi:10.1016/j.envres.2021.110707.
Mutheneni, S.R., A.P. Morse, C. Caminade and S.M. Upadhyayula, 2017: Dengue burden in India: recent trends and importance of climatic parameters. Emerg. Microbes Infect. , 6 (8), e70, doi:10.1038/emi.2017.57.
Mutono, N., et al., 2020: The nexus between improved water supply and water-borne diseases in urban areas in Africa: a scoping review protocol. AAS Open Res. , 3, 12, doi:10.12688/aasopenres.13063.2.
Mutono, N., et al., 2021: The nexus between improved water supply and water-borne diseases in urban areas in Africa: a scoping review. AAS Open Res, 4, 27, doi:10.12688/aasopenres.13225.1.
Muyambo, F., A. Jordaan and Y. Bahta, 2017: Assessing social vulnerability to drought in South Africa: policy implication for drought risk reduction. Jamba J. Disaster Risk Stud. , 9 (1), doi:10.4102/jamba.v9i1.326.
Mweya, C., et al., 2016: Climate change influences potential distribution of infected Aedes aegypti co-occurrence with dengue epidemics risk areas in Tanzania. PLoS ONE, 11 (9), doi:10.1371/journal.pone.0162649.
Mygind, L., et al., 2019: Immersive nature-experiences as health promotion interventions for healthy, vulnerable, and sick populations? A systematic review and appraisal of controlled studies. Front. Psychol. , 10, 943–943, doi:10.3389/fpsyg.2019.00943.
Myrttinen, H., L. Khattab and C. Maydaa, 2017: Trust no one, beware of everyone. In: A Gendered Approach to the Syrian Refugee Crisis. Routledge, Abingdon, Oxon; New York, NY, pp. 61–76.
Myrttinen, H., J. Naujoks and J. Schilling, 2015: Gender, natural resources, and peacebuilding in Kenya and Nepal. Peace Rev. , 27 (2), 181–187, doi:10.1080/10402659.2015.1037623.
Na, M., et al., 2020: Food insecurity and cognitive function in middle to older adulthood: a systematic review. Adv. Nutr. , 11 (3), 667–676, doi:10.1093/advances/nmz122.
Nagarajan, C., et al., 2018: Climate Fragility Profile: Lake Chad Basilisks. Adelphi, Berlin.
Nagy, G.J., et al., 2018: An assessment of the relationships between extreme weather events, vulnerability, and the impacts on human wellbeing in Latin America. Int. J. Environ. Res. Public Health, 15, 1802.
Nah, K., A. Bede-Fazekas, A. Trajer and J. Wu, 2020: The potential impact of climate change on the transmission risk of tick-borne encephalitis in Hungary. BMC Infect Dis. , 20 (1), doi:10.1186/s12879-019-4734-4.
Nahian, M. A., , et al., 2018: Drinking water salinity associated health crisis in coastal Bangladesh. Elem. Sci. Anthropocene, 6.DOI: https://doi.org/10.1525/elementa.143
Naik, V., S. Szopa, B. Adhikary, P. Artaxo, T. Berntsen, W.D. Collins, S. Fuzzi, L. Gallardo, A. Kiendler Scharr, Z. Klimont, H. Liao, N. Unger and P. Zanis, 2021: Short-Lived Climate Forcers. In: Climate Change 2021: The Physical Science Basis. Contribution of Working Group I to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change. [Masson-Delmotte, V., P. Zhai, A. Pirani, S. L. Connors, C. Péan, S. Berger, N. Caud, Y. Chen, L. Goldfarb, M. I. Gomis, M. Huang, K. Leitzell, E. Lonnoy, J. B. R. Matthews, T. K. Maycock, T. Waterfield, O. Yelekçi, R. Yu and B. Zhou (eds.)]. Cambridge University Press, Cambridge..
Nasir, S., et al., 2017: Effect of climatic conditions and water bodies on population dynamics of the dengue vector, Aedes aegypti (diptera: culicidae). J. Arthropod Borne Dis. , 11 (1), 50–59.
Natarajan, N., K. Brickell and L. Parsons, 2019: Climate change adaptation and precarity across the rural–urban divide in Cambodia: towards a ‘climate precarity’ approach. Environ. Plan. E Nat. Space, 2 (4), 899–921.
Nawrotzki, R. and J. DeWaard, 2018: Putting trapped populations into place: climate change and inter-district migration flows in Zambia. Reg. Environ. Change, 18 (2), 533–546, doi:10.1007/s10113-017-1224-3.
Nawrotzki, R.J. and M. Bakhtsiyarava, 2017: International climate migration: evidence for the climate inhibitor mechanism and the agricultural pathway. Popul. Space Place, 23 (4), e2033–e2033.
Nawrotzki, R.J., J. DeWaard, M. Bakhtsiyarava and J.T. Ha, 2017: Climate shocks and rural-urban migration in Mexico: exploring nonlinearities and thresholds. Clim. Change, 140 (2), 243–258, doi:10.1007/s10584-016-1849-0.
Neef, A., et al., 2018: Climate adaptation strategies in Fiji: the role of social norms and cultural values. World Dev. , 107, 125–137, doi:10.1016/j.worlddev.2018.02.029.
Nelson, M., et al., 2016: Alignment of healthy dietary patterns and environmental sustainability: a systematic review. Adv. Nutr. , 7 (6), 1005–1025, doi:10.3945/an.116.012567.
Neufeld, H.T., C. Richmond and Southwest Ontario Aboriginal Health Access Centre, , 2020: Exploring first nation elder women’s relationships with food from social, ecological, and historical perspectives. Curr. Dev. Nutr. , 4 (3), nzaa11, doi:10.1093/cdn/nzaa011.
Neumann, B., A.T. Vafeidis, J. Zimmermann and R.J. Nicholls, 2015: Future coastal population growth and exposure to sea-level rise and coastal flooding – a global assessment. PLoS ONE, 10 (6), e131375–e131375.
Neumann, J.E., et al., 2019: Estimates of present and future asthma emergency department visits associated with exposure to oak, birch, and grass pollen in the United States. GeoHealth, 3 (1), 11–27, doi:10.1029/2018gh000153.
Neumann, K. and F. Hermans, 2015: What drives human migration in Sahelian countries? A meta-analysis. Popul. Space Place, doi:10.1002/psp.1962.
Newnham, E., N. Titov and P. McEvoy, 2020: Preparing mental health systems for climate crisis. Lancet Planet. Health, 4 (3), E89–E90.
Ng, K.Y.Y., et al., 2021: Factors influencing protective behaviours during haze episodes in Singapore: a population-based study. Ann. Acad. Med. Singap. , 50 (7), 514–526, doi:10.47102/annals-acadmedsg.2020614.
Ngigi, M., U. Mueller and R. Birner, 2017: Gender differences in climate change adaptation strategies and participation in group-based approaches: an intra-household analysis from rural Kenya. Ecol. Econ. , 138, 99–108, doi:10.1016/j.ecolecon.2017.03.019.
Ngo, C., P. Poortvliet and P. Feindt, 2020: Drivers of flood and climate change risk perceptions and intention to adapt: an explorative survey in coastal and delta Vietnam. J. Risk Res. , 23 (4), 424–446, doi:10.1080/13669877.2019.1591484.
Ngo, N.S. and R.M. Horton, 2016: Climate change and fetal health: the impacts of exposure to extreme temperatures in New York City. Environ. Res. , 144 (Pt A), 158–164, doi:10.1016/j.envres.2015.11.016.
Nguyen, H., 2019: Gendered vulnerabilities in times of natural disasters: male-to-female violence in the Philippines in the aftermath of super Typhoon Haiyan. Violence Against Women, 25 (4), 421–440, doi:10.1177/1077801218790701.
Nhamo, G. and S. Muchuru, 2019: Climate adaptation in the public health sector in Africa: evidence from United Nations framework convention on climate change national communications. Jamba J. Disaster Risk Stud. , 11, doi:10.4102/jamba.v11i1.644.
Nicholls, R.J., et al., 2021: A global analysis of subsidence, relative sea-level change and coastal flood exposure. Nat. Clim. Change, 11 (4), 338–342, doi:10.1038/s41558-021-00993-z.
Nicholls, R.J., et al., 2007: Ranking of the World’s Cities Most Exposed to Coastal Flooding Today and in the Future. Organisation for Economic Co-operation and Development (OECD), Paris.
Nichols, A., 2019: Climate change, natural hazards, and relocation: insights from Nabukadra and Navuniivi villages in Fiji. Clim. Change, 156 (1), 255–271, doi:10.1007/s10584-019-02531-5.
Nichols, G., I. Lake and C. Heaviside, 2018: Climate change and water-related infectious diseases. Atmosphere, 9 (10), doi:10.3390/atmos9100385.
Nightingale, A., 2017: Power and politics in climate change adaptation efforts: struggles over authority and recognition in the context of political instability. Geoforum, 84, 11–20.
Niles, M., et al., 2021: Climate impacts associated with reduced diet diversity in children across nineteen countries. Environ. Res. Lett. , 16 (1), doi:10.1088/1748-9326/abd0ab.
Nilsson, L., et al., 2011: Diet and lifestyle of the Sami of southern Lapland in the 1930s–1950s and today. Int. J. Circumpolar Health, 70 (3), 301–318, doi:10.3402/ijch.v70i3.17831.
Nitschke, M., et al., 2016: Evaluation of a heat warning system in Adelaide, South Australia, using case-series analysis. BMJ Open, 6 (7), doi:10.1136/bmjopen-2016-012125.
Nkumama, I.N., W.P. O’Meara and F.H.A. Osier, 2017: Changes in malaria epidemiology in Africa and new challenges for elimination. Trends Parasitol. , 33 (2), 128–140, doi:10.1016/j.pt.2016.11.006.
Noelke, C., et al., 2016: Increasing ambient temperature reduces emotional well-being. Environ. Res. , 151, 124–129, doi:10.1016/j.envres.2016.06.045.
Nordqvist, P. and F. Krampe, 2018: Climate Change and Violent Conflict: Sparse Evidence from South Asia and South East Asia. International Peace Research Institute, Stockholm.
Norton-Smith, K., et al., 2016: Climate Change and Indigenous Peoples: a Synthesis of Current Impacts and Experiences. US Department of Agriculture, Forest Service, Pacific Northwest Research Station, Portland.
Nurse, K., 2019: Migration, diasporas, remittances and the sustainable development goals in least developed countries. J. Glob. Dev. , 9 (2), 20190006.
Nursey-Bray, M., 2017: Towards socially just adaptive climate governance: the transformative potential of conflict. Local Environ, 22 (2), 156–171, doi:10.1080/13549839.2016.1181618.
Nursey-Bray, M. and R. Palmer, 2018: Country, climate change adaptation and colonisation: insights from an Indigenous adaptation planning process, Australia. Heliyon, 4 (3), e565, doi:10.1016/j.heliyon.2018.e00565.
Nursey-Bray, M., et al., 2020: Scale, colonisation and adapting to climate change: insights from the Arabana people, South Australia. Geoforum, 114, 138–150, doi:10.1016/j.geoforum.2020.05.021.
O’Neill, D., A. Fanning, W. Lamb and J. Steinberger, 2018: A good life for all within planetary boundaries. Nat. Sustain. , 1 (2), 88–95, doi:10.1038/s41893-018-0021-4.
O’Donnell, R., M. Savaglio, D. Vicary and H. Skouteris, 2021: Effect of community mental health care programs in Australia: a systematic review. Aust. J. Prim. Health, 26 (6), 443–451.
Oakes, R., 2019: Culture, climate change and mobility decisions in Pacific Small Island Developing States. Popul. Environ. , 40 (4), 480–503, doi:10.1007/s11111-019-00321-w.
Obaidat, M.M. and A.A. Roess, 2018: First report on seroprevalence and risk factors of dengue virus in Jordan. Trans. R. Soc. Trop. Med. Hyg. , 112 (6), 279–284, doi:10.1093/trstmh/try055.
Obokata, R. and L. Veronis, 2018: Transnational approaches to remittances, risk reduction, and disaster relief: evidence from post-Typhoon Haiyan experiences of Filipino immigrants in Canada. In Routledge handbook of environmental displacement and migration. [McLeman, R. and F. Gemenne(eds.)]. Routledge, London.
Obradovich, N. and J.H. Fowler, 2017: Climate change may alter human physical activity patterns. Nat. Hum. Behav. , 1, 97, doi:10.1038/s41562-017-0097. https://www.nature.com/articles/s41562-017-0097#supplementary-information.
Obradovich, N. and R. Migliorini, 2018: Sleep and the human impacts of climate change. Sleep Med. Rev. , 42, 1–2, doi:10.1016/j.smrv.2018.09.002.
Obradovich, N., R. Migliorini, S.C. Mednick and J.H. Fowler, 2017: Nighttime temperature and human sleep loss in a changing climate. Sci. Adv. , 3 (5), e1601555–e1601555, doi:10.1126/sciadv.1601555.
Obradovich, N., R. Migliorini, M.P. Paulus and I. Rahwan, 2018: Empirical evidence of mental health risks posed by climate change. Proc. Natl. Acad. Sci. U.S.A. , 115 (43), 10953–10958, doi:10.1073/pnas.1801528115.
Obradovich, N. and I. Rahwan, 2019: Risk of a feedback loop between climatic warming and human mobility. J. R. Soc. Interface.16, DOI: 2019005820190058
Ocello, C., A. Petrucci, M.R. Testa and D. Vignoli, 2015: Environmental aspects of internal migration in Tanzania. Popul. Environ. , 37 (1), 99–108.
Ogunbode, C., et al., 2021: Negative emotions about climate change are related to insomnia symptoms and mental health: cross-sectional evidence from 25 countries. Curr. Psychol. , doi:10.1007/s12144-021-01385-4.
Ogunbode, C.A., C. Demski, S.B. Capstick and R.G. Sposato, 2019: Attribution matters: revisiting the link between extreme weather experience and climate change mitigation responses. Glob. Environ. Change, 54, 31–39.
Okpara, U.T., L.C. Stringer and A.J. Dougill, 2016: Perspectives on contextual vulnerability in discourses of climate conflict. Earth Syst. Dyn. , 7 (1), 89–102, doi:10.5194/esd-7-89-2016.
Okpara, U.T., L.C. Stringer and A.J. Dougill, 2018: Integrating climate adaptation, water governance and conflict management policies in lake riparian zones: insights from African drylands. Environ. Sci. Policy, 79, 36–44.
Olson, D.M. and G.A.S. Metz, 2020: Climate change is a major stressor causing poor pregnancy outcomes and child development. F1000Res, 9, doi:10.12688/f1000research.27157.1.
Oluwole, O.S.A., 2015: Seasonal influenza epidemics and El Ninos. Front. Public Health, 3, doi:10.3389/fpubh.2015.00250.
Oluwole, O.S.A., 2017: Dynamic regimes of El Nino southern oscillation and influenza pandemic timing. Front. Public Health, 5, doi:10.3389/fpubh.2017.00301.
Onozuka, D. and A. Hagihara, 2015: Non-stationary dynamics of climate variability in synchronous influenza epidemics in Japan. Int. J. Biometeorol. , 59 (9), 1253–1259, doi:10.1007/s00484-014-0936-z.
Opondo, M., U. Abdi and P. Nangiro, 2016: Assessing Gender in Resilience Programming: Uganda. BRACED, Overseas Development Institute, London. 16 pp.
Oppermann, E., et al., 2021: Establishing intensifying chronic exposure to extreme heat as a slow onset event with implications for health, wellbeing, productivity, society and economy. Curr. Opin. Environ. Sustain. , 50, 225–235, doi:10.1016/j.cosust.2021.04.006.
Orlov, A., et al., 2020: Economic costs of heat-induced reductions in worker productivity due to global warming. Glob. Environ. Change Policy Dimensions, 63, doi:10.1016/j.gloenvcha.2020.102087.
Orru, H., et al., 2019: Ozone and heat-related mortality in Europe in 2050 significantly affected by changes in climate, population and greenhouse gas emission. Environ. Res. Lett. , 14 (7), doi:10.1088/1748-9326/ab1cd9.
Orru, H., K.L. Ebi and B. Forsberg, 2017: The interplay of climate change and air pollution on health. Curr. Environ. Health Rep. , 4 (4), 504–513, doi:10.1007/s40572-017-0168-6.
Orru, K., et al., 2016: Well-being and environmental quality: Does pollution affect life satisfaction?Qual. Life Res. , 25 (3), 699–705, doi:10.1007/s11136-015-1104-6.
Osberghaus, D. and J. Kühling, 2016: Direct and indirect effects of weather experiences on life satisfaction–which role for climate change expectations?J. Environ. Plan. Manag. , 59 (12), 2198–2230.
Ostergard, J.R.L. and N. Seltzer, 2020: Climate change and global health security: an overview of the scope and issues. Glob. Health Gov. , X (1) 5–23.
Ostro, B., et al., 2010: The effects of temperature and use of air conditioning on hospitalizations. Am. J. Epidemiol. , 172 (9), 1053–1061, doi:10.1093/aje/kwq231.
Ottenhoff, L., 2021: Indigenous conservation can get Canada to climate goals: former MP Ethel Blondin-Andrew to Trudeau. National Observer, 25 January 2021. https://www.nationalobserver.com/2021/01/25/news/climate-change-indigenous-knowledge-ethel-blondin-andrew. Last accessed 3 September 2021.
Otto, F.E.L., et al., 2020: Challenges to understanding extreme weather changes in lower income countries. Bull. Am. Meteorol. Soc. , 101 (10), E1851–E1860, doi:10.1175/bams-d-19-0317.1.
Otto, I.M., et al., 2017: Social vulnerability to climate change: a review of concepts and evidence. Reg. Environ. Change, 17 (6), 1651–1662.
Ouattara, B. and E. Strobl, 2014: Hurricane strikes and local migration in US coastal counties. Econ. Lett. , 124 (1), 17–20.
Owain, E.L. and M. A. Maslin, 2018: Assessing the relative contribution of economic, political and environmental factors on past conflict and the displacement of people in East Africa. Palgrave Commun. , 4, doi:10.1057/s41599-018-0096-6.
Owen, J.P., B. Baig, C. Abbo and Y. Baheretibeb, 2016: Child and adolescent mental health in sub-Saharan Africa: a perspective from clinicians and researchers. BJPsych Int. , 13, 45–47, doi:10.1192/s2056474000001136.
Paavola, J., 2017: Health impacts of climate change and health and social inequalities in the UK. Environ. Health, 16 (Suppl 1), 113, doi:10.1186/s12940-017-0328-z.
Paerl, H.W., et al., 2016: Mitigating cyanobacterial harmful algal blooms in aquatic ecosystems impacted by climate change and anthropogenic nutrients. Harmful Algae, 54, 213–222, doi:10.1016/j.hal.2015.09.009.
Paffenholz, T., 2018: Women in peace negotiations. In: Gendering Diplomacy and International Negotiation. Springer, Dordrecht, pp. 169–191.
Pai, N., 2008: Climate Change and National Security: Preparing India for New Conflict Scenarios. Indian National Interest Policy Brief, Vol. 1. Takshashila Institution, Bangalore.
Pal, J.S. and E.A.B. Eltahir, 2016: Future temperature in southwest Asia projected to exceed a threshold for human adaptability. Nat. Clim. Change, 6 (2), 197–200, doi:10.1038/nclimate2833.
Papadakis, G., Z. Chalabi and J.E. Thornes, 2018: Ambulance Service Resource Planning for Extreme Temperatures: Analysis of Ambulance 999 Calls during Episodes of Extreme Temperature in London, UK. Atmosphere, 9 (5), doi:10.3390/atmos9050182.
Park, C., et al., 2019: The global effect of extreme weather events on nutrient supply: a superposed epoch analysis. Lancet Planet. Health, 3, e429–e438, doi:10.1016/s2542-5196(19)30193-7.
Park, J., et al., 2020: Association between short-term air pollution exposure and attention-deficit/hyperactivity disorder-related hospital admissions among adolescents: a nationwide time-series study. Environ. Pollut. , 266 (Pt 1), 115369, doi:10.1016/j.envpol.2020.115369.
Park, M., K. Park and G. Bahk, 2018a: Combined influence of multiple climatic factors on the incidence of bacterial foodborne diseases. Sci. Total Environ. , 610, 10–16, doi:10.1016/j.scitotenv.2017.08.045.
Park, M.S., K.H. Park and G.J. Bahk, 2018b: Combined influence of multiple climatic factors on the incidence of bacterial foodborne diseases. Sci. Total Environ. , 610-611, 10–16, doi:10.1016/j.scitotenv.2017.08.045.
Park, M.S., K.H. Park and G.J. Bahk, 2018c: Interrelationships between multiple climatic factors and incidence of foodborne diseases. Int. J. Environ. Res. Public Health, 15 (11), doi:10.3390/ijerph15112482.
Park, R.J., A.P. Behrer and J. Goodman, 2021: Learning is inhibited by heat exposure, both internationally and within the United States. Nat. Hum. Behav. , 5 (1), 19–27, doi:10.1038/s41562-020-00959-9.
Parks, R.M., et al., 2020: Anomalously warm temperatures are associated with increased injury deaths. Nat. Med. , 26 (1), 65–70.
Parthemore, C., F. Femia and C. Werrell, 2018: The global responsibility to prepare for intersecting climate and nuclear risks. Bull. At. Sci. , 74 (6), 374–378, doi:10.1080/00963402.2018.1533186.
Pascal, M., et al., 2021: Extreme heat and acute air pollution episodes: a need for joint public health warnings?Atmos. Environ. , 249, doi:10.1016/j.atmosenv.2021.118249.
Pasini, A. and F. Mazzocchi, 2020: Perception and risk of Covid-19 and climate change: investigating analogies in a common framework. Glob. Sustain. , 3, e32, doi:10.1017/sus.2020.30.
Patel, D., et al., 2019: Joint effects of heatwaves and air quality on ambulance services for vulnerable populations in Perth, western Australia. Environ. Pollut. , 252, 532–542, doi:10.1016/j.envpol.2019.05.125.
Patel, P., S. Mondal and K. Ghosh, 2020: Some respite for India’s dirtiest river? Examining the Yamuna’s water quality at Delhi during the COVID-19 lockdown period. Sci. Total Environ. , 744, doi:10.1016/j.scitotenv.2020.140851.
Patterson, K., et al., 2017: Seasonal variation of food security among the Batwa of Kanungu, Uganda. Public Health Nutr. , 20 (1), 1-11.
Paudel, B., et al., 2021: Increased duration of pollen and mold exposure are linked to climate change. Sci. Rep. , 11 (1), 12816–12816, doi:10.1038/s41598-021-92178-z.
Payne, J., D. Weatherall and F. Downy, 2015: Capturing the “multiple benefits” of energy efficiency in practice: the UK example. In: ECEE Summer Study Proc. , pp. 229–238.
Paynter, S., et al., 2010: Childhood pneumonia: a neglected, climate-sensitive disease?Lancet , 376 (9755), 1804–1805, doi:10.1016/s0140-6736(10)62141-1.
Paz, S. and J.C. Semenza, 2016: El Niño and climate change – contributing factors in the dispersal of Zika virus in the Americas?Lancet , 387 (10020), 745, doi:10.1016/s0140-6736(16)00256-7.
Pearse, R., 2017: Gender and climate change. Wiley Interdiscip. Rev. Clim. Change, 8 (2), e451.
Pelling, M., et al., 2021: Synergies between COVID-19 and climate change impacts and responses. J. Extrem. Events. DOI: https://doi.org/10.1142/S2345737621310023
Pelling, M. and K. Dill, 2010: Disaster politics: tipping points for change in the adaptation of sociopolitical regimes. Prog. Hum. Geogr. , 34 (1), 21–37.
Pena-Garcia, V. H., O. Triana-Chavez and S. Arboleda-Sanchez, 2017: Estimating effects of temperature on dengue transmission in Colombian cities. Ann. Glob. Health, 83 (3), 509–518, doi:10.1016/j.aogh.2017.10.011.
Peng, W., J. Yang, X. Lu and D.L. Mauzerall, 2018: Potential co-benefits of electrification for air quality, health, and CO2 mitigation in 2030 China. Appl. Energy, 218, 511–519, doi:10.1016/j.apenergy.2018.02.048.
Peng, W., J. Yang, F. Wagner and L. Mauzerall, 2017: Substantial air quality and climate co-benefits achievable now with sectoral mitigation strategies in China. Sci. Total Environ. , 598, 1076–1084, doi:10.1016/j.scitotenv.2017.03.287.
Perera, F., 2017: Multiple threats to child health from fossil fuel combustion: impacts of air pollution and climate change. Environ. Health Perspect. , 125 (2), 141–148, doi:10.1289/ehp299.
Perevolotsky, A. and E. Sheffer, 2011: Integrated management of heterogenous landscape – Mediterranean Israel as a study case. Isr. J. Ecol. Evol. , 57 (1-2), 111–128.
Peters, D.H., et al., 2019: Financing common goods for health: core government functions in health emergency and disaster risk management. Health Syst. Reform, 5 (4), 307–321, doi:10.1080/23288604.2019.1660104.
Petkova, E.P., A. Gasparrini and P.L. Kinney, 2014: Heat and mortality in New York City since the beginning of the 20th century. Epidemiology, 25 (4), 554–560, doi:10.1097/ede.0000000000000123.
Petrova, D., et al., 2019: Sensitivity of large dengue epidemics in Ecuador to long-lead predictions of El Nino. Clim. Serv. , 15, doi:10.1016/j.cliser.2019.02.003.
Petrova, K., 2021: Natural hazards, internal migration and protests in Bangladesh. J. Peace Res. , 58 (1), 33–49, doi:10.1177/0022343320973741.
Phalkey, R. and V. Louis, 2016: Two hot to handle: How do we manage the simultaneous impacts of climate change and natural disasters on human health?Eur. Phys. J. Special Top. , 225 (3), 443–457, doi:10.1140/epjst/e2016-60071-y.
Phelan, A.L., R. Katz and L.O. Gostin, 2020: The novel coronavirus originating in Wuhan, China challenges for global health governance. J. Am. Med. Assoc. , 323 (8), 709–710, doi:10.1001/jama.2020.1097.
Philipsborn, R., S.M. Ahmed, B.J. Brosi and K. Levy, 2016: Climatic drivers of Diarrheagenic Escherichia coli incidence: a systematic review and meta-analysis. J. Infect. Dis. , 214 (1), 6–15, doi:10.1093/infdis/jiw081.
Phillips, C.A., et al., 2020: Compound climate risks in the COVID-19 pandemic. Nat. Clim. Change, 10, 586–598.
Phung, D., et al., 2017: Heatwave and risk of hospitalization: a multi-province study in Vietnam. Environ. Pollut. , 220, 597–607, doi:10.1016/j.envpol.2016.10.008.
Phung, D., et al., 2015: Climate change, water quality, and water-related diseases in the Mekong Delta Basin: a systematic review. Asia Pac. J. Public Health, 27 (3), 265–276, doi:10.1177/1010539514565448.
Phung, D., et al., 2016: Ambient temperature and risk of cardiovascular hospitalization: an updated systematic review and meta-analysis. Sci. Total Environ. , 550, 1084–1102, doi:10.1016/j.scitotenv.2016.01.154.
Piekałkiewicz, M., 2017: Why do economists study happiness?Econ. Labour Relat. Rev. , 28, 361–377, doi:10.1177/1035304617717130.
Piggott-McKellar, A., K. McNamara, P. Nunn and S. Sekinini, 2019: Moving people in a changing climate: lessons from two case studies in Fiji. Soc. Sci. , 8, 133, doi:10.3390/socsci8050133.
Piguet, E., 2019: Climatic statelessness: risk assessment and policy options. Popul. Dev. Rev. , 45 (4), 865–883, doi:10.1111/padr.12295.
Piguet, E., R. Kaenzig and J. Guélat, 2018: The uneven geography of research on “environmental migration”. Popul. Environ. , 39 (4), 357–383, doi:10.1007/s11111-018-0296-4.
Pineda, C., R. Munoz-Louis, C.V. Caballero-Uribe and D. Viasus, 2016: Chikungunya in the region of the Americas. A challenge for rheumatologists and health care systems. Clin. Rheumatol. , 35 (10), 2381–2385, doi:10.1007/s10067-016-3390-y.
Piper, N., 2017: Migration and the SDGs. Glob. Soc. Policy, 17 (2), 231–238.
Pisello, A.L., et al., 2018: Facing the urban overheating: recent developments. Mitigation potential and sensitivity of the main technologies. Wiley Interdiscip. Rev. Environ. , 7 (4), doi:10.1002/wene.294.
Poch, M., et al., 2020: When the fourth water and digital revolution encountered COVID-19. Sci. Total Environ. , 744, doi:10.1016/j.scitotenv.2020.140980.
Polain, J.D., H.L. Berry and J.O. Hoskin, 2011: Rapid change, climate adversity and the next ‘big dry’: older farmers’ mental health. Aust. J. Rural Health, 19 (5), 239–243, doi:10.1111/j.1440-1584.2011.01219.x.
Pollack, A., B. Weiss and T. Trung, 2016: Mental health, life functioning and risk factors among people exposed to frequent natural disasters and chronic poverty in Vietnam. BJPsych Open, 2 (3), 221–232.
Pollard, G., M. Davies and H. Moore, 2015: Women, marketplaces and exchange partners amongst the Marakwet of northwest Kenya. J. East. Afr. Stud. , 9 (3), 412–439, doi:10.1080/17531055.2015.1089699.
Polyakova, M., G. Kocks, V. Udalova and A. Finkelstein, 2020: Initial economic damage from the COVID-19 pandemic in the United States is more widespread across ages and geographies than initial mortality impacts. Proc. Natl. Acad. Sci. U. S. A. , doi:10.1073/pnas.2014279117.
Ponjoan, A., et al., 2017: Effects of extreme temperatures on cardiovascular emergency hospitalizations in a Mediterranean region: a self-controlled case series study. Environ. Health, 16, doi:10.1186/s12940-017-0238-0.
Poole, J.A., et al., 2019: Impact of weather and climate change with indoor and outdoor air quality in asthmatic patients. Journal of Allergy and Clinical Immunology, 143 (5), 1702-1710
Poore, J. and T. Nemecek, 2018: Reducing food’s environmental impacts through producers and consumers. Science, 360 (6392), 987–992, doi:10.1126/science.aag0216.
Poortinga, W., et al., 2019: Climate change perceptions and their individual-level determinants: a cross-European analysis. Glob. Environ. Change, 55, 25–35.
Popov, I. and V. Yasyukevich, 2014: The taiga tick Ixodes persulcatus: propagation under climate change conditions in the 21st century. Russ. Meteorol. Hydrol. , 39 (8), 558–563, doi:10.3103/s1068373914080081.
Porst, L. and P. Sakdapolrak, 2020: Gendered translocal connectedness: rural–urban migration, remittances, and social resilience in Thailand. Popul. Space Place, 26 (4), e2314, doi:10.1002/psp.2314.
Porter, C. and R. Goyal, 2016: Social protection for all ages? Impacts of Ethiopia’s Productive Safety Net Program on child nutrition. Soc. Sci. Med. , 159, 92–99, doi:10.1016/j.socscimed.2016.05.001.
Portier, C., et al., 2010: A human health perspective on climate change. In: Environmental Health Perspectives. National Institute of Environmental Health Sciences, Research Triangle Park, NC.
Pottie, K., et al., 2015: Access to healthcare for the most vulnerable migrants: a humanitarian crisis. Confl. Health, 9, doi:10.1186/s13031-015-0043-8.
Power, M., S. Adar, J. Yanosky and J. Weuve, 2016: Exposure to air pollution as a potential contributor to cognitive function, cognitive decline, brain imaging, and dementia: a systematic review of epidemiologic research. Neurotoxicology, 56, 235–253, doi:10.1016/j.neuro.2016.06.004.
Pozza, L.E. and D.J. Field, 2020: The science of soil security and food security. Soil Security, DOI: https://doi.org/10.1016/j.soisec.2020.100002
Pramanik, M., et al., 2020: El Nino Southern Oscillation as an early warning tool for dengue outbreak in India. BMC Public Health, 20 (1), doi:10.1186/s12889-020-09609-1.
Pretty, J. and J. Barton, 2020: Nature-based interventions and mind-body interventions: saving public health costs whilst increasing life satisfaction and happiness. Int. J. Environ. Res. Public Health, 17 (21), doi:10.3390/ijerph17217769.
Price, D., K.M. Hughes, F. Thien and C. Suphioglu, 2021: Epidemic thunderstorm asthma: lessons learned from the storm down-under. J. Allergy Clin. Immunol. Pract. , 9 (4), 1510–1515, doi:10.1016/j.jaip.2020.10.022.
Proestos, Y., et al., 2015: Present and future projections of habitat suitability of the Asian tiger mosquito, a vector of viral pathogens, from global climate simulation. Philos. Trans. Royal Soc. B, 370 (1678), doi:10.1098/rstb.2015.0246.
Prueksapanich, P., et al., 2018: Liver fluke-associated biliary tract cancer. Gut Liver, 12 (3), 236–245, doi:10.5009/gnl17102.
Psarros, C., et al., 2017: Insomnia and PTSD one month after wildfires: evidence for an independent role of the “fear of imminent death”. Int. J. Psychiat. Clin. , 21 (2), 137–141, doi:10.1080/13651501.2016.1276192.
Pu, X., et al., 2017: Enhanced surface ozone during the heat wave of 2013 in Yangtze River Delta region, China. Sci. Total Environ. , 603, 807–816, doi:10.1016/j.scitotenv.2017.03.056.
Pyrgou, A., P. Hadjinicolaou and M. Santamouris, 2018: Enhanced near-surface ozone under heatwave conditions in a Mediterranean island. Sci. Rep. , 8, doi:10.1038/s41598-018-27590-z.
Qiu, H., et al., 2016: Pneumonia hospitalization risk in the elderly attributable to cold and hot temperatures in Hong Kong, China. Am. J. Epidemiol. , 184 (8), 570–578, doi:10.1093/aje/kww041.
Qu, J., 2016: Is sunspot activity a factor in influenza pandemics?Rev. Med. Virol. , 26 (5), 309–313, doi:10.1002/rmv.1887.
Quast, T. and L. Feng, 2019: Long-term effects of disasters on health care utilization: Hurricane Katrina and older individuals with diabetes. Disaster Med. Public Health Prep. , 1–8, doi:10.1017/dmp.2018.128.
Quintero-Herrera, L.L., et al., 2015: Potential impact of climatic variability on the epidemiology of dengue in Risaralda, Colombia, 2010–2011. J. Infect. Public Health, 8 (3), 291–297, doi:10.1016/j.jiph.2014.11.005.
Ragettli, M.S. and M. Roosli, 2019: Heat-health action plans to prevent heat-related deaths-experiences from Switzerland. Bundesgesundheitsbl. Gesundheitsforsch. Gesundheitsschutz, 62 (5), 605–611, doi:10.1007/s00103-019-02928-8.
Raghavan, S.V., et al., 2019: ASEAN food security under the 2°C-4°C global warming climate change scenarios. In: Disasters, Climate Change, and Food Security: Supporting ASEAN Resilience[Anbum Ozhi, V., M.B. Reiling and V. Reddy(eds.)], Towards a Resilient ASEAN, Vol. 1, Economic Research Institute for ASEAN and East Asia, Jakarta.
Rahman, S., et al., 2019: Projected changes of inundation of cyclonic storms in the Ganges–Brahmaputra–Meghna delta of Bangladesh due to SLR by 2100. J. Earth Syst. Sci. , doi:10.1007/s12040-019-1184-8.
Rail, M., et al., 2019: Impact of climate and population change on temperature-related mortality burden in Bavaria, Germany. Environ. Res. Lett. , 14 (12), doi:10.1088/1748-9326/ab5ca6.
Rakotoarison, N., et al., 2018: Assessment of risk, vulnerability and adaptation to climate change by the health sector in Madagascar. Int. J. Environ. Res. Public Health, 15 (12), doi:10.3390/ijerph15122643.
Ramamurthy, P. and E. Bou-Zeid, 2017: Heatwaves and urban heat islands: a comparative analysis of multiple cities. J. Geophys. Res. , 122 (1), 168–178, doi:10.1002/2016jd025357.
Ramesh, A., et al., 2016: The impact of climate on the abundance of Musca sorbens, the vector of trachoma. Parasit Vectors, 9, 48, doi:10.1186/s13071-016-1330-y.
Ramos-Castillo, A., E. Castellanos and K. McLean, 2017: Indigenous peoples, local communities and climate change mitigation. Clim. Change, 140 (1), 1–4, doi:10.1007/s10584-016-1873-0.
Ramos, A.K., et al., 2020: Invisible no more: the impact of COVID-19 on essential food production workers. J. Agromed. , 25, 378–382.
Rankoana, S.A., 2021: Climate change impacts on indigenous health promotion: the case study of Dikgale community in Limpopo Province, South Africa. Glob. Health Promot. , doi:10.1177/17579759211015183.
Ranson, M., 2014: Crime, weather, and climate change. J. Environ. Econ. Manag. , 67 (3), 274–302, doi:10.1016/j.jeem.2013.11.008.
Rao, K.K., et al., 2020: Projections of heat stress and associated work performance over India in response to global warming. Sci. Rep. , 10 (1), doi:10.1038/s41598-020-73245-3.
Rao, M.R.K., R.N. Padhy and M.K. Das, 2018: Episodes of the epidemiological factors correlated with prevailing viral infections with dengue virus and molecular characterization of serotype-specific dengue virus circulation in eastern India. Infect. Genet. Evol. , 58, 40–49, doi:10.1016/j.meegid.2017.12.005.
Rao, N., 2019: From abandonment to autonomy: gendered strategies for coping with climate change, Isiolo County, Kenya. Geoforum, 102, 27–37, doi:10.1016/j.geoforum.2019.03.017.
Rao, N., et al., 2019a: Gendered vulnerabilities to climate change: insights from the semi-arid regions of Africa and Asia. Clim. Dev. , 11 (1), 14–26.
Rao, N., et al., 2019b: Managing risk, changing aspirations and household dynamics: implications from wellbeing and adaptation in semi-arid Africa and India. World Dev. , doi:10.1016/j.worlddev.2019.104667.
Rataj, E., K. Kunzweiler and S. Garthus-Niegel, 2016: Extreme weather events in developing countries and related injuries and mental health disorders – a systematic review. BMC Public Health, 16 (1), 1020, doi:10.1186/s12889-016-3692-7.
Ravera, F., B. Martin-Lopez, U. Pascual and A. Drucker, 2016: The diversity of gendered adaptation strategies to climate change of Indian farmers: a feminist intersectional approach. Ambio, 45, 335–351, doi:10.1007/s13280-016-0833-2.
Raymond, C., T. Matthews and R.M. Horton, 2020: The emergence of heat and humidity too severe for human tolerance. Sci. Adv. , 6 (19), doi:10.1126/sciadv.aaw1838.
Reckien, D., 2021: What can local climate planning learn from COVID-19? Transform the city – it saves the climate and lowers the risk of pandemics. Plan. Theory Pract. , doi:10.1080/14649357.2021.1951578.
Regli, S., et al., 2015: Estimating potential increased bladder cancer risk due to increased bromide concentrations in sources of disinfected drinking waters. Environ. Sci. Technol. , 49 (22), 13094–13102, doi:10.1021/acs.est.5b03547.
Reid, C.E., et al., 2016: Critical review of health impacts of wildfire smoke exposure. Environ. Health Perspect. , 124 (9), 1334–1343, doi:10.1289/ehp.1409277.
Reid, P., D. Cormack and S.J. Paine, 2019: Colonial histories, racism and health – the experience of Māori and indigenous peoples. Public Health, 172, 119–124, doi:10.1080/10705422.2019.1658677.
Remling, E., 2020: Migration as climate adaptation? Exploring discourses amongst development actors in the Pacific Island region. Reg. Environ. Change, 20 (1), 3, doi:10.1007/s10113-020-01583-z.
Reser, J.P., et al., 2012: Public Risk Perceptions, Understandings, and Responses to Climate Change and Natural Disasters in Australia, 2010 and 2011. National Climate Change Adaptation Research Facility, Gold Coast. 245 pp.
Reyer, C.P., et al., 2017: Climate change impacts in Central Asia and their implications for development. Reg. Environ. Change, 17 (6), 1639–1650.
Reyes, M.E.S., et al., 2021: An investigation into the relationship between climate change anxiety and mental health among Gen Z Filipinos. Curr. Psychol. , 1–9, doi:10.1007/s12144-021-02099-3.
Rice, M.B., G.D. Thurston, J.R. Balmes and K.E. Pinkerton, 2014: Climate change. A global threat to cardiopulmonary health. Am. J. Respir. Crit. Care Med. , 189 (5), 512–519, doi:10.1164/rccm.201310-1924PP.
Richmond, C.A.M. and N.A. Ross, 2009: The determinants of First Nation and Inuit health: a critical population health approach. Health Place, 15 (2), 403–411, doi:10.1016/j.healthplace.2008.07.004.
Rickerts, V., 2019: Climate change and systemic fungal infections. Bundesgesundheitsbl. Gesundheitsforsch. Gesundheitsschutz, 62 (5), 646–651, doi:10.1007/s00103-019-02931-z.
Rigaud, K.K., et al., 2018: Groundswell: Preparing for Internal Climate Migration. Washington DC, https://openknowledge.worldbank.org/handle/10986/29461. Last accessed 3 September 2021.
Rigg, J., T. Nguyen, T. Thu and H. Luong, 2018: The texture of livelihoods: migration and making a living in Hanoi. J. Dev. Stud. , 50, 368–382.
Rigg, J. and A. Salamanca, 2015: The devil in the details: interpreting livelihood turbulence from a 25-year panel study from Thailand. Area, 47 (3), 296–304.
Rigi, H. and J.F. Warner, 2020: Two-level games on the trans-boundary river Indus: obstacles to cooperation. Water Policy, 22 (6), 972–990.
Riley, M., 2021: The New South Wales air quality alert system: a brief history. Aust. J. Emerg. Manag. , 36 (1), 21–24.
Riosmena, F., R. Kuhn and W.C. Jochem, 2017: Explaining the immigrant health advantage: self-selection and protection in health-related factors among five major national-origin immigrant groups in the United States. Demography, 54 (1), 175–200, doi:10.1007/s13524-016-0542-2.
Riosmena, F., R. Nawrotzki and L. Hunter, 2018: Climate migration at the height and end of the Great Mexican Emigration Era. Popul. Dev. Rev. , 44 (3), 455–488, doi:10.1111/padr.12158.
Rippin, H., et al., 2020: Disrupted food systems in the WHO European region – a threat or opportunity for healthy and sustainable food and nutrition?Food Sec. , 12 (4), 859–864, doi:10.1007/s12571-020-01079-y.
Ripple, W., et al., 2014: Commentary: Ruminants, climate change and climate policy. Nat. Clim. Change, 4 (1), 2–5, doi:10.1038/nclimate2081.
Ritchie, H., D. Reay and P. Higgins, 2018: Beyond calories: a holistic assessment of the global food system. Front. Sustain. Food Syst. , 2, doi:10.3389/fsufs.2018.00057.
Rivas, A.V., et al., 2018: Building Infestation Index for Aedes aegypti and occurrence of dengue fever in the municipality of Foz do Iguacu, Parana, Brazil, from 2001 to 2016. Rev. Soc. Bras. Med. Trop. , 51 (1), 71–76, doi:10.1590/0037-8682-0228-2017.
Roa, L., et al., 2020: Climate change: challenges and opportunities to scale up surgical, obstetric, and anaesthesia care globally. Lancet Planet. Health, 4 (11), E538–E543.
Robalino, J., J. Jiminez and A. Chacón, 2015: The effect of hydro-meteorological emergencies on internal migration. World Dev. , 67, 438–448.
Roberts, I. and E. Arnold, 2007: Policy at the crossroads: climate change and injury control. Inj. Prev. , 13 (4), 222–223.
Roberts, I. and M. Hillman, 2005: Climate change: the implications for policy on injury control and health promotion. Inj. Prev. , 11 (6), 326–329.
Roche, K.R., et al., 2020: Climate change and the opportunity cost of conflict. Proc. Natl. Acad. Sci. , 117 (4), 1935–1940.
Rocklöv, J. and R. Dubrow, 2020: Climate change: an enduring challenge for vector-borne disease prevention and control. Nat. Immunol. , 21 (5), 479–483.
Rocklöv, J., V. Huber, K. Bowen and R. Paul, 2021: Taking globally consistent health impact projections to the next level. Lancet Planet. Health. DOI: https://doi.org/10.1016/S2542-5196(21)00171-6
Rocklov, J., et al., 2019: Using big data to monitor the introduction and spread of Chikungunya, Europe, 2017. Emerg. Infect. Dis. , 25 (6), 1041–1049, doi:10.3201/eid2506.180138.
Roda Gracia, J., B. Schumann and A. Seidler, 2015: Climate variability and the occurrence of human Puumala hantavirus infections in Europe: a systematic review. Zoonoses Public Health, 62 (6), 465–478, doi:10.1111/zph.12175.
Rodrigues, M., P. Santana and A. Rocha, 2020: Statistical modelling of temperature-attributable deaths in Portuguese metropolitan areas under climate change: who is at risk?Atmosphere, 11 (2), doi:10.3390/atmos11020159.
Rodriguez-Llanes, J., S. Ranjan-Dash, A. Mukhopadhyay and D. Guha-Sapir, 2016: Looking upstream: enhancers of child nutritional status in post-flood rural settings. PeerJ, 4, doi:10.7717/peerj.1741.
Rogers, D.J., 2015: Dengue: recent past and future threats. Philos. Trans. R. Soc. Lond. B Biol. Sci. , 370 (1665), doi:10.1098/rstb.2013.0562.
Rohat, G., et al., 2019a: Projections of human exposure to dangerous heat in African cities under multiple socioeconomic and climate scenarios. Earths Future, 7 (5), 528–546, doi:10.1029/2018ef001020.
Rohat, G., et al., 2019b: Influence of changes in socioeconomic and climatic conditions on future heat-related health challenges in Europe. Glob. Planet. Change, 172, 45–59, doi:10.1016/j.gloplacha.2018.09.013.
Rohat, G., et al., 2019c: Characterizing the role of socioeconomic pathways in shaping future urban heat-related challenges. Sci. Total Environ. , 695, doi:10.1016/j.scitotenv.2019.133941.
Rojas-Rueda, D., et al., 2016: Health impacts of active transportation in Europe. PLoS ONE, 11 (3), doi:10.1371/journal.pone.0149990.
Roos, N., et al., 2021: Maternal and newborn health risks of climate change: a call for awareness and global action. Acta Obstet. Gynecol. Scand. , 100 (4), 566–570, doi:10.1111/aogs.14124.
Rosenberg, A., et al., 2018: Ambient temperature and age-related notified Campylobacter infection in Israel: a 12-year time series study. Environ. Res. , 164, 539–545, doi:10.1016/j.envres.2018.03.017.
Rosenbloom, D. and J. Markard, 2020: A COVID-19 recovery for climate. Science, 368 (6490), 447–447, doi:10.1126/science.abc4887.
Rosenstock, T., et al., 2019: A planetary health perspective on agroforestry in Sub-Saharan Africa. One Earth, 1 (3), 330–344, doi:10.1016/j.oneear.2019.10.017.
Roth, D., et al., 2019: Climates of urbanization: local experiences of water security, conflict and cooperation in peri-urban South-Asia. Clim. Policy, 19 (sup1), S78–S93.
Roth, G.A., et al., 2020: Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J. Am. Coll. Cardiol. , 76 (25), 2982–3021, doi:10.1016/j.jacc.2020.11.010.
Rozenberg, H., 2017: Climate change through a poverty lens. Nat. Clim. Change, 7 (4), 250–256.
Rüegger, S. and H. Bohnet, 2020: The link between forced migration and conflict. In: Environmental Conflicts, Migration and Governance, Bristol University Press, Bristol, pp. 177.
Rushton, S.P., et al., 2019: Climate, human behaviour or environment: individual-based modelling of Campylobacter seasonality and strategies to reduce disease burden. J. Transl. Med. , 17 (1), 34, doi:10.1186/s12967-019-1781-y.
Russo, S., A. F. Marchese, J. Sillmann and G. Imme, 2016: When will unusual heat waves become normal in a warming Africa?Environ. Res. Lett. , 11 (5), doi:10.1088/1748-9326/11/5/054016.
Russo, S., et al., 2019: Half a degree and rapid socioeconomic development matter for heatwave risk. Nat. Commun. , 10, doi:10.1038/s41467-018-08070-4.
Ruszkiewicz, J., et al., 2019: Brain diseases in changing climate. Environ. Res. , 177, doi:10.1016/j.envres.2019.108637.
Rüttinger, L., et al., 2015: A New Climate for Peace: Taking Action on Climate and Fragility Risks. Adelphi, Berlin/London/Washington/Paris.
Ruuhela, R., et al., 2021: Temperature-related mortality in Helsinki compared to its surrounding region over two decades, with special emphasis on intensive heatwaves. Atmosphere, 12 (1), doi:10.3390/atmos12010046.
Ryan, B., et al., 2015a: Identifying and describing the impact of cyclone, storm and flood related disasters on treatment management, care and exacerbations of non-communicable diseases and the implications for public health. PLoS Curr. , 7, doi:10.1371/currents.dis.62e9286d152de04799644dcca47d9288.
Ryan, S., C. Carlson, E. Mordecai and L. Johnson, 2019: Global expansion and redistribution of Aedes-borne virus transmission risk with climate change. PLoS Negl. Trop. Dis. , 13 (3), doi:10.1371/journal.pntd.0007213.
Ryan, S., C. Lippi and F. Zermoglio, 2020: Shifting transmission risk for malaria in Africa with climate change: a framework for planning and intervention. Malar. J. , 19 (1), doi:10.1186/s12936-020-03224-6.
Ryan, S.J., et al., 2015b: Mapping physiological suitability limits for malaria in Africa under climate change. Vector Borne Zoonotic Dis. , 15 (12), 718–725, doi:10.1089/vbz.2015.1822.
Sabate, J. and S. Soret, 2014: Sustainability of plant-based diets: back to the future. Am. J. Clin. Nutr. , 100, 476S–483S.
Saeed, F., C.F. Schleussner and M. Almazroui, 2021: From Paris to Makkah: heat stress risks for Muslim pilgrims at 1.5 degrees C and 2 degrees C. Environ. Res. Lett. , 16 (2), doi:10.1088/1748-9326/abd067.
Saha, S.K., 2016: Cyclone Aila, livelihood stress, and migration: empirical evidence from coastal Bangladesh. Disasters, doi:10.1111/disa.12214.
Salas, R. and A. Jha, 2019: Climate change threatens the achievement of effective universal healthcare. BMJ, 366, doi:10.1136/bmj.l5302.
Samir, K. and W. Lutz, 2017: The human core of the shared socioeconomic pathways: population scenarios by age, sex and level of education for all countries to 2100. Glob. Environ. Change Policy Dimens. , 42, 181–192, doi:10.1016/j.gloenvcha.2014.06.004.
Sampedro, J., et al., 2020: Health co-benefits and mitigation costs as per the Paris Agreement under different technological pathways for energy supply. Environ. Int. , 136, 1–12, doi:10.1016/j.envint.2020.105513.
Sangha, K.K., et al., 2018: An ecosystem services framework to evaluate Indigenous and local peoples’ connections with nature. Ecosyst. Serv. , 31, 111–125.
Santiago, E.C. and F. Rivas, 2012: Polychlorinated biphenyls in selected sites in Pasig River and Laguna Lake in the Philippines before and after a big flood event investigated under the UNU East Asia Regional POPs monitoring project. Bull. Environ. Contam. Toxicol. , 89 (2), 407–411, doi:10.1007/s00128-012-0677-9.
Sanz-Barbero, B., et al., 2018: Heat wave and the risk of intimate partner violence. Sci. Total Environ. , 644, 413–419, doi:10.1016/j.scitotenv.2018.06.368.
Sapkota, A., et al., 2020: Association between changes in timing of spring onset and asthma hospitalization in Maryland. JAMA Network Open, 3 (7). DOI:10.1001/jamanetworkopen.2020.7551
Sarkar, S., V. Gangare, P. Singh and R. Dhiman, 2019: Shift in potential malaria transmission areas in India, using the fuzzy-based climate suitability malaria transmission (FCSMT) model under changing climatic conditions. Int. J. Environ. Res. Public Health, 16 (18), doi:10.3390/ijerph16183474.
Sattler, D.N., et al., 2020: Climate change in Tonga: risk perception and behavioral adaptation. In: Managing Climate Change Adaptation in the Pacific Region, Springer, Cham, pp. 273–292.
Sattler, D.N., A. Whippy, J.M. Graham and J. Johnson, 2018: A psychological model of climate change adaptation: influence of resource loss, posttraumatic growth, norms, and risk perception following Cyclone Winston in Fiji. In: Climate Change Impacts and Adaptation Strategies for Coastal Communities, Springer, Dordrecht, pp. 427–443.
Sawas, A., M. Workman and N. Mirumachi, 2018: Climate Change, Low-carbon Transitions and Security. Grantham Institute Briefing paper, Vol. 25. Imperial College, London.
Scarpa, G., et al., 2021: Developing an online food composition database for an Indigenous population in south-western Uganda. Public Health Nutr. , 24 (9), 2455–2464, doi:10.1017/s1368980021001397.
Scasny, M., E. Massetti, J. Melichar and S. Carrara, 2015: Quantifying the ancillary benefits of the representative concentration pathways on air quality in Europe. Environ. Resour. Econ. , 62 (2), 383–415, doi:10.1007/s10640-015-9969-y.
Schachtel, A., J.A. Dyer and M.D. Boos, 2021: Climate change and pediatric skin health. Int. J. Womens Dermatol. , 7 (1), 85–90, doi:10.1016/j.ijwd.2020.07.006.
Schaferhoff, M., et al., 2019: Trends in global health financing. BMJ, 365, doi:10.1136/bmj.l2185.
Scheelbeek, P., et al., 2021: The effects on public health of climate change adaptation responses: a systematic review of evidence from low- and middle-income countries. Environ. Res. Lett. , 16 (7), doi:10.1088/1748-9326/ac092c.
Scheffran, J., et al., 2012: Disentangling the climate-conflict nexus: empirical and theoretical assessment of vulnerabilities and pathways. Rev. Eur. Stud. , 4 (5), 13.
Scheidel, A., et al., 2020: Environmental conflicts and defenders: a global overview. Glob. Environ. Change, 63, 102104.
Schinasi, L.H., T. Benmarhnia and A.J. De Roos, 2018: Modification of the association between high ambient temperature and health by urban microclimate indicators: a systematic review and meta-analysis. Environ. Res. , 161, 168–180, doi:10.1016/j.envres.2017.11.004.
Schipper, E., et al., 2021: Turbulent transformation: abrupt societal disruption and climate resilient development. Clim. Dev. , 13 (6), 467–474.
Schipper, E.L.F., 2020: Maladaptation: when adaptation to climate change goes very wrong. One Earth, 3 (4), 409–414, doi:10.1016/j.oneear.2020.09.014.
Schleussner, C.-F., J.F. Donges, R.V. Donner and H.J. Schellnhuber, 2016: Armed-conflict risks enhanced by climate-related disasters in ethnically fractionalized countries. Proc. Natl. Acad. Sci. , 113 (33), 9216–9221.
Schneider, A., et al., 2020: Impact of meteorological parameters on suicide mortality rates: a case-crossover analysis in Southern Germany (1990–2006). Sci. Total Environ. , 707, doi:10.1016/j.scitotenv.2019.136053.
Schnell, J.L. and M.J. Prather, 2017: Co-occurrence of extremes in surface ozone, particulate matter, and temperature over eastern North America. Proc. Natl. Acad. Sci. U.S.A. , 114 (11), 2854–2859, doi:10.1073/pnas.1614453114.
Schramm, P., et al., 2020a: Climate change and health: local solutions to local challenges. Curr. Environ. Health Rep. , 7 (4), 363–370, doi:10.1007/s40572-020-00294-1.
Schramm, P., et al., 2020b: How indigenous communities are adapting to climate change: insights from the climate-ready tribes initiative. Health Aff. , 39 (12), 2153–2159, doi:10.1377/hlthaff.2020.00997.
Schucht, S., et al., 2015: Moving towards ambitious climate policies: Monetised health benefits from improved air quality could offset mitigation costs in Europe. Environ. Sci. Policy, 50, 252–269, doi:10.1016/j.envsci.2015.03.001.
Schumacher, K. A. and V. Shandas, 2019: Rescaling air quality management: an assessment of local air quality authorities in the United States. Air Soil Water Res. , 12, doi:10.1177/1178622119842125.
Schuster, C., J. Honold, S. Lauf and T. Lakes, 2017: Urban heat stress: novel survey suggests health and fitness as future avenue for research and adaptation strategies. Environ. Res. Lett. , 12, doi:10.1088/1748-9326/aa5f35.
Schutte, S., J. Vestby, J. Carling and H. Buhaug, 2021: Climatic conditions are weak predictors of asylum migration. Nat. Commun. , 12 (1), 2067, doi:10.1038/s41467-021-22255-4.
Schwartz, R., et al., 2015: The impact of Hurricane Sandy on the mental health of New York area residents. Am. J. Disaster Med. , 10 (4), 339–346.
Schwarz, L., et al., 2021: Spatial variation in the joint effect of extreme heat events and ozone on respiratory hospitalizations in California. Proc. Natl. Acad. Sci. U.S.A. , 118 (22), doi:10.1073/pnas.2023078118.
Schweitzer, M.D., et al., 2018: Lung health in era of climate change and dust storms. Environ. Res. , 163, 36–42, doi:10.1016/j.envres.2018.02.001.
Schwerdtle, P., K. Bowen and C. McMichael, 2018: The health impacts of climate-related migration. BMC Med. , 16 (1), 1–7.
Schwerdtle, P., et al., 2020: Health and migration in the context of a changing climate: a systematic literature assessment. Environ. Res. Lett. , 15 (10), doi:10.1088/1748-9326/ab9ece.
Schwingshackl, C., et al., 2021: Heat stress indicators in CMIP6: estimating future trends and exceedances of impact-relevant thresholds. Earths Future, 9 (3), doi:10.1029/2020ef001885.
Scortichini, M., et al., 2018: The inter-annual variability of heat-related mortality in nine European cities (1990–2010). Environ. Health, 17 (1), 66, doi:10.1186/s12940-018-0411-0.
Scott, A.A., D.W. Waugh and B. Zaitchik, 2018: Reduced Urban Heat Island intensity under warmer conditions. Environ. Res. Lett. , 13 (6), doi:10.1088/1748-9326/aabd6c.
Scott, C.A., et al., 2019: Water in the Hindu Kush Himalaya. In: The Hindu Kush Himalaya Assessment . Springer, Berlin Heidelberg, pp. 257–299.
Selby, J., 2019: Climate change and the Syrian civil war, Part II: the Jazira’s agrarian crisis. Geoforum, 101, 260–274.
Selby, J., O.S. Dahi, C. Frohlich and M. Hulme, 2017: Climate change and the Syrian civil war revisited. Polit. Geogr. , 60, 232–244, doi:10.1016/j.polgeo.2017.05.007.
Sellers, S. and K.L. Ebi, 2017: Climate change and health under the shared socioeconomic pathway framework. Int. J. Environ. Res. Public Health, 15 (1), doi:10.3390/ijerph15010003.
Semakula, H., et al., 2017: Prediction of future malaria hotspots under climate change in sub-Saharan Africa. Clim. Change, 143 (3-4), 415–428, doi:10.1007/s10584-017-1996-y.
Semenza, J., 2020: Cascading risks of waterborne diseases from climate change. Nat. Immunol. , 21 (5), 484–487, doi:10.1038/s41590-020-0631-7.
Semenza, J., 2021: Lateral public health: advancing systemic resilience to climate change. Lancet Reg. Health. DOI: https://doi.org/10.1016/j.lanepe.2021.100231
Semenza, J., et al., 2021: COVID-19 research priorities for non-pharmaceutical public health and social measures. Epidemiol. Infect. , 149, e87, doi:10.1017/s0950268821000716.
Semenza, J., et al., 2016: Determinants and drivers of infectious disease threat events in Europe. Emerg. Infect. Dis. , 22 (4), 581–589, doi:10.3201/eid2204.151073.
Semenza, J., et al., 2017: Environmental suitability of vibrio infections in a warming climate: an early warning system. Environ. Health Perspect. , 125 (10), doi:10.1289/ehp2198.
Semenza, J. and H. Zeller, 2014: Integrated surveillance for prevention and control of emerging vector-borne diseases in Europe. Euro Surveill. , 19 (13), 2–5, doi:10.2807/1560-7917.Es2014.19.13.20757.
Semenza, J.C., 2011: Lateral public health: a comprehensive approach to adaptation in urban environments. In: Climate Change Adaptation in Developed Nations: From Theory to Practice Advances in Global Research[Ford, J.D. and L. Berrang-Ford(eds.)]. Springer Science +Business Media, New York, NY, pp. 143–159.
Semenza, J.C. and K.L. Ebi, 2019: Climate change impact on migration, travel, travel destinations and the tourism industry. J. Travel Med. , 26 (5), doi:10.1093/jtm/taz026.
Semenza, J.C. and S. Paz, 2021: Climate change and infectious disease in Europe: impact, projection and adaptation. Lancet Reg. Health. https://doi.org/10.1016/j.lanepe.2021.100230
Sen, A., 2001: Development as Freedom. Oxford University Press, Oxford.
Sera, F., et al., 2019: How urban characteristics affect vulnerability to heat and cold: a multi-country analysis. Int. J. Epidemiol. , 48 (4), 1101–1112, doi:10.1093/ije/dyz008.
Sera, F., et al., 2020: Air conditioning and heat-related mortality A multi-country longitudinal study. Epidemiology, 31 (6), 779–787, doi:10.1097/ede.0000000000001241.
Serdeczny, O., et al., 2017: Climate change impacts in Sub-Saharan Africa: from physical changes to their social repercussions. Reg. Environ. Change, 17 (6), 1585–1600, doi:10.1007/s10113-015-0910-2.
Shaffer, R., et al., 2019: Improving and expanding estimates of the global burden of disease due to environmental health risk factors. Environ. Health Perspect. , 127 (10), doi:10.1289/ehp5496.
Shaffie, A., 2021: International institutions and global governance on climate change. Chapter 20. In: Global Climate Change and Human Health: from Science to Practice[Lemery, J., K. Knowlton and C. Sorensen(eds.)]. John Wiley & Sons, Hoboken NJ.
Shair-Rosenfield, S. and R.M. Wood, 2017: Governing well after war: how improving female representation prolongs post-conflict peace. J. Polit. , 79 (3), 995–1009.
Shaman, J. and M. Lipsitch, 2013: The El Nino-Southern Oscillation (ENSO)-pandemic Influenza connection: coincident or causal?Proc. Natl. Acad. Sci. U.S.A. , 110, 3689–3691, doi:10.1073/pnas.1107485109.
Shayegh, S., 2017: Outward migration may alter population dynamics and income inequality. Nat. Clim. Change, 7, 828–828.
Shekhar, M., et al., 2018: Effects of climate change on occurrence of aflatoxin and its impacts on maize in India. Int. J. Curr. Microbiol. App. Sci, 7 (6), 109–116.
Sheller, M., 2018: Theorising mobility justice. Tempo Soc. , 30 (2), 17–34, doi:10.11606/0103-2070.ts.2018.142763.
Sheng, R., et al., 2018: Does hot weather affect work-related injury? A case-crossover study in Guangzhou, China. Int. J. Hyg. Environ. Health, 221 (3), 423–428, doi:10.1016/j.ijheh.2018.01.005.
Sheridan, S. and M. Allen, 2018: Temporal trends in human vulnerability to excessive heat. Environ. Res. Lett. , 13, doi:10.1088/1748-9326/aab214.
Sherpa, A., T. Koottatep, C. Zurbrugg and G. Cisse, 2014: Vulnerability and adaptability of sanitation systems to climate change. J. Water Clim. Change, 5 (4), 487–495, doi:10.2166/wcc.2014.003.
Shi, J., Z.Y. Chen, S.S. Ding and Y.Q. Lu, 2020: A hot blob eastward of New Zealand in December 2019. Atmosphere, 11 (12), doi:10.3390/atmos11121267.
Shih, D.H., T.W. Wu, W.X. Liu and P.Y. Shih, 2019: An Azure ACES early warning system for air quality index deteriorating. Int. J. Environ. Res. Public Health, 16 (23), doi:10.3390/ijerph16234679.
Shindell, D., G. Faluvegi, K. Seltzer and C. Shindell, 2018: Quantified, localized health benefits of accelerated carbon dioxide emissions reductions. Nat. Clim. Change, 8 (4), 291, doi:10.1038/s41558-018-0108-y.
Shooshtarian, S., P. Rajagopalan and A. Sagoo, 2018: A comprehensive review of thermal adaptive strategies in outdoor spaces. Sustain. Cities Soc. , 41, 647–665, doi:10.1016/j.scs.2018.06.005.
Shrestha, N., et al., 2020: The impact of COVID-19 on globalization. One Health, 100180, doi:10.1016/j.onehlt.2020.100180.
Shultz, J., C. Fugate and S. Galea, 2020: Cascading risks of COVID-19 resurgence during an active 2020 Atlantic hurricane season. JAMA, 324 (10), 935–936, doi:10.1001/jama.2020.15398.
Shultz, J.M., et al., 2018a: Risks, health consequences, and response challenges for small-island-based populations: observations from the 2017 Atlantic hurricane season. Disaster Med. Public Health Prep. , 1–13, doi:10.1017/dmp.2018.28.
Shultz, J.M., J. Russell and Z. Espinel, 2005: Epidemiology of tropical cyclones: the dynamics of disaster, disease, and development. Epidemiol. Rev. , 27, 21–35, doi:10.1093/epirev/mxi011.
Shultz, J.M., et al., 2018b: Mitigating tropical cyclone risks and health consequences: urgencies and innovations. Lancet Planet Health, 2 (3), e103–e104, doi:10.1016/s2542-5196(18)30021-4.
Shumake-Guillemot, J, et al., 2020: Technical Brief: Protecting Health from Hot Weather During the COVID-19 Pandemic. Global Heat Health Information Network, Geneva, https://ghhin.org/wp-content/uploads/technical-brief-COVID-and-Heat-finalv2-1.pdf. Accessed 2 September 2021 . (8 pp).
Siddiqi, A., 2019: In the Wake of Disaster: Islamists, the State and a Social Contract in Pakistan. Cambridge University Press, Cambridge, ISBN 978-1108597708.
Siders, A.R., I. Ajibade and D. Casagrande, 2021: Transformative potential of managed retreat as climate adaptation. Curr. Opin. Environ. Sustain. , 50, 272–280. Available at: https://www.sciencedirect.com/science/article/pii/S1877343521000798.
Sijbrandij, M., et al., 2020: The effect of psychological first aid training on knowledge and understanding about psychosocial support principles: a cluster-randomized controlled trial. Int. J. Environ. Res. Public Health, 17 (2), doi:10.3390/ijerph17020484.
Silva, F.D., A.M. dos Santos, G. Correa Rda and J. Caldas Ade, 2016a: Temporal relationship between rainfall, temperature and occurrence of dengue cases in Sao Luis, Maranhao, Brazil. Cien. Saude Colet. , 21 (2), 641–646, doi:10.1590/1413-81232015212.09592015.
Silva, M., A. Loureiro and G. Cardoso, 2016b: Social determinants of mental health: a review of the evidence. Eur. J. Psychiatry, 30 (4), 259–292.
Silva, R.A., et al., 2016c: The effect of future ambient air pollution on human premature mortality to 2100 using output from the ACCMIP model ensemble. Atmos. Chem. Phys. , 16 (15), 9847–9862, doi:10.5194/acp-16-9847-2016.
Silva, R.A., et al., 2017: Future global mortality from changes in air pollution attributable to climate change. Nat. Clim. Change, 7 (9), 647–651, doi:10.1038/nclimate3354.
Silveira, I.H., T.R. Cortes, B.F.A. de Oliveira and W.L. Junger, 2021a: Projections of excess cardiovascular mortality related to temperature under different climate change scenarios and regionalized climate model simulations in Brazilian cities. Environ. Res. , 197, 110995, doi:10.1016/j.envres.2021.110995.
Silveira, S., et al., 2021b: Chronic mental health sequelae of climate change extremes: a case study of the deadliest Californian wildfire. Int. J. Environ. Res. Public Health, 18 (4), doi:10.3390/ijerph18041487.
Singh, C., 2019: Migration as a driver of changing household structures: implications for local livelihoods and adaptation. Migr. Dev. , 8 (3), 301–319, doi:10.1080/21632324.2019.1589073.
Singh, C. and R. Basu, 2020: Moving in and out of vulnerability: Interrogating migration as an adaptation strategy along a rural-urban continuum in India. Geogr. J. , 186 (1), doi:10.1111/geoj.12328.
Singh, P.K. and H. Chudasama, 2021: Pathways for climate resilient development: human well-being within a safe and just space in the 21st century. Glob. Environ. Change, 68, 102277.
Sioui, M., 2019: Drought in the Yucatan: Maya perspectives on tradition, change, and adaptation. In: Drought Challenges: Policy Options for Developing Countries[Mapedza, E., D. Tsegai, M. Bruntrup and R. McLeman(eds.)]. Elsevier, Amsterdam.
Siraj, A., et al., 2014: Altitudinal changes in malaria incidence in highlands of Ethiopia and Colombia. Science, 343 (6175), 1154–1158, doi:10.1126/science.1244325.
Smith, A., et al., 2016: Health and environmental co-benefits and conflicts of actions to meet UK carbon targets. Clim. Policy, 16 (3), 253–283, doi:10.1080/14693062.2014.980212.
Smith, B.A. and A. Fazil, 2019: How will climate change impact microbial foodborne disease in Canada?Can. Commun. Dis. Rep. , 45 (4), 108–113, doi:10.14745/ccdr.v45i04a05.
Smith, C., K. Dupre, A. McEvoy and S. Kenny, 2021: Community perceptions and pro-environmental behavior: the mediating roles of social norms and climate change risk. Can. J. Behav. Sci. , 53 (2), 200–210, doi:10.1037/cbs0000229.
Smith, J., et al., 2017: Malaria early warning tool: linking inter-annual climate and malaria variability in northern Guadalcanal, Solomon Islands. Malar. J. , 16 (1), 472, doi:10.1186/s12936-017-2120-5.
Smith, K., et al., 2014: Human health: impacts, adaptation, and co-benefits. In: Climate Change 2014: Impacts, Adaptation, and Vulnerability, Pt a: Global and Sectoral Aspects, Cambridge University Press, Cambridge, UK, pp. 709–754.
Smith, M.R. and S.S. Myers, 2018: Impact of anthropogenic CO2 emissions on global human nutrition. Nat. Clim. Change, 8 (9), 834–839, doi:10.1038/s41558-018-0253-3.
Soebiyanto, R.P., et al., 2015: Associations between meteorological parameters and influenza activity in Berlin (Germany), Ljubljana (Slovenia), Castile and Leon (Spain) and Israeli districts. PLoS ONE, 10 (8), doi:10.1371/journal.pone.0134701.
Sohn, S., et al., 2019: ‘Pneumonia weather’: short-term effects of meteorological factors on emergency room visits due to pneumonia in Seoul, Korea. J. Prev. Med. Public. Health, 52 (2), 82–91, doi:10.3961/jpmph.18.232.
Song, G., et al., 2017: Dietary changes to mitigate climate change and benefit public health in China. Sci. Total Environ. , 577, 289–298, doi:10.1016/j.scitotenv.2016.10.184.
Sorensen, C., et al., 2018: Climate change and women’s health: impacts and opportunities in India. GeoHealth, 2 (10) 283-297.
Sorgho, R., et al., 2020: Climate change policies in 16 West African countries: a systematic review of adaptation with a focus on agriculture, food security, and nutrition. Int. J. Environ. Res. Public Health, 17 (23), doi:10.3390/ijerph17238897.
Sovacool, B., D. Del Rio and S. Griffiths, 2020: Contextualizing the Covid-19 pandemic for a carbon-constrained world: insights for sustainability transitions, energy justice, and research methodology. Energy Res. Soc. Sci. , 68, doi:10.1016/j.erss.2020.101701.
Sovacool, B.K., 2018: Bamboo beating Bandits: conflict, inequality, and vulnerability in the political ecology of climate change adaptation in Bangladesh. World Dev. , 102, 183–194, doi:10.1016/j.worlddev.2017.10.014.
Sovacool, K., B. LinnÈr and M. Goodsite, 2015: The political economy of climate adaptation. Nat. Clim. Change, 5, 616–618.
Sow, P., E. Marmer and J. Scheffran, 2016: Between the heat and the hardships. Climate change and mixed migration flows in Morocco. Migr. Dev. , 5 (2), 293–313.
Speakman, J.R., 2018: Obesity and thermoregulation. In: Thermoregulation: from Basic Neuroscience to Clinical Neurology, Pt I, Vol. 156(431–443). Elsevier, Amsterdam. doi:10.1016/b978-0-444-63912-7.00026-6.
Spearing, L.A. and K. M. Faust, 2020: Cascading system impacts of the 2018 Camp Fire in California: the interdependent provision of infrastructure services to displaced populations. Int. J. Disaster Risk Reduct. , 50, 101822, doi:10.1016/j.ijdrr.2020.101822.
Spencer, N. and M. A. Urquhart, 2018: Hurricane strikes and migration: evidence from storms in Central America and the Caribbean. Weather Clim. Soc. , 10 (3), 569–577, doi:10.1175/wcas-d-17-0057.1.
Spentzou, E., M.J. Cook and S. Emmitt, 2021: Low-energy cooling and ventilation refurbishments for buildings in a Mediterranean climate. Archit. Eng. Des. Manag. , doi:10.1080/17452007.2021.1926898.
Spilker, G., Q. Nguyen, V. Koubi and T. Bohmelt, 2020: Attitudes of urban residents towards environmental migration in Kenya and Vietnam. Nat. Clim. Change, 10 (7), 622–627, doi:10.1038/s41558-020-0805-1.
Springmann, M., et al., 2018a: Options for keeping the food system within environmental limits. Nature, 562 (7728), 519–525, doi:10.1038/s41586-018-0594-0.
Springmann, M., H.C.J. Godfray, M. Rayner and P. Scarborough, 2016a: Analysis and valuation of the health and climate change cobenefits of dietary change. J Proc. Natl. Acad. Sci. , 113 (15), 4146–4151, doi:10.1073/pnas.1523119113.
Springmann, M., et al., 2018b: Health-motivated taxes on red and processed meat: a modelling study on optimal tax levels and associated health impacts. PLoS ONE, 13 (11), doi:10.1371/journal.pone.0204139.
Springmann, M., et al., 2016b: Global and regional health effects of future food production under climate change: a modelling study. Lancet , 387 (10031), 1937–1946, doi:10.1016/s0140-6736(15)01156-3.
Springmann, M., et al., 2020: The healthiness and sustainability of national and global food based dietary guidelines: modelling study. BMJ, 370, doi:10.1136/bmj.m2322.
Springmann, M., et al., 2018c: Health and nutritional aspects of sustainable diet strategies and their association with environmental impacts: a global modelling analysis with country-level detail. Lancet Planet. Health, 2 (10), e451–e461, doi:10.1016/s2542-5196(18)30206-7.
Squire, S.A. and U. Ryan, 2017: Cryptosporidium and Giardia in Africa: current and future challenges. Parasit Vectors, 10 (1), 195, doi:10.1186/s13071-017-2111-y.
Staddon, C., et al., 2020: Water insecurity compounds the global coronavirus crisis. Water Int. , 45 (5), 416–422, doi:10.1080/02508060.2020.1769345.
Steentjes, K., et al., 2017: European Perceptions of Climate Change: Topline Findings of a Survey Conducted in Four European Countries in 2016. Cardiff University, Cardiff.
Steffen, W., et al., 2015: Planetary boundaries: guiding human development on a changing planet. Science, 347 (6223), doi:10.1126/science.1259855.
Stensgaard, A., et al., 2013: Large-scale determinants of intestinal schistosomiasis and intermediate host snail distribution across Africa: does climate matter?Acta Trop. , 128 (2), 378–390, doi:10.1016/j.actatropica .2011.11.010.
Stevens, S.E., et al., 2019: Precipitation and fatal motor vehicle crashes: continental analysis with high-resolution radar data. Bulletin of the American Meteorological Society, 100(8), 1453-1461.
Stewart-Sinclair, P., et al., 2020: Blue restoration – building confidence and overcoming barriers. Front. Mar. Sci. , 7, doi:10.3389/fmars.2020.541700.
Stewart, S., A.K. Keates, A. Redfern and J.J.V. McMurray, 2017: Seasonal variations in cardiovascular disease. Nat. Rev. Cardiol. , 14 (11), 654–664, doi:10.1038/nrcardio.2017.76.
Stojanov, R., B. Duži, I. Kelman, D. Němec, D. Procházka, 2016: Local perceptions of climate change impacts and migration patterns in Malé, Maldives. Geogr. J. , 183 (4), 370–385.
Stork, A., C. Travis and S. Halle, 2015: Gender-sensitivity in natural resource management in Côte d’Ivoire and Sudan. Peace Rev. , 27 (2), 147–155, doi:10.1080/10402659.2015.1037617.
Subiros, M., et al., 2019: Health monitoring during water scarcity in Mayotte, France, 2017. BMC Public Health, 19 (1), 288, doi:10.1186/s12889-019-6613-8.
Suckall, N., E. Fraser and P. Forster, 2017: Reduced migration under climate change: evidence from Malawi using an aspirations and capabilities framework. Clim. Dev. , 9 (4), 298–312, doi:10.1080/17565529.2016.1149441.
Suk, J.E., E.C. Vaughan, R.G. Cook and J.C. Semenza, 2020: Natural disasters and infectious disease in Europe: a literature review to identify cascading risk pathways. Eur. J. Public Health, 30 (5), 928–935, doi:10.1093/eurpub/ckz111.
Suliman, S., et al., 2019: Indigenous (im)mobilities in the Anthropocene. Mobilities, 14 (3), 298–318.
Sulser, T.B., et al., 2021: Disability-adjusted life years due to chronic and hidden hunger under food system evolution with climate change and adaptation to 2050. Am. J. Clin. Nutr. , 114 (2), 550–563, doi:10.1093/ajcn/nqab101.
Sultana, P., et al., 2019: Transforming local natural resource conflicts to cooperation in a changing climate: Bangladesh and Nepal lessons. Clim. Policy, 19 (sup1), S94–S106.
Sun, S., et al., 2019: Ambient temperature and markers of fetal growth: a retrospective observational study of 29 million US singleton births. Environmental health perspectives, 127 (6).DOI: https://doi.org/10.1289/EHP4648
Sun, Z., C. Chen, D. Xu and T. Li, 2018: Effects of ambient temperature on myocardial infarction: a systematic review and meta-analysis. Environ. Pollut. , 241, 1106–1114, doi:10.1016/j.envpol.2018.06.045.
Swinburn, B.A., et al., 2019: The global syndemic of obesity, undernutrition, and climate change: the Lancet commission report. Lancet , 393 (10173), 791–846, doi:10.1016/s0140-6736(18)32822-8.
Sylla, M.B., et al., 2018: Projected heat stress under 1.5 degrees C and 2 degrees C global warming scenarios creates unprecedented discomfort for humans in West Africa. Earths Future, 6 (7), 1029–1044, doi:10.1029/2018ef000873.
Tadgell, A., B. Doberstein and L. Mortsch, 2018: Principles for climate-related resettlement of informal settlements in less developed nations: a review of resettlement literature and institutional guidelines. Clim. Dev. , 10 (2), 102–115, doi:10.1080/17565529.2017.1291401.
Tadgell, A., M. Linda and D. Brent, 2017: Assessing the feasibility of resettlement as a climate change adaptation strategy for informal settlements in Metro Manila, Philippines. Int. J. Disaster Risk Reduct. , 22, 447–457, doi:10.1016/j.ijdrr.2017.01.005.
Tainio, M., et al., 2017: Mortality, greenhouse gas emissions and consumer cost impacts of combined diet and physical activity scenarios: a health impact assessment study. BMJ Open, 7 (2), e14199, doi:10.1136/bmjopen-2016-014199.
Takebayashi, H., 2018: A simple method to evaluate adaptation measures for urban heat island. Environments, 5 (6), doi:10.3390/environments5060070.
Talhaoui, A., et al., 2019: Association between malnutrition and cognitive impairment among Morocco’s older adults. Open J. Med. Psychol. , 8 (1), 1–14.
Talukder, M.R.R., et al., 2017: Drinking water salinity and risk of hypertension: a systematic review and meta-analysis. Arch. Environ. Occup. Health, 72 (3), 126–138, doi:10.1080/19338244.2016.1175413.
Tamerius, J.D., et al., 2013: Environmental predictors of seasonal influenza epidemics across temperate and tropical climates. PLoS Pathog. , 9 (3), doi:10.1371/journal.ppat.1003194.
Tamnes, R. and K. Offerdal, 2014: Geopolitics and Security in the Arctic: Regional Dynamics in a Global World. Routledge, New York, ISBN 978-1317801597.
Tänzler, D., N. Scherer and Adelphi, 2019: Guidelines for Conflict-sensitive Adaptation to Climate Change. Agency, G. E., Dessau-Roßlau.
Tayimlong, R.A., 2020: Fragility and insurgency as outcomes of underdevelopment of public infrastructure and socio-economic deprivation: the case of Boko Haram in the Lake Chad Basin. J. Peacebuild. Dev. 16 (2), 209-223.
Taylor, D., et al., 2016a: Environmental change and Rift Valley fever in eastern Africa: projecting beyond HEALTHY FUTURES. Geospat. Health, 11 (1 Suppl), 387, doi:10.4081/gh.2016.387.
Taylor, L., et al., 2016b: The impact of different environmental conditions on cognitive function: a focused review. Front. Physiol. , 6, doi:10.3389/fphys.2015.00372.
Taylor, R.G., et al., 2012: Ground water and climate change. Nat. Clim. Change, 3, 322, doi:10.1038/nclimate1744.
Taylor, S., 2020: Anxiety disorders, climate change, and the challenges ahead: introduction to the special issue. J Anxiety Disord. , 76.DOI: https://doi.org/10.1016/j.janxdis.2020.102313
Teixidor-Toneu, I., et al., 2021: Which plants matter? A comparison of academic and community assessments of plant value and conservation status in the Moroccan High Atlas. Ambio, doi:10.1007/s13280-021-01584-0.
Telford, A., 2018: A threat to climate-secure European futures? Exploring racial logics and climate-induced migration in US and EU climate security discourses. Geoforum, 96, 268–277.
Tennison, I., et al., 2021: Health care’s response to climate change: a carbon footprint assessment of the NHS in England. Lancet Planet. Health, 5 (2), E84–E92.
Terekhina, A., et al., 2021: The context of an emerging predation problem: Nenets reindeer herders and Arctic foxes in Yamal. Eur. J. Wildl. Res. , 67 (3), 13, doi:10.1007/s10344-021-01497-z.
Tesla, B., et al., 2018: Temperature drives Zika virus transmission: evidence from empirical and mathematical models. Proc. Royal Soc. B, 285 (1884), doi:10.1098/rspb.2018.0795.
Thaker, J., et al., 2015: The role of collective efficacy in climate change adaptation in India. Weather Clim. Soc. , 8 (1), 21–34, doi:10.1175/WCAS-D-14-00037.1.
Theisen, O.M., 2017: Climate change and violence: insights from political science. Curr. Clim. Change Rep. , 3 (4), 210–221.
Thema, J., et al., 2017: More than energy savings: quantifying the multiple impacts of energy efficiency in Europe. ECEEE 2017 Summer Study conerence proceedings, 29 May-03 June 2017, Presqu’ile de Giens, France, pp.1727–1736.
Theobald, S., et al., 2018: Implementation research: new imperatives and opportunities in global health. Lancet , 392 (10160), 2214–2228, doi:10.1016/S0140-6736(18)32205-0.
Thiam, S., et al., 2017: Association between childhood diarrhoeal incidence and climatic factors in urban and rural settings in the health district of Mbour, Senegal. Int. J. Environ. Res. Public Health, 14 (9), doi:10.3390/ijerph14091049.
Thiede, B. and C. Gray, 2020: Climate exposures and child undernutrition: evidence from Indonesia. Soc. Sci. Med. , 265, doi:10.1016/j.socscimed.2020.113298.
Thiery, W., et al., 2021: Age-dependent extreme event exposure. Science. Accepted 1 September 2021. https://spiral.imperial.ac.uk/bitstream/10044/1/92988/2/manuscript.pdf
Thomas, A., et al., 2020: Climate change and small island developing states. Annu. Rev. Environ. Resour. , 45, 6.1–6.27.
Thomas, A. and L. Benjamin, 2020: Non-economic loss and damage: lessons from displacement in the Caribbean. Clim. Policy, 20 (6), 715–728, doi:10.1080/14693062.2019.1640105.
Thompson, R., R. Hornigold, L. Page and T. Waite, 2018: Associations between high ambient temperatures and heat waves with mental health outcomes: a systematic review. Public Health, 161, 171–191, doi:10.1016/j.puhe.2018.06.008.
Thornton, R.L., et al., 2016: Evaluating strategies for reducing health disparities by addressing the social determinants of health. Health Aff. , 35 (8), 1416–1423.
Tian, H.Y., et al., 2016: Surface water areas significantly impacted 2014 dengue outbreaks in Guangzhou, China. Environ. Res. , 150, 299–305, doi:10.1016/j.envres.2016.05.039.
Tian, Y., et al., 2019: Association between temperature variability and daily hospital admissions for cause-specific cardiovascular disease in urban China: a national time-series study. PLoS Med. , 16, e1002738, doi:10.1371/journal.pmed.1002738.
Tigchelaar, M., D.S. Battisti and J.T. Spector, 2020: Work adaptations insufficient to address growing heat risk for US agricultural workers. Environ. Res. Lett. , 15 (9), doi:10.1088/1748-9326/ab86 f4.
Tiihonen, J., et al., 2017: The association of ambient temperature and violent crime. Sci. Rep. , 7 (1), 1–7, doi:10.1038/s41598-017-06720-z.
Tilman, D. and M. Clark, 2014: Global diets link environmental sustainability and human health. Nature, 515 (7528), 518–522, doi:10.1038/nature13959. http://www.nature.com/nature/journal/v515/n7528/abs/nature13959.html#supplementary-information.
Timler, K. and D. Sandy, 2020: Gardening in ashes: the possibilities and limitations of gardening to support indigenous health and well-being in the context of wildfires and colonialism. Int. J. Environ. Res. Public Health, 17 (9), doi:10.3390/ijerph17093273.
Timlin, U., et al., 2021: Living conditions and mental wellness in a changing climate and environment: focus on community voices and perceived environmental and adaptation factors in Greenland. Heliyon, 7 (4), e6862, doi:10.1016/j.heliyon.2021.e06862.
Timmerman, J., 2020: Building resilience through transboundary water resources management. In: The Palgrave Handbook of Climate Resilient Societies, Palgrave Macmillan, New York, pp. 1–19.
Timmerman, J., et al., 2017: Improving governance in transboundary cooperation in water and climate change adaptation. Water Policy, 19 (6), 1014–1029.
Tirado, M.C., 2017: Sustainable Diets for Healthy People and a Healthy Planet . United Nations System Standing Committee on Nutrition, Italy, Rome. Discussion paper.
Todd, N. and A.J. Valleron, 2015: Space-time Covariation of mortality with temperature: a systematic study of deaths in France, 1968–2009. Environ. Health Perspect. , 123 (7), 659–664, doi:10.1289/ehp.1307771.
Tompkins, A.M. and L. Caporaso, 2016a: Assessment of malaria transmission changes in Africa, due to the climate impact of land use change using Coupled Model Intercomparison Project Phase 5 earth system models. Geospat. Health, 11 (1 Suppl), 380, doi:10.4081/gh.2016.380.
Tompkins, A.M. and L. Caporaso, 2016b: Assessment of malaria transmission changes in Africa, due to the climate impact of land use change using Coupled Model Intercomparison Project Phase 5 earth system models. Geospat. Health, 11, doi:10.4081/gh.2016.380.
Tong, S., et al., 2016: Climate change, food, water and population health in China. Bull. World Health Organ. , 94 (10), 759–765, doi:10.2471/blt.15.167031.
Torres, J.M. and J.A. Casey, 2017: The centrality of social ties to climate migration and mental health. BMC Public Health, 17, 600–600, doi:10.1186/s12889-017-4508-0.
Tosun, J., A. Jordan and M. Maor, 2017: Governing climate change: the (dis)proportionality of policy responses. J. Environ. Policy Plan. , 19 (6), 596–598, doi:10.1080/1523908x.2017.1354451.
Tozier de la Poterie, A., et al., 2020: Managing multiple hazards: lessons from anticipatory humanitarian action for climate disasters during COVID-19. Clim. Dev. DOI: https://doi.org/10.1080/17565529.2021.1927659.
Trewin, B.J., et al., 2020: Urban landscape features influence the movement and distribution of the Australian container-inhabiting mosquito vectors Aedes aegypti (diptera: Culicidae) and Aedes notoscriptus (diptera: Culicidae). J. Med. Entomol. , 57 (2), 443–453, doi:10.1093/jme/tjz187.
Tschakert, P., et al., 2017: Climate change and loss, as if people mattered: values, places, and experiences. WIREs Clim. Change, 8 (5), e476–e476.
Tschakert, P., et al., 2019: One thousand ways to experience loss: a systematic analysis of climate-related intangible harm from around the world. Glob. Environ. Change Policy Dimens. , 55, 58–72, doi:10.1016/j.gloenvcha.2018.11.006.
Tshimanga, R.M., et al., 2021: An integrated information system of climate-water-migrations-conflicts nexus in the Congo basin. Sustainability, 13 (16), 9323.
Turco, M., N. Levin, N. Tessler and H. Saaroni, 2017: Recent changes and relations among drought, vegetation and wildfires in the eastern Mediterranean: the case of Israel. Glob. Planet. Change, 151, 28–35.
Turek-Hankins, L.L., et al., 2021: Climate change adaptation to extreme heat: a global systematic review of implemented action. Oxf. Open Clim. Change, 1 (1), 13, doi:10.1093/oxfclm/kgab005.
Turner, N. and K. Turner, 2008: “Where our women used to get the food”: cumulative effects and loss of ethnobotanical knowledge and practice; case study from coastal British Columbia. Botany, 86, 103-115..
Uboni, A., B. Ahman and J. Moen, 2020: Can management buffer pasture loss and fragmentation for Sami reindeer herding in Sweden?Pastor. Policy Pract. , 10 (1), doi:10.1186/s13570-020-00177-y.
Udas, B., et al., 2019: Basin level gendered vulnerabilities and adaptation: a case of Gandaki River Basin. Environ. Dev. , 31, 43–54.
Ulpiani, G., 2019: Water mist spray for outdoor cooling: a systematic review of technologies, methods and impacts. Appl. Energy, 254, doi:10.1016/j.apenergy.2019.113647.
UNDRR Asia-Pacific, 2020: COVID-19 Brief: Combating the Dual Challenges of Climate-related Disasters and COVID-19. United Nations Office for Disaster Risk Reduction, Bangkok, Thailand. 15 pp.UNEP, 2014: The Adaptation Gap Report 2014. United Nations Environment Programme (UNEP), Nairobi, Kenya.
UNEP, 2018: The Adaptation Gap Report 2018. United Nations Environment Programme (UNEP), Nairobi, Kenya, ISBN 978-9280737288.
UNEP, 2021: Adaptation Gap Report . Nairobi, https://www.unep.org/resources/adaptation-gap-report-2020. Last accessed 3 September 2021.
UNEP, European Union and Adelphi, 2019: Guidance Note and Tools to Address Climate-Fragility Risks. UNEP, Nairobi.
UNFCCC, 2017a: Human health and adaptation: understanding climate impacts on health and opportunities for action synthesis paper by the secretariat. In: Nairobi Work Programme on Impacts, Vulnerability and Adaptation to Climate Change. 03.03. Subsidiary Body for Scientific and Technological Advice, Bonn.
UNFCCC, 2017b: Opportunities and Options for Integrating Climate Change Adaptation with the Sustainable Development Goals and the Sendai Framework for Disaster Risk Reduction 2015–2030. Technical paper by the UNFCCC secretariat, Bonn.
UNICEF, 2021: The Climate Crisis is a Child Rights Crisis: Introducing the Children’s Climate Risk Index. UNICEF, New York.
UNICEF et al, 2021: Joint Child Malnutrition Estimates—Levels and Trends – 2021 Edition. United Nations Children’s Fund, New York.
UNICEF, WHO and WBG, 2019: United Nations Children’s Fund (UNICEF), World Health Organization, International Bank for Reconstruction and Development/The World Bank. Levels and Trends in Child Malnutrition: Key Findings of the 2019 Edition Joint Child Malnutrition Estimates. World Health Organization, Geneva.
United Nations Department of Economic and Social Affairs, Population Division 2019: World Population Prospects 2019. Department of Economic and social affairs: Population Division. United Nations, New York.
Ürge-Vorsatz, D., T. Herrero, K. Dubash and F. Lecocq, 2014: Measuring the co-benefits of climate change mitigation. Annu. Rev. Environ. Resour. , 39 (6), 549–582, doi:10.1146/annurev-environ-031312-125456.
Ürge-Vorsatz, D., et al., 2016: Measuring multiple impacts of low-carbon energy options in a green economy context. Appl. Energy, 179, 1409–1426, doi:10.1016/j.apenergy.2016.07.027.
U.S. Global Change Research Program, 2016: The Impacts of Climate Change on Human Health in the United States: a Scientific Assessment . U.S. Global Change Research Program, Washington, DC, doi:10.7930/J0R49NQX.
Vahmani, P., A.D. Jones and C.M. Patricola, 2019: Interacting implications of climate change, population dynamics, and urban heat mitigation for future exposure to heat extremes. Environ. Res. Lett. , 14 (8), doi:10.1088/1748-9326/ab28b0.
van den Hurk, B., et al., 2020: What Can COVID-19 Teach Us About Preparing for Climate Risks in Europe?UN Office for Disaster Risk Reduction, Geneva, 17 pp. https://climatestorylines.eu/wp-content/uploads/2020/12/Policy-Brief-Lessons-from-COVID.pdf. Last accessed 3 September 2021.
van der Geest, K., et al., 2020: Climate change, ecosystem services and migration in the Marshall Islands: are they related?Clim. Change, 16 (1), 109–127.
van der Linden, S., 2015: The social-psychological determinants of climate change risk perceptions: towards a comprehensive model. J. Environ. Psychol. , 41, 112–124, doi:10.1016/j.jenvp.2014.11.012.
van Dijk, M., T. Morley, M.L. Rau and Y. Saghai, 2021: A meta-analysis of projected global food demand and population at risk of hunger for the period 2010–2050. Nat. Food, 2 (7), 494–501, doi:10.1038/s43016-021-00322-9.
van Loenhout, J.A. F., et al., 2018: Heat and emergency room admissions in the Netherlands. BMC Public Health, 18 (1), 108, doi:10.1186/s12889-017-5021-1.
van Valkengoed, A. and L. Steg, 2019: Meta-analyses of factors motivating climate change adaptation behaviour. Nat. Clim. Change, 9 (2), 158, doi:10.1038/s41558-018-0371-y.
van Weezel, S., 2019: On climate and conflict: precipitation decline and communal conflict in Ethiopia and Kenya. J. Peace Res. , 56 (4), 514–528.
Vandyck, T., et al., 2018: Air quality co-benefits for human health and agriculture counterbalance costs to meet Paris Agreement pledges. Nat. Commun. , 9 (1), 4939, doi:10.1038/s41467-018-06885-9.
Vanos, J., D.J. Vecellio and T. Kjellstrom, 2019: Workplace heat exposure, health protection, and economic impacts: a case study in Canada. Am. J. Ind. Med. , 62 (12), 1024–1037, doi:10.1002/ajim.22966.
Vardoulakis, S., et al., 2014: Comparative assessment of the effects of climate change on heat- and cold-related mortality in the United Kingdom and Australia. Environ. Health Perspect. , 122 (12), 1285–1292, doi:10.1289/ehp.1307524.
Varghese, B.M., et al., 2019: The effects of ambient temperatures on the risk of work-related injuries and illnesses: evidence from Adelaide, Australia 2003–2013. Environmental research, 170, 101-109.
Varghese, B.M., et al., 2020: Heat-related injuries in Australian workplaces: perspectives from health and safety representatives. Saf. Sci, 126, doi:10.1016/j.ssci.2020.104651.
Varotsos, K.V., C. Giannakopoulos and M. Tombrou, 2019: Ozone-temperature relationship during the 2003 and 2014 heatwaves in Europe. Reg. Environ. Change, 19 (6), 1653–1665, doi:10.1007/s10113-019-01498-4.
Varquez, A.C.G., et al., 2020: Future increase in elderly heat-related mortality of a rapidly growing Asian megacity. Sci. Rep. , 10 (1), doi:10.1038/s41598-020-66288-z.
Vautard, R., et al., 2020: Human contribution to the record-breaking June and July 2019 heatwaves in Western Europe. Environ. Res. Lett. , 15 (9), doi:10.1088/1748-9326/aba3d4.
Velez-Valle, E.M., S. Echeverria and M. Santorelli, 2016: Type II diabetes emergency room visits associated with Hurricane Sandy in New Jersey: implications for preparedness. J. Environ. Health, 79 (2), 30–37.
Venugopal, R. and S. Yasir, 2017: The politics of natural disasters in protracted conflict: the 2014 flood in Kashmir. Oxf. Dev. Stud. , 45 (4), 424–442.
Venugopal, V., et al., 2021: Epidemiological evidence from south Indian working population-the heat exposures and health linkage. J. Expo. Sci. Environ. Epidemiol. , 31 (1), 177–186, doi:10.1038/s41370-020-00261-w.
Verhaeghe, C., E. Feltes and J. Stacey, 2017: Nagmwedizk’an Gwanes Gangu Ch’inidzed Ganexwilagh: the Fires Awakened Us. Tsilhqot’in National Government, Williams Lake, BC, Canada.
Veronis, L., B. Boyd, R. Obokata and B. Main, 2018: Environmental change and international migration: a review. In: Routledge Handbook of Environmental Displacement and Migration[McLeman, R. and F. Gemenne]. Routledge, London/New York.
Veronis, L. and R. McLeman, 2014: Environmental influences on African migration to Canada: focus group findings from Ottawa-Gatineau. Popul. Environ. , 36 (2), 234–251, doi:10.1007/s11111-014-0214-3.
Vestby, J., 2019: Climate variability and individual motivations for participating in political violence. Glob. Environ. Change, 56, 114–123.
Vicedo-Cabrera, A.M., et al., 2018a: Temperature-related mortality impacts under and beyond Paris Agreement climate change scenarios. Clim. Change, 150 (3), 391–402, doi:10.1007/s10584-018-2274-3.
Vicedo-Cabrera, A.M., et al., 2021: The burden of heat-related mortality attributable to recent human-induced climate change. Nat. Clim. Change, 11 (6), 492, doi:10.1038/s41558-021-01058-x.
Vicedo-Cabrera, A.M., et al., 2018b: A multi-country analysis on potential adaptive mechanisms to cold and heat in a changing climate. Environ. Int. , 111, 239–246, doi:10.1016/j.envint.2017.11.006.
Vidal, R., et al., 2014: Comparison of the carbon footprint of different patient diets in a Spanish hospital. J. Health Serv. Res. Policy, 20, doi:10.1177/1355819614553017.
Vik, M.H. and E. Carlquist, 2018: Measuring subjective well-being for policy purposes: the example of well-being indicators in the WHO “Health 2020” framework. Scand. J. Public Health, 46 (2), 279–286, doi:10.1177/1403494817724952.
Vinke, K., et al., 2017: Climatic risks and impacts in South Asia: extremes of water scarcity and excess. Reg. Environ. Change, 17 (6), 1569–1583.
Vins, H., J. Bell, S. Saha and J.J. Hess, 2015: The mental health outcomes of drought: a systematic review and causal process diagram. Int. J. Environ. Res. Public Health, 12 (10), 13251–13275, doi:10.3390/ijerph121013251.
Viswanathan, B. and K. Kumar, 2015: Weather, agriculture and rural migration: evidence from state and district level migration in India. Envir. Dev. Econ. , 20 (4), 469–492, doi:10.1017/s1355770x1500008x.
Vlaskamp, D., et al., 2020: First autochthonous human West Nile virus infections in the Netherlands, July to August 2020. Euro Surveill. , 25 (46), doi:10.2807/1560-7917.Es.2020.25.46.2001904.
von Schneidemesser, E., C. Driscoll, H.E. Rieder and L.D. Schiferl, 2020: How will air quality effects on human health, crops and ecosystems change in the future?Philos. Trans. Royal Soc. A Math. Phys. Eng. Sci. , 378 (2183), doi:10.1098/rsta.2019.0330.
von Uexkull, N. and H. Buhaug, 2021: Security implications of climate change: a decade of scientific progress. J. Peace Res. , 58 (1), 3–17, doi:10.1177/0022343320984210.
Von Uexkull, N., M. Croicu, H. Fjelde and H. Buhaug, 2016: Civil conflict sensitivity to growing-season drought. Proc. Natl. Acad. Sci. , 113 (44), 12391–12396.
Voordeckers, D., et al., 2021: Guidelines for passive control of traffic-related air pollution in street canyons: an overview for urban planning. Landsc. Urban Plan. , 207, doi:10.1016/j.landurbplan.2020.103980.
Vos T, et al., 2020: Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet , 396(10598), 1204-1222
Vratnica, Z., et al., 2017: Haemorrhagic fever with renal syndrome in Montenegro, 2004–14. Eur. J. Public. Health. , 27 (6), 1108–1110, doi:10.1093/eurpub/ckx149.
Waha, K., et al., 2017: Climate change impacts in the Middle East and Northern Africa (MENA) region and their implications for vulnerable population groups. Reg. Environ. Change, 17 (6), 1623–1638.
Waite, T.D., et al., 2017: The English national cohort study of flooding and health: cross-sectional analysis of mental health outcomes at year one. BMC Public Health, 17, doi:10.1186/s12889-016-4000-2.
Walch, C., 2018: Disaster risk reduction amidst armed conflict: informal institutions, rebel groups, and wartime political orders. Disasters, 42, S239–S264, doi:10.1111/disa.12309.
Walkepää, A., 2019: Syntesrapport - En sammanställning av fyra samebyars pilotprojekt med klimat- och sårbarhetsanalys samt handlingsplan för klimatanpassning (Synthesis report – A compilation of four Sami villages’ pilot projects with climate and vulnerability analysis and an action plan for climate adaptation). Giron-Kiruna, Sweden. Uppdragsnummer 12602183. https://www.sametinget.se/klimat/syntesrapport Last accessed 3 September 2021.
Wallace, L.M., et al., 2015: Social vulnerability as a predictor of mortality and disability: cross-country differences in the survey of health, aging, and retirement in Europe (SHARE). Aging Clin. Exp. Res. , 27 (3), 365–372.
Walton, D. and M.K. van Aalst, 2020: Climate-related Extreme Weather Events and COVID-19: A First Look at the Number of People Affected by Intersecting Disasters. IFRC, Geneva. 21 pp.
Wang, H., et al., 2017a: Global, regional, and national under-5 mortality, adult mortality, age-specific mortality, and life expectancy, 1970–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet , 390 (10100), 1084–1150, doi:10.1016/S0140-6736(17)31833-0.
Wang, H., et al., 2020a: Global age-sex-specific fertility, mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950–2019: a comprehensive demographic analysis for the Global Burden of Disease Study 2019. The Lancet, 396 (10258), 1160–1203, doi:10.1016/S0140-6736(20)30977-6.
Wang, J., N. Obradovich and S. Zheng, 2020b: A 43-million person investigation into weather extremes and expressed sentiment under climate change. One Earth, 2 (6), 568-577..
Wang, P., W.B. Goggins and E.Y.Y. Chan, 2018a: Associations of Salmonella hospitalizations with ambient temperature, humidity and rainfall in Hong Kong. Environ. Int. , 120, 223–230, doi:10.1016/j.envint.2018.08.014.
Wang, Q., et al., 2017: Environmental ambient temperature and blood pressure in adults: a systematic review and meta-analysis. Sci. Total Environ. , 575, 276–286, doi:10.1016/j.scitotenv.2016.10.019.
Wang, Q. et al. 2020: Independent and combined effects of heatwaves and PM2.5 on preterm birth in Guangzhou, China: A survival analysis. Environmental Health Perspectives. 128(1): 7006. DOI: 10.1289/EHP5117
Wang, X., et al., 2016: Ambient temperature and stroke occurrence: a systematic review and meta-analysis. Int. J. Environ. Res. Public Health, 13 (7), doi:10.3390/ijerph13070698.
Wang, X., E. Lavigne, H. Ouellette-kuntz and B. Chen, 2014: Acute impacts of extreme temperature exposure on emergency room admissions related to mental and behavior disorders in Toronto, Canada. J. Affect. Disord. , 155, 154–161, doi:10.1016/j.jad.2013.10.042.
Wang, X., et al., 2020c: Global burden of respiratory infections associated with seasonal influenza in children under 5 years in 2018: a systematic review and modelling study. Lancet Glob. Health, 8 (4), E497–E510, doi:10.1016/s2214-109x(19)30545-5.
Wang, X.L., et al., 2017c: Different responses of influenza epidemic to weather factors among Shanghai, Hong Kong, and British Columbia. Int. J. Biometeorol. , 61 (6), 1043–1053, doi:10.1007/s00484-016-1284-y.
Wang, Y., et al., 2018b: Accounting for adaptation and intensity in projecting heat wave-related mortality. Environ. Res. , 161, 464–471, doi:10.1016/j.envres.2017.11.049.
Wang, Z., Z. Han, L. Liu and S. Yu, 2021: Place attachment and household disaster preparedness: examining the mediation role of self-efficacy. Int. J. Environ. Res. Public Health, 18 (11), doi:10.3390/ijerph18115565.
Wangdi, K., A.C.A. Clements, T. Du and S.V. Nery, 2018: Spatial and temporal patterns of dengue infections in Timor-Leste, 2005–2013. Parasit Vectors, 11 (1), 9, doi:10.1186/s13071-017-2588-4.
Warner, K., 2018: Coordinated approaches to large-scale movements of people: contributions of the Paris Agreement and the Global Compacts for migration and on refugees. Popul. Environ. , 39 (4), 384–401, doi:10.1007/s11111-018-0299-1.
Watson, C.R., W. Matthew and S.T. Kirk, 2017: Public health preparedness funding: key programs and trends from 2001 to 2017. Am. J. Public Health, 107 (S2), S165–S167, doi:10.2105/ajph.2017.303963.
Watts, N., et al., 2017: The Lancet Countdown: tracking progress on health and climate change. Lancet , 389 (10074), 1151–1164, doi:10.1016/s0140-6736(16)32124-9.
Watts, N., et al., 2015: Health and climate change: policy responses to protect public health. Lancet , 386 (10006), 1861–1914, doi:10.1016/s0140-6736(15)60854-6.
Watts, N., et al., 2021: The 2020 report of the Lancet Countdown on health and climate change: responding to converging crises. Lancet , 397 (10269), 129–170, doi:10.1016/s0140-6736(20)32290-x.
Watts, N., et al., 2018a: The 2018 report of the Lancet Countdown on health and climate change: shaping the health of nations for centuries to come. Lancet , 392 (10163), 2479–2514.
Watts, N., et al., 2019: The 2019 report of The Lancet Countdown on health and climate change: ensuring that the health of a child born today is not defined by a changing climate. Lancet , 394 (10211), 1836–1878, doi:10.1016/s0140-6736(19)32596-6.
Watts, N., et al., 2018b: The Lancet Countdown on health and climate change: from 25 years of inaction to a global transformation for public health (vol 391, pg 581, 2017). Lancet , 391 (10120), 540–540.
Weber, E., 2017: Trade agreements, labour mobility and climate change in the Pacific Islands. Reg. Environ. Change, 17, 1089–1101.
Weber, T., et al., 2020: Analysis of compound climate extremes and exposed population in Africa under two different emission scenarios. Earths Future, 8 (9), doi:10.1029/2019ef001473.
Weible, C., et al., 2020: COVID-19 and the policy sciences: initial reactions and perspectives. Policy Sci. , 53 (2), 225–241, doi:10.1007/s11077-020-09381-4.
Weiler, F., 2019: Adaptation and health: are countries with more climate-sensitive health sectors more likely to receive adaptation aid?Int. J. Environ. Res. Public Health, 16 (8), doi:10.3390/ijerph16081353.
Weinberger, K.R., et al., 2017: Projected temperature-related deaths in ten large U.S. metropolitan areas under different climate change scenarios. Environ. Int. , 107, 196–204, doi:10.1016/j.envint.2017.07.006.
Weinberger, K.R., et al., 2018a: Projected changes in temperature-related morbidity and mortality in Southern New England. Epidemiology, 29 (4), 473–481, doi:10.1097/ede.0000000000000825.
Weinberger, K.R., A. Zanobetti, J. Schwartz and G.A. Wellenius, 2018b: Effectiveness of National Weather Service heat alerts in preventing mortality in 20 US cities. Environ. Int. , 116, 30–38, doi:10.1016/j.envint.2018.03.028.
Weisent, J., W. Seaver, A. Odoi and B. Rohrbach, 2014: The importance of climatic factors and outliers in predicting regional monthly campylobacteriosis risk in Georgia, USA. Int. J. Biometeorol. , 58 (9), 1865–1878, doi:10.1007/s00484-014-0788-6.
Weitensfelder, L. and H. Moshammer, 2020: Evidence of adaptation to increasing temperatures. Int. J. Environ. Res. Public Health, 17 (1), doi:10.3390/ijerph17010097.
Wells, M.L., et al., 2020: Future HAB science: directions and challenges in a changing climate. Harmful Algae, 91, 101632, doi:10.1016/j.hal.2019.101632.
Wells, M.L., et al., 2015: Harmful algal blooms and climate change: learning from the past and present to forecast the future. Harmful Algae, 49, 68–93, doi:10.1016/j.hal.2015.07.009.
Weyant, C., et al., 2018: Anticipated burden and mitigation of carbon-dioxide-induced nutritional deficiencies and related diseases: a simulation modeling study. PLoS Med. , 15 (7), e1002586, doi:10.1371/journal.pmed.1002586.
Whaley, A.L., 2009: Trauma among survivors of hurricane Katrina: considerations and recommendations for mental health care. J. Loss Trauma. , 14 (6), 459–476, doi:10.1080/15325020902925480.
Wheeler, N. and N. Watts, 2018: Climate change: from science to practice. Curr. Environ. Health Rep. , 5 (1), 170–178, doi:10.1007/s40572-018-0187-y.
Whitmee, S., et al., 2015: Safeguarding human health in the Anthropocene epoch: report of The Rockefeller Foundation-Lancet Commission on planetary health. Lancet , 386 (10007), 1973–2028, doi:10.1016/s0140-6736(15)60901-1.
WHO. and International Water Association, 2009: Water Safety Plan Manual: Step-by-step Risk Management for Drinking-water Suppliers. [Who (ed.)].Geneva, Switzerland, https://apps.who.int/iris/handle/10665/75141.
WHO, 1946: Preamble to the Constitution of WHO as Adopted by the International Health Conference, New York, 19 June – 22 July 1946; Signed on 22 July 1946 by the Representatives of 61 States and Entered into Force on 7 April 1948. Official Records of WHO, New York. 100 pp.
WHO, 2013: Protecting Health from Climate Change: Vulnerability and Adaptation Assessment . WHO, Geneva.
WHO, 2014: Quantitative Risk Assessment of the effects of Climate Change on Selected Causes of Death, 2030s and 2050s. WHO, Geneva.
WHO, 2015a: Operational Framework for Building Climate Resilient Health Systems. World Health Organization, Geneva.
WHO, 2015b: Climate and Health Country Profiles – 2015 a Global Overview. WHO, Geneva. 24 pp.
WHO, 2015c: Reducing Global Health Risks Through Mitigation of Short Lived Climate Pollutants, 1–121. WHO, Geneva.
WHO., 2016a: Sanitation Safety Planning: Manual for Safe Use and Disposal of Wastewater, Greywater and Excreta. WHO, Geneva, https://www.who.int/water_sanitation_health/publications/ssp-manual/en/.
WHO, 2016b: World Health Statistics 2016, Chapter 6 Sustainable development goals health and health related targets. WHO, Geneva. https://www.who.int/gho/publications/world_health_statistics/2016/EN_WHS2016_Chapter6.pdf. Last accessed 3 September 2021.
WHO., 2018a: COP24 Special Report on Health and Climate Change. WHO, Geneva.
WHO, 2018b: WHO Estimates of the Global Burden of Foodborne Diseases. World Health Organization, https://apps.who.int/iris/bitstream/handle/10665/199350/9789241565165_eng.pdf.. Last accessed 3 September 2021.
WHO, 2018c: WASH and Health Working Together: a ‘How-to’ Guide for Neglected Tropical Disease Programmes. WHO, Geneva.
WHO., 2019a: The WHO Special Initiative for Mental Health (2019–2023): Universal Health Coverage for Mental health. WHO, Geneva.
WHO, 2019b: WHO Health and Climate Change Survey Report: Tracking Global Progress. World Health Organization, Geneva.
WHO, 2020a: Who Guidance for Climate Resilient and Environmentally Sustainable Health Care Facilities. World Health Organization, Geneva.
WHO, 2020b: WHO Manifesto for a Healthy Recovery from COVID-19: Prescriptions and Actionables for a Healthy and Green Recovery. [Who (ed.)]. https://www.who.int/publications/i/item/who-manifesto-healthy-recovery-covid19. Last accessed 3 September 2021.
WHO, 2020c: Joint Child Malnutrition Estimates. WHO, Geneva.
WHO, 2021a: Stronger Collaboration for an Equitable and Resilient Recovery Towards the Health-Related Sustainable Development Goals: 2021 Progress Report on the Global Action Plan for Healthy Lives and Well-Being for All. WHO, Geneva.
WHO, 2021b: Universal Health Coverage (UHC). WHO, Geneva.
WHO, 2021c: World Health Statistics 2021: Monitoring Health for the SDGs, Sustainable Development Goals. WHO, Geneva.
Whyte, K., 2018: Critical investigations of resilience: a brief introduction to indigenous environmental studies & sciences. Daedalus, 147 (2), 136–147, doi:10.1162/DAED_a_00497.
Wickramage, K., et al., 2018: Migration and health: a global public health research priority. BMC Public Health, 18, doi:10.1186/s12889-018-5932-5.
Wiederkehr, C., M. Beckmann and K. Hermans, 2018: Environmental change, adaptation strategies and the relevance of migration in Sub-Saharan drylands. Environ. Res. Lett. , 13 (11).DOI: https://doi.org/10.1088/1748-9326/aae6de. Last accessed 3 September 2021
Wiegel, H., I. Boas and J. Warner, 2019: A mobilities perspective on migration in the context of environmental change. Wiley Interdiscip. Rev. Clim. Change, 10 (6), e610.
Wilder, J., et al., 2017: Polar bear attacks on humans: implications of a changing climate. Wildl. Soc. Bull. , 41 (3), 537–547, doi:10.1002/wsb.783.
Willett, W., et al., 2019: Food in the Anthropocene: the EAT-Lancet Commission on healthy diets from sustainable food systems. Lancet , 393 (10170), 447–492, doi:10.1016/s0140-6736(18)31788-4.
Willi, Y., G. Nischik, D. Braunschweiger and M. Putz, 2020: Responding to the COVID-19 crisis: transformative governance in Switzerland. Tijdschr. Econ. Soc. Geogr. , 111 (3), 302–317, doi:10.1111/tesg.12439.
Williams, L., 2018: Climate change, colonialism, and women’s well-being in Canada: what is to be done?Can. J. Public Health, 109 (2), 268–271, doi:10.17269/s41997-018-0031-z.
Williams, M.L., et al., 2018: The Lancet Countdown on health benefits from the UK Climate Change Act: a modelling study for Great Britain. Lancet Planet. Health, 2 (5), e202–e213, doi:10.1016/s2542-5196(18)30067-6.
Williams, M.N., S.R. Hill and J. Spicer, 2015a: Will Climate Change Increase or Decrease Suicide Rates? The Differing Effects of Geographical, Seasonal, and Irregular Variation in Temperature on Suicide Incidence. Springer, Netherlands, 1–10.
Williams, M.S., et al., 2015b: Temporal patterns of Campylobacter contamination on chicken and their relationship to campylobacteriosis cases in the United States. Int. J. Food Microbiol. , 208, 114–121, doi:10.1016/j.ijfoodmicro.2015.05.018.
Williams, S., et al., 2020: Workers’ health and safety in the heat: current practice in Australian workplaces. Policy Pract. Health Saf. , 18 (2), 67–79, doi:10.1080/14773996.2020.1765610.
Williamson, C., et al., 2017: Climate change-induced increases in precipitation are reducing the potential for solar ultraviolet radiation to inactivate pathogens in surface waters. Sci. Rep. , 7, doi:10.1038/s41598-017-13392-2.
Wilmsen, B. and M. Webber, 2015: What can we learn from the practice of development-forced displacement and resettlement for organised resettlements in response to climate change?Geoforum, 58, 76–85.
Winkler, R.L. and R. M. D., 2021: Amenities or disamenities? Estimating the impacts of extreme heat and wildfire on domestic US migration. Popul. Environ. , 42 (4), 622–648, doi:10.1007/s11111-020-00364-4.
Winne, J.D. and G. Peersman, 2019: The impact of food prices on conflict revisited. J. Bus. Econ. Stat. , 39 (2), 1–14.
Winsemius, H., et al., 2018: Disaster risk, climate change, and poverty: assessing the global exposure of poor people to floods and droughts. Envir. Dev. Econ. , 23 (3), 328–348, doi:10.1017/s1355770x17000444.
Wischnath, G. and H. Buhaug, 2014: Rice or riots: on food production and conflict severity across India. Polit. Geogr. , 43, 6–15, doi:10.1016/j.polgeo.2014.07.004.
Witmer, F.D., et al., 2017: Subnational violent conflict forecasts for sub-Saharan Africa, 2015–65, using climate-sensitive models. J. Peace Res. , 54 (2), 175–192.
Witt, C., et al., 2015: The effects of climate change on patients with chronic lung disease. Dtsch. Arztebl. Online, doi:10.3238/arztebl.2015.0878.
Wondmagegn, B., et al., 2019: What do we know about the healthcare costs of extreme heat exposure? A comprehensive literature review. Sci. Total Environ. , 657, 608–618, doi:10.1016/j.scitotenv.2018.11.479.
Wood, R.M. and T.M. Wright, 2016: Responding to catastrophe: repression dynamics following rapid-onset natural disasters. J. Confl. Resolut. , 60 (8), 1446–1472.
Woodcock, J., et al., 2018: Development of the Impacts of Cycling Tool (ICT): A modelling study and web tool for evaluating health and environmental impacts of cycling uptake. PLoS Med. , 15 (7), e1002622, doi:10.1371/journal.pmed.1002622.
Woodward, A., et al., 2019: Population health impacts of China’s climate change policies. Environ. Res. , 175, 178–185, doi:10.1016/j.envres.2019.05.020.
Woodward, A.J. and J.M. Samet, 2018: Climate change, hurricanes, and health. Am. J. Public Health, 108 (1), 33–35, doi:10.2105/ajph.2017.304197.
World Bank., 2021: Global Economic Prospects, June 2021. World Bank, Washington DC, ISBN 978-1464816659.
World Bank,, 2021: Indigenous Peoples. World Bank, Washington, DC. https://www.worldbank.org/en/topic/indigenouspeoples#1. Last accessed 3 September 2021.
Wouters, H., et al., 2017: Heat stress increase under climate change twice as large in cities as in rural areas: a study for a densely populated midlatitude maritime region. Geophys. Res. Lett. , 44 (17), 8997–9007, doi:10.1002/2017gl074889.
Wrathall, D. and N. Suckall, 2016: Labour migration amidst ecological change. Migr. Dev. , 5 (2), 314–329.
Wright, C., et al., 2021: A transdisciplinary approach to address climate change adaptation for human health and well-being in Africa. Int. J. Environ. Res. Public Health, 18 (8), doi:10.3390/ijerph18084258.
Wright, N., et al., 2020: Health emergency and disaster risk management: five years into implementation of the Sendai framework. Int. J. Disaster Risk Sci. , 11 (2), 206–217, doi:10.1007/s13753-020-00274-x.
Wu, F., et al., 2011: Climate change impacts on mycotoxin risks in US maize. World Mycotoxin J. , 4 (1), 79–93, doi:10.3920/wmj2010.1246.
Wu, J., M. Yunus, P.K. Streatfield and M. Emch, 2014: Association of climate variability and childhood diarrhoeal disease in rural Bangladesh, 2000–2006. Epidemiol. Infect. , 142 (9), 1859–1868, doi:10.1017/s095026881300277x.
Xiang, J., et al., 2018: Impact of meteorological factors on hemorrhagic fever with renal syndrome in 19 cities in China, 2005–2014. Sci. Total Environ. , 636, 1249–1256, doi:10.1016/j.scitotenv.2018.04.407.
Xiang, J.J., P. Bi, D. Pisaniello and A. Hansen, 2014: Health impacts of workplace heat exposure: an epidemiological review. Ind. Health, 52 (2), 91–101, doi:10.2486/indhealth.2012-0145.
Xiao, H., et al., 2014: Animal reservoir, natural and socioeconomic variations and the transmission of hemorrhagic fever with renal syndrome in Chenzhou, China, 2006–2010. PLoS Negl. Trop. Dis. , 8 (1), e2615, doi:10.1371/journal.pntd.0002615.
Xie, Y., et al., 2018: Co-benefits of climate mitigation on air quality and human health in Asian countries. Environ. Int. , 119, 309–318, doi:10.1016/j.envint.2018.07.008.
Xiong, J., et al., 2020: Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J. Affect. Disord. , 277, 55–64, doi:10.1016/j.jad.2020.08.001.
Xu, C., et al., 2020: Future of the human climate niche. Proc. Natl. Acad. Sci. , 117, 201910114, doi:10.1073/pnas.1910114117.
Xu, Y.Z., W.D. Yang and J.Z. Wang, 2017: Air quality early-warning system for cities in China. Atmos. Environ. , 148, 239–257, doi:10.1016/j.atmosenv.2016.10.046.
Xu, Z., et al., 2019a: Spatiotemporal patterns and climatic drivers of severe dengue in Thailand. Sci. Total Environ. , 656, 889–901, doi:10.1016/j.scitotenv.2018.11.395.
Xu, Z., et al., 2014: The impact of heat waves on children’s health: a systematic review. Int. J. Biometeorol. , 58 (2), 239–247, doi:10.1007/s00484-013-0655-x.
Xu, Z., et al., 2019b: Heatwaves and diabetes in Brisbane, Australia: a population-based retrospective cohort study. Int. J. Epidemiol. , 48 (4), 1091–1100.
le Xuan, T.T., P. Van Hau, T. do Thu and T.T. do Toan, 2014: Estimates of meteorological variability in association with dengue cases in a coastal city in northern Vietnam: an ecological study. Glob. Health Action, 7, 23119, doi:10.3402/gha.v7.23119.
Yactayo, S., et al., 2016: Epidemiology of Chikungunya in the Americas. J. Infect. Dis. , 214 (suppl 5), S441–S445, doi:10.1093/infdis/jiw390.
Yamana, T.K., A. Bomblies and E.A.B. Eltahir, 2016: Climate change unlikely to increase malaria burden in West Africa. Nat. Clim. Change, 6, 1009–1013.
Yan, X., et al., 2018: Effects of early-life malnutrition on neurodevelopment and neuropsychiatric disorders and the potential mechanisms. Prog. Neuropsychopharmacol. Biol. Psychiatry, 83, 64–75.
Yang, G. and R. Bergquist, 2018: Potential impact of climate change on schistosomiasis: a global assessment attempt. Trop. Med. Infect. Dis. , 3 (4), doi:10.3390/tropicalmed3040117.
Yang, J., et al., 2019: Heatwave and mortality in 31 major Chinese cities: definition, vulnerability and implications. Sci. Total Environ. , 649, 695–702, doi:10.1016/j.scitotenv.2018.08.332.
Yang, J., et al., 2016: The effect of ambient temperature on diabetes mortality in China: a multi-city time series study. Sci. Total Environ. , 543 (Pt A), 75–82, doi:10.1016/j.scitotenv.2015.11.014.
Yang, J., et al., 2021: Projecting heat-related excess mortality under climate change scenarios in China. Nat. Commun. , 12 (1), doi:10.1038/s41467-021-21305-1.
Yang, Z. and J. Wang, 2017: A new air quality monitoring and early warning system: air quality assessment and air pollutant concentration prediction. Environ. Res. , 158, 105–117, doi:10.1016/j.envres.2017.06.002.
Yasjukevich, V.V., I.O. Popov, S.N. Titkina and N.V. Yasjukevich, 2018: The vulnerability of subjects of the Russian Federation in relation to the distribution of the main vectors of Ixodes tick-borne borelliosis and tick-borne encephalitis in the expected climate change. Probl. Ecol. Monit. Ecosyst. Model. , xix (4), 8–28.
Yeargin, S.W., et al., 2019: Epidemiology of exertional heat illnesses in national collegiate athletic association athletes during the 2009–2010 through 2014–2015 academic years. J. Athl. Train. , 54 (1), 55–63, doi:10.4085/1062-6050-504-17.
Yeni, F. and H. Alpas, 2017: Vulnerability of global food production to extreme climatic events. Food Res. Int. , 96, 27–39, doi:10.1016/j.foodres.2017.03.020.
Yin, Q., et al., 2019: Mapping the increased minimum mortality temperatures in the context of global climate change. Nat. Commun. , 10, doi:10.1038/s41467-019-12663-y.
Yoo, E.H., et al., 2021: Association between extreme temperatures and emergency room visits related to mental disorders: a multi-region time-series study in New York, USA. Sci. Total Environ. https://doi.org/10.1016/j.scitotenv.2021.148246
Yorifuji, T., et al., 2017: Prenatal exposure to outdoor air pollution and child behavioral problems at school age in Japan. Environ. Int. , 99, 192–198, doi:10.1016/j.envint.2016.11.016.
Younan, D., et al., 2018: Longitudinal analysis of particulate air pollutants and adolescent delinquent behavior in Southern California. J. Abnorm. Child Psychol. , 46 (6), 1283–1293.
Young, H.S., et al., 2017: Interacting effects of land use and climate on rodent-borne pathogens in central Kenya. Philos. Trans. Royal Soc. B Biol. Sci. , 372 (1722), doi:10.1098/rstb.2016.0116.
Young, I., B.A. Smith and A. Fazil, 2015: A systematic review and meta-analysis of the effects of extreme weather events and other weather-related variables on Cryptosporidium and Giardia in fresh surface waters. J. Water Health, 13 (1), 1–17, doi:10.2166/wh.2014.079.
Youssouf, H., et al., 2014: Non-accidental health impacts of wildfire smoke. Int. J. Environ. Res. Public Health, 11 (11), 11772–11804, doi:10.3390/ijerph111111772.
Yuan, L., K. Shin and S. Managi, 2018: Subjective well-being and environmental quality: the impact of air pollution and green coverage in China. Ecol. Econ. , 153, 124–138, doi:10.1016/j.ecolecon.2018.04.033.
Yun, J., et al., 2016: Association between the ambient temperature and the occurrence of human Salmonella and Campylobacter infections. Sci Rep, 6, 28442, doi:10.1038/srep28442.
Zadnik, V., et al., 2020: Impact of COVID-19 on cancer diagnosis and management in Slovenia – preliminary results. Radiol. Oncol. , 54 (3), 329–334, doi:10.2478/raon-2020-0048.
Zaitchik, B.F., 2019: Climate and health across Africa. In: Oxford Research Encyclopedia, Climate Science. Oxford University Press, Oxford. doi:10.1093/acrefore/9780190228620.013.555.
Zander, K., C. Richerzhagen and S. Garnett, 2019: Human mobility intentions in response to heat in urban South East Asia. Glob. Environ. Change Hum. Policy Dimens. , 56, 18–28, doi:10.1016/j.gloenvcha.2019.03.004.
Zavaleta-Cortijo, C., et al., 2020: Climate change and COVID-19: reinforcing Indigenous food systems. Lancet Planet. Health, 4 (9), E381–E382, doi:10.1016/s2542-5196(20)30173-x.
Zavaleta, C., et al., 2018: Multiple non-climatic drivers of food insecurity reinforce climate change maladaptation trajectories among Peruvian Indigenous Shawi in the Amazon. PLoS ONE, 13 (10), doi:10.1371/journal.pone.0205714.
Zeng, J., C. Lu and Q.H. Deng, 2017: Prenatal exposure to diurnal temperature variation and early childhood pneumonia. J. Therm. Biol. , 65, 105–112, doi:10.1016/j.jtherbio.2017.02.012.
Zhang, B., G. Li, Y. Ma and X. Pan, 2018a: Projection of temperature-related mortality due to cardiovascular disease in Beijing under different climate change, population, and adaptation scenarios. Environ. Res. , 162, 152–159, doi:10.1016/j.envres.2017.12.027.
Zhang, J., et al., 2020a: The effects of elevated carbon dioxide concentration and mental workload on task performance in an enclosed environmental chamber. Build. Environ. , 178, 106938, doi:10.1016/j.buildenv.2020.106938.
Zhang, N., et al., 2019a: The impact of the 2016 flood event in Anhui Province, China on infectious diarrhea disease: an interrupted time-series study. Environ. Int. , 127, 801–809, doi:10.1016/j.envint.2019.03.063.
Zhang, Y., S. Isukapalli, L. Bielory and P. Georgopoulos, 2013: Bayesian analysis of climate change effects on observed and projected airborne levels of birch pollen. Atmos. Environ. , 68, 64–73, doi:10.1016/j.atmosenv.2012.11.028.
Zhang, Y., et al., 2017a: Co-benefits of global, domestic, and sectoral greenhouse gas mitigation for US air quality and human health in 2050. Environ. Res. Lett. , 12 (11), doi:10.1088/1748-9326/aa8f76.
Zhang, Y., C. Yu and L. Wang, 2017b: Temperature exposure during pregnancy and birth outcomes: an updated systematic review of epidemiological evidence. Environ. Pollut. , 225, 700–712, doi:10.1016/j.envpol.2017.02.066.
Zhang, Y.Q., M.J. Peng, L. Wang and C.H. Yu, 2018b: Association of diurnal temperature range with daily mortality in England and Wales: a nationwide time-series study. Sci. Total Environ. , 619, 291–300, doi:10.1016/j.scitotenv.2017.11.056.
Zhang, Y.Q., et al., 2019b: Socio-geographic disparity in cardiorespiratory mortality burden attributable to ambient temperature in the United States. Environ. Sci. Pollut. Res. , 26 (1), 694–705, doi:10.1007/s11356-018-3653-z.
Zhang, Z., T. Xue and X. Jin, 2020b: Effects of meteorological conditions and air pollution on COVID-19 transmission: evidence from 219 Chinese cities. Sci. Total Environ. , 741, 140244, doi:10.1016/j.scitotenv.2020.140244.
Zhao, L., et al., 2021: Global multi-model projections of local urban climates. Nat. Clim. Change, 11 (2), doi:10.1038/s41558-020-00958-8.
Zhao, N., G. Cao, J.K. Vanos and D.J. Vecellio, 2018a: The effects of synoptic weather on influenza infection incidences: a retrospective study utilizing digital disease surveillance. Int. J. Biometeorol. , 62 (1), 69–84, doi:10.1007/s00484-017-1306-4.
Zhao, Q., et al., 2019: Temperature variability and hospitalization for ischaemic heart disease in Brazil: a nationwide case-crossover study during 2000–2015. Sci. Total Environ. , 664, 707–712, doi:10.1016/j.scitotenv.2019.02.066.
Zhao, T., et al., 2018b: Ambient ozone exposure and mental health: a systematic review of epidemiological studies. Environ. Res. , 165, 459–472, doi:10.1016/j.envres.2018.04.015.
Zhao, X., et al., 2014: Japanese encephalitis risk and contextual risk factors in southwest China: a Bayesian hierarchical spatial and spatiotemporal analysis. Int. J. Environ. Res. Public Health, 11 (4), 4201–4217, doi:10.3390/ijerph110404201.
Zheng, X.R., et al., 2021: Preconceptional and prenatal exposure to diurnal temperature variation increases the risk of childhood pneumonia. BMC Pediatr. , 21 (1), doi:10.1186/s12887-021-02643-x.
Zhong, S., et al., 2020: Assessing the effectiveness and pathways of planned shelters in protecting mental health of flood victims in China. Environ. Res. Lett. DOI: https://doi.org/10.1088/1748-9326/abc446.
Zhong, S., et al., 2018: The long-term physical and psychological health impacts of flooding: a systematic mapping. Sci. Total Environ. , 626, 165–194, doi:10.1016/j.scitotenv.2018.01.041.
Zhu, C., et al., 2018: Carbon dioxide (CO2) levels this century will alter the protein, micronutrients, and vitamin content of rice grains with potential health consequences for the poorest rice-dependent countries. Sci. Adv. , 4 (5), eaaq1012, doi:10.1126/sciadv.aaq1012.
Zickgraf, 2019: Keeping people in place: political factors of (Im)mobility and climate change. Soc. Sci. , 8, 228, doi:10.3390/socsci8080228.
Zickgraf, C., 2018: Immobility[McLeman, R. and F. Gemenne (eds.)]. Routledge, London.
Zickgraf, C., et al., 2016: The Impact of Vulnerability and Resilience to Environmental Changes on Mobility Patterns in West Africa. World Bank, Washington, DC.
Ziegler, U., et al., 2020: West Nile virus epidemic in Germany triggered by epizootic emergence, 2019. Viruses, 12 (4), doi:10.3390/v12040448.
Zilbermint, M., 2020: Diabetes and climate change. J. Commun. Hosp. Intern. Med. Perspect. , 10 (5), 409–412, doi:10.1080/20009666.2020.1791027.
Zinsstag, J., et al., 2018: Climate change and One Health. FEMS Microbiol. Lett. , 365 (11), doi:10.1093/femsle/fny085.
Ziska, L.H., 2020: An overview of rising CO2 and climatic change on aeroallergens and allergic diseases. Allergy, Asthma & Immunology Research12 (5). DOI: 10.4168/aair.2020.12.5.771
Ziska, L.H., et al., 2019: Temperature-related changes in airborne allergenic pollen abundance and seasonality across the northern hemisphere: a retrospective data analysis. Lancet Planet. Health, 3 (3), e124–e131, doi:10.1016/s2542-5196(19)30015-4.
Zorrilla, C.D., 2017: The view from Puerto Rico — Hurricane Maria and its aftermath. N. Engl. J. Med. , 377 (19), 1801–1803, doi:10.1056/NEJMp1713196.
Zuvela-Aloise, M., R. Koch, S. Buchholz and B. Fruh, 2016: Modelling the potential of green and blue infrastructure to reduce urban heat load in the city of Vienna. Clim. Change, 135 (3-4), 425–438, doi:10.1007/s10584-016-1596-2.
1 In this Report, the following summary terms are used to describe the available evidence: limited, medium, or robust; and for the degree of agreement: low, medium, or high. A level of confidence is expressed using five qualifiers: very low, low, medium, high, and very high, and typeset in italics, e.g., medium confidence. For a given evidence and agreement statement, different confidence levels can be assigned, but increasing levels of evidence and degrees of agreement are correlated with increasing confidence.
2 In this Report, the following terms have been used to indicate the assessed likelihood of an outcome or a result: Virtually certain 99–100% probability, Very likely 90–100%, Likely 66–100%, About as likely as not 33–66%, Unlikely 0–33%, Very unlikely 0–10%, and Exceptionally unlikely 0–1%. Additional terms (Extremely likely : 95–100%, More likely than not > 50–100%, and Extremely unlikely 0–5%) may also be used when appropriate. Assessed likelihood is typeset in italics, e.g., very likely ). This Report also uses the term ‘likely range’ to indicate that the assessed likelihood of an outcome lies within the 17–83% probability range.
Table of Contents
7.1.1 Major Health-Related Statements in AR51048
7.1.2 Major Statements About Migration and Conflict in AR51048
7.1.3 Important Developments Since AR51048
7.1.4 Interpretation of ‘Health and Well-Being’ Used in This Chapter 1049
7.1.5 Towards Socioecological Perspectives on Health, Well-Being, and Loss and Damage 1049
7.1.6 Developments Relevant to Tracking and Assessing Climate Change Impacts on Health 1049
Box 7.1 | Indigenous Peoples’ Health and Well-Being in a Changing Climate 1054
7.1.8 Visual Guide to this Chapter 1059
7.2. Observed Impacts of Climate Change on Health, Well-Being, Migration and Conflict 1059
7.2.1 Observed Impacts on Health and Well-Being 1059
Box 7.2 | The Global Burden of Climate-Sensitive Health Outcomes Assessed in this Chapter 1060
7.2.2 Observed Impacts on Communicable Diseases 1062
Box 7.3 | Cascading Risk Pathways Linking Waterborne Disease to Climate Hazards 1065
Cross-Chapter Box COVID | COVID-191067
7.2.3 Observed Impacts on Non-communicable Diseases 1071
7.2.4 Observed Impacts on Other Climate-Sensitive Health Outcomes 1072
7.2.5 Observed Impacts on Mental Health and Well-Being 1076
7.2.6 Observed Impacts on Migration 1079
Cross-Chapter Box MIGRATE | Climate-Related Migration 1080
Box 7.4 | Gender Dimensions of Climate-Related Migration 1085
7.2.7 Observed Impacts of Climate on Conflict 1086
7.3 Projected Future Risks under Climate Change 1089
7.3.1 Projected Future Risks for Health and Well-Being 1089
7.3.2 Migration and Displacement in a Changing Climate 1099
7.3.3 Climate Change and Future Risks of Conflict 1102
7.4 Adaptation to Key Risks and Climate Resilient Development Pathways 1102
7.4.1 Adaptation Solution Space for Health and Well-Being 1103
7.4.2 Adaptation Strategies, Policies and Interventions 1105
7.4.3 Enabling Conditions and Constraints for Health Adaptation 1115
7.4.4 Migration and Adaptation in the Context of Climate Change 1116
7.4.5 Adaptation Solutions for Reducing Conflict Risks 1118
7.4.6 Climate Resilient Development Pathways 1119
FAQ 7.1 | How will climate change affect physical and mental health and well-being?1126
FAQ 7.2 | Will climate change lead to wide-scale forced migration and involuntary displacement?1128
FAQ 7.3 | Will climate change increase the potential for violent conflict?1128